Last Updated on November 20, 2025 by Ugurkan Demir
Ewing sarcoma is a very aggressive cancer. It mainly affects the bones and soft tissues of kids and teens.
It’s the second most common bone tumor in young people. The average age when it’s found is 15 years old.
This rare cancer needs quick and skilled treatment to have the best results.
Knowing the important details about Ewing tumor is key. This includes where it’s found, how it’s staged, if it can spread, and its overall outlook. This knowledge is important for both patients and doctors.

Ewing tumor is a very aggressive cancer that starts in bones or soft tissues. It often hits children and young adults. Finding it early and treating it fast is key because it can spread quickly.
Ewing sarcoma is a malignant cancer because it can grow into other tissues and spread. It belongs to the Ewing family of tumors, sharing genetic traits. The disease is caused by specific genetic changes that lead to cancer growth.
It’s important to tell Ewing sarcoma apart from other cancers or conditions for the right treatment. Ewing sarcoma is often mixed up with other small, round, blue-cell tumors. But, it can be told apart by certain genetic and immunohistochemical markers. The EWS-FLI1 fusion gene, from a t(11;22) chromosomal translocation, is a key sign of Ewing sarcoma, found in about 85% of cases.
Ewing sarcoma mainly hits kids and young adults, mostly between 10 and 20 years old. It’s less common in adults over 30. More boys than girls get Ewing sarcoma. It can happen in any ethnic group, but Caucasians are more likely to get it.
| Age Group | Incidence Rate | Relative Frequency |
| 0-9 years | Low | Less common |
| 10-20 years | High | Most common |
| 21-30 years | Moderate | Less frequent |
| >30 years | Low | Rare |
The table above shows how Ewing sarcoma affects different age groups. It’s most common in the young.
Understanding Ewing sarcoma’s biology is key to finding effective treatments. It has unique genetic and molecular traits that set it apart from other cancers.
The exact cell type where Ewing sarcoma starts is a topic of ongoing research. Yet, it’s thought to involve nonrandom gene rearrangements creating specific fusion genes. These genetic changes are vital for the disease’s growth and spread.
Studies point to mesenchymal stem cells or other early cell types as possible origins. The exact process is being studied, but it’s clear genetics are central.
Ewing sarcoma is marked by specific genetic translocations. The most common is the EWSR1 gene on chromosome 22 fusing with the FLI1 gene on chromosome 11. This creates the EWS/FLI1 fusion protein, an abnormal transcription factor that promotes tumor growth.
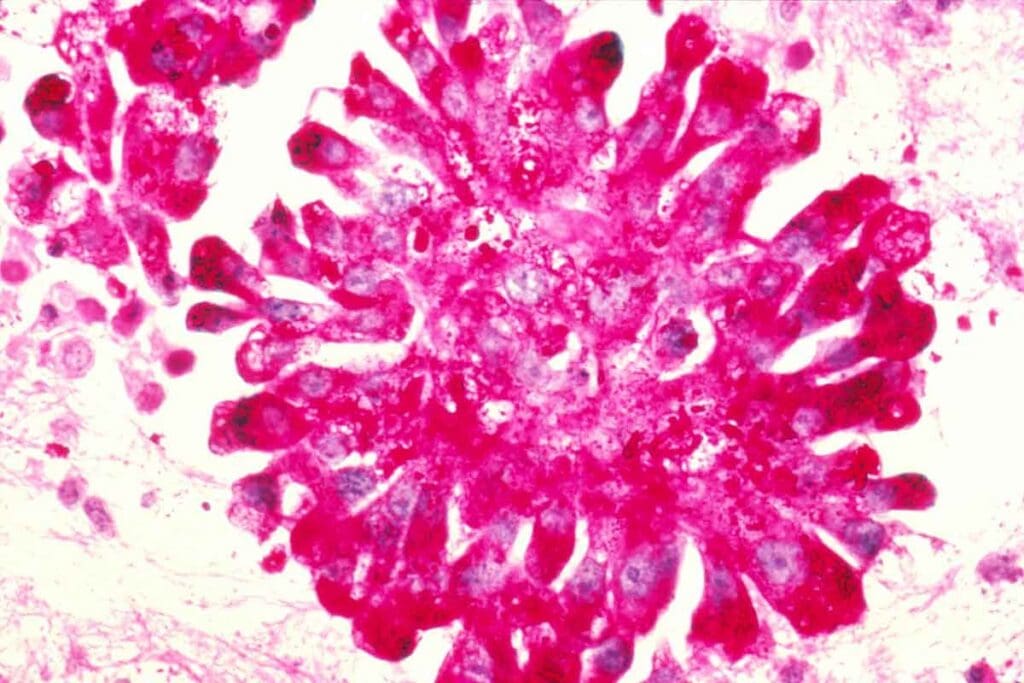
Ewing sarcoma is known for its pathological features, like small, round, blue-staining cells under the microscope. The tumor cells also show specific cellular markers, like CD99. This marker is used in pathology to confirm Ewing sarcoma.
“The diagnosis of Ewing sarcoma relies heavily on the identification of characteristic genetic translocations and the expression of specific cellular markers.” – Expert in Oncology
The presence of these markers and the tumor’s look help tell Ewing sarcoma apart from other cancers. Knowing these features is vital for accurate diagnosis and treatment planning.
Knowing where Ewing tumors usually show up is key for doctors to plan treatment. Ewing sarcoma is a very aggressive tumor that can appear in different bones and soft tissues.
Ewing sarcoma often happens in long bones, like the pelvis, femur, and ribs. The pelvis is a common spot, but it’s tricky to diagnose because of its complex shape. The femur, being a long bone, is also a common place for Ewing sarcoma, needing quick and strong treatment.
The chest wall is another area where Ewing sarcoma can show up, often affecting the ribs. This can cause a lot of problems because of its closeness to important parts. Other bones, like the humerus, tibia, and fibula, can also get affected, but less often.
Ewing sarcoma can also happen in soft tissues, known as extraskeletal Ewing sarcoma. These tumors can pop up in different soft tissue spots, like the trunk, limbs, and retroperitoneum. Treating extraskeletal Ewing sarcoma is different from treating bone tumors.
A top oncologist said, “The variety in Ewing tumor locations shows we need a detailed diagnosis and treatment plans.” This shows how complex and varied Ewing sarcoma is, making it vital to know its usual places.
Ewing sarcoma symptoms vary based on the tumor’s location. Patients often feel pain, stiffness, or swelling in the affected area.
Pain and swelling are common symptoms of Ewing sarcoma. The pain can be constant or come and go. It may get worse over time. Swelling happens as the tumor grows, making the area look bigger.
Table: Common Symptoms of Ewing Sarcoma by Location
| Location | Common Symptoms |
| Pelvis | Pain in the hip or lower back, swelling, limited mobility |
| Chest Wall | Pain or swelling in the chest, difficulty breathing |
| Long Bones (e.g., Femur) | Pain, swelling, limited mobility of the affected limb |
Symptoms of Ewing sarcoma change based on where the tumor is. For example, chest wall tumors can cause breathing problems. Pelvic tumors might lead to hip or lower back pain.
Some patients with Ewing sarcoma also have systemic symptoms. These include fever, weight loss, and feeling very tired. These signs can mean the disease is more advanced and are important for understanding the prognosis.
Knowing how Ewing sarcoma presents and its symptoms is key for early diagnosis and treatment. The symptoms help doctors decide on the best course of action and can affect how well a patient does.
Diagnosing Ewing Sarcoma needs a comprehensive approach. This includes imaging modalities, biopsy techniques, and molecular testing. These steps help confirm the diagnosis accurately.
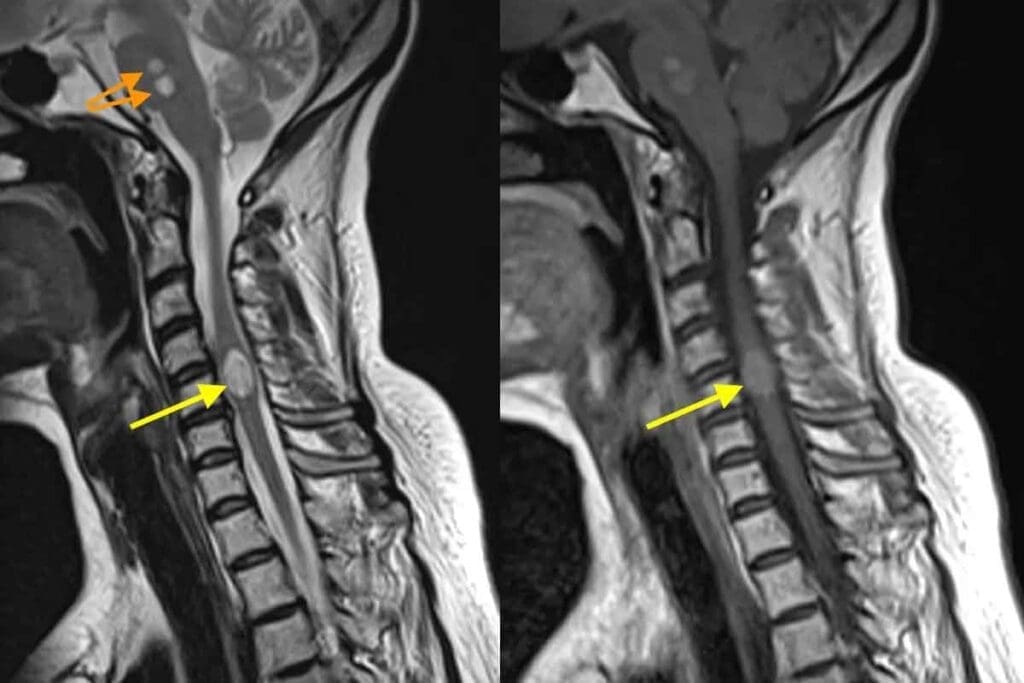
Imaging studies are key in diagnosing Ewing Sarcoma. MRI and CT scans help see how big the tumor is and if it has spread. MRI is great for checking soft tissue and how the tumor affects nearby areas.
A biopsy is vital for a clear diagnosis. Core needle or incisional biopsies are used to get tissue samples. Looking at these samples under a microscope helps spot Ewing Sarcoma’s unique small, round, blue cells.
Molecular testing is key to confirm the diagnosis. Tests like fluorescence in situ hybridization (FISH) and reverse transcription-polymerase chain reaction (RT-PCR) find specific genetic changes. These changes are linked to Ewing Sarcoma, like the EWS-FLI1 fusion.
Using all these diagnostic methods ensures a precise and quick diagnosis. This is essential for planning the best treatment.
The staging of Ewing sarcoma is key in figuring out how far the disease has spread. It helps doctors decide on the best treatment. Staging systems sort the disease into two main types: localized or metastatic.
The TNM classification is a common way to stage Ewing sarcoma. It looks at the tumor’s size and spread (T), nearby lymph nodes (N), and if it has gone to distant places (M).
TNM Staging Components:
Ewing sarcoma is divided into two main types: localized and metastatic. Localized disease is mostly in one place or has spread a little. Metastatic disease has spread to other parts of the body.
| Disease Category | Description |
| Localized | Disease mostly in one place or has spread a little. |
| Metastatic | Disease has spread to other parts of the body. |
Risk stratification in Ewing sarcoma looks at how far the disease has spread, tumor size, and patient age. This helps doctors choose the right treatment intensity for each patient. It aims to improve treatment outcomes.
Knowing how to stage and risk stratify Ewing sarcoma is vital. It helps doctors plan better treatments. It also helps patients understand their chances of recovery.
It’s important to know how Ewing sarcoma spreads to other parts of the body. This knowledge helps doctors plan better treatments. When cancer moves from its first place to other areas, it’s called metastatic Ewing sarcoma.
About 25% of patients have metastasis when they first get diagnosed. When this happens can vary. Some people have it right away, while others get it later, during or after treatment.
The cancer often goes to the lungs, bones, or bone marrow. These places are where it usually spreads. The lungs are a common spot because of their blood flow and how Ewing sarcoma cells tend to settle there.
Doctors use different ways to find metastasis in Ewing sarcoma. They look at images from CT scans, MRI, and PET scans. But, the best way to confirm it is through biopsy and looking at tissue under a microscope.
Micrometastatic disease means there are tiny cancer cells that have spread but can’t be seen yet. It’s hard to deal with these tiny cells. Doctors usually use chemotherapy to try to get rid of them before they grow into bigger problems.
Handling metastatic Ewing sarcoma needs a team effort. This includes chemotherapy, radiation, and sometimes surgery. Knowing how the cancer spreads helps doctors make treatment plans that fit each patient’s needs.
The stage of the disease is key in choosing the best treatment for Ewing sarcoma. Doctors create a treatment plan that fits the patient’s disease stage, health, and needs.
Multimodal therapy is the main treatment for Ewing sarcoma. It combines chemotherapy, surgery, and radiotherapy for the best results. This approach helps control both local and systemic disease well.
Patients with localized Ewing sarcoma usually get intense chemotherapy first. Then, they might have surgery and/or radiotherapy to control the disease. The goal is to get rid of the disease completely and prevent it from coming back.
Dealing with metastatic Ewing sarcoma is tougher. It often means using stronger chemotherapy. Doctors might also use local treatments to help with symptoms and control disease at specific spots.
There’s always new research into better treatments for Ewing sarcoma. This includes targeted therapies, immunotherapies, and other new treatments. They aim to make treatments more effective and less harmful.
Targeted therapies and immunotherapies are exciting areas of research. They could offer new options for treating Ewing sarcoma.
The outlook for Ewing’s sarcoma depends on several important factors. Knowing these factors helps doctors choose the best treatment and predict how well a patient will do.
Where the tumor is located greatly affects the prognosis. Tumors in the limbs usually have a better chance of recovery than those in the pelvis or spine. Tumors in the chest wall also tend to have a better outlook. How easily the tumor can be removed and the chance of removing it all play big roles in survival.
The size of the tumor is a big factor in Ewing’s sarcoma. Bigger tumors often mean a worse prognosis because they’re more likely to spread. Tumor volume is also important. Smaller tumors usually mean better chances of survival.
Having metastasis at diagnosis is a big concern. Patients with spread have a much worse outlook than those without. Common places for metastasis include the lungs, bones, and bone marrow. Finding and treating metastasis early is key to better survival chances.
How well a patient responds to first treatment is a strong sign of long-term success. Those who fully respond to treatment tend to live longer. On the other hand, poor response to treatment means a higher risk of coming back and spreading, leading to a worse prognosis.
In summary, Ewing’s sarcoma’s prognosis depends on many things like tumor location, size, spread, and treatment response. Understanding these factors is vital for creating effective treatment plans and improving patient outcomes.
Surviving Ewing sarcoma means dealing with treatment’s late effects and keeping a good quality of life. Survivors move from treatment to long-term care, facing new challenges. These affect their health and happiness.
Ewing sarcoma survivors may face many late effects from treatment. These include:
It’s important to know about these late effects for proper follow-up care. Survivors should stay in close touch with their healthcare team to manage these issues.
Surveillance is key for Ewing sarcoma survivors’ long-term care. Regular check-ups and screenings help catch and manage late effects early. The recommended surveillance includes:
These protocols are customized based on the survivor’s treatment and risk factors. This ensures they get care that fits their needs.
Psychosocial support is vital for survivorship care. It addresses survivors’ emotional, social, and psychological needs. This support may include:
By combining these elements, Ewing sarcoma survivors can improve their quality of life. They can better navigate long-term survivorship with the right support.
Research on Ewing tumor is moving forward fast. This is because we want to make treatments better for patients. Scientists are studying the tumor’s molecular makeup to find new ways to treat it.
New treatments and better care plans are on the horizon. This will happen as we learn more about Ewing sarcoma’s genetics and biology. These advancements will help doctors treat the disease more effectively.
As research improves, so will how we manage Ewing tumor. This will make life better for those affected. New therapies and better care will be key in the fight against Ewing tumor.
Ewing’s Sarcoma is a rare cancer that affects bones or soft tissue around bones. It’s most common in kids and young adults. It’s known for a specific genetic change.
Yes, it’s a malignant cancer. It can grow and spread to other parts of the body. Early diagnosis and treatment are key.
It can happen in any bone, but often affects the pelvis, thigh bone, and ribs. It also occurs in soft tissues like muscles and fat, mainly in the chest, abdomen, and limbs.
It’s staged using the TNM system. This looks at the tumor size, nearby lymph nodes, and if it has spread. It’s either localized or metastatic, with further details based on size and location.
It’s when the cancer spreads to other parts of the body. Common places include the lungs, bones, and bone marrow. This affects treatment and outlook.
Diagnosis uses imaging like X-rays, MRI, and CT scans. A biopsy examines tissue samples. Molecular tests look for genetic changes. Histopathology confirms the diagnosis.
Treatment includes chemotherapy, surgery, and radiation. The plan depends on the disease stage. Localized disease might get chemotherapy and local treatments. Metastatic disease needs more intense chemotherapy and other treatments.
Prognosis varies based on tumor location, size, metastasis, and treatment response. Patients with localized disease usually have a better outlook than those with metastasis.
Survivors might face late effects like growth issues, fertility problems, and higher cancer risk. Long-term care is vital to manage these effects.
Long-term care includes watching for recurrence and late effects, psychosocial support, and rehabilitation. Survivors should lead a healthy lifestyle and stay in touch with their healthcare team.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!