Last Updated on November 26, 2025 by Bilal Hasdemir
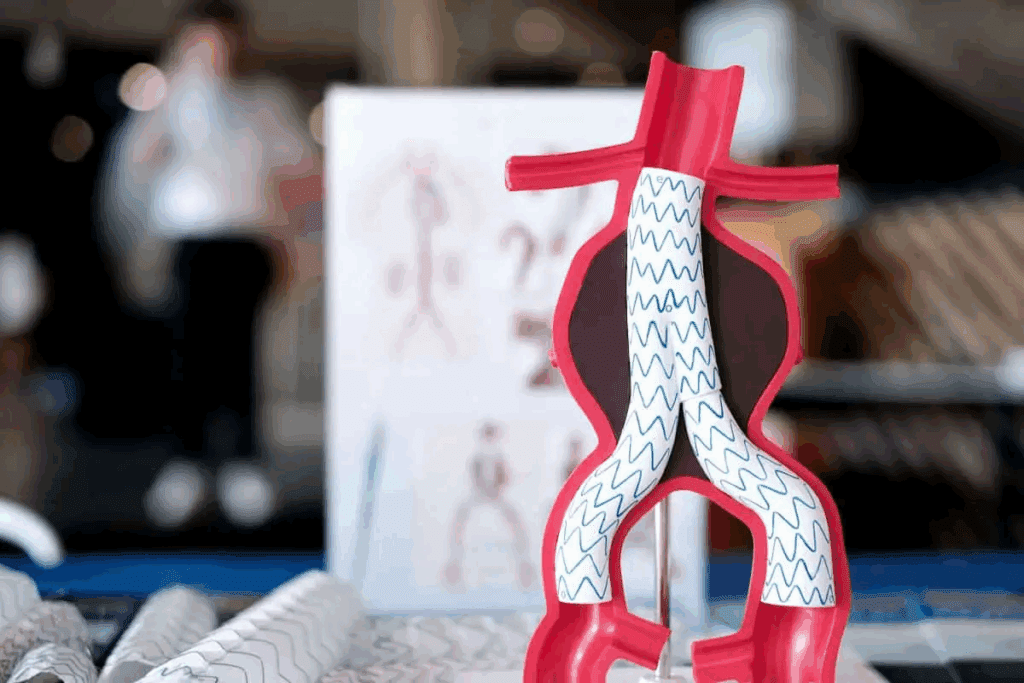
When an abdominal aortic aneurysm (AAA) isn’t detected early, the risk of rupture increases significantly. We understand how vital it is to treat it quickly and effectively. The EVAR procedure offers a less invasive way to repair the aneurysm, ensuring faster recovery and fewer complications compared to traditional surgery.
At Liv Hospital, we perform endovascular AAA treatments with precision and care. The EVAR procedure steps involve inserting a stent graft through small incisions in the groin to reinforce the weakened section of the aorta. This advanced method has transformed how we treat abdominal aortic aneurysms, making it a much safer and more effective choice than open surgery.
Key Takeaways
- EVAR is a minimally invasive procedure for treating AAA.
- The procedure involves inserting a stent graft to reinforce the weakened aorta.
- EVAR reduces recovery time and complication rates compared to open repair.
- Patients with AAAs larger than 5.5 cm or those growing rapidly are suitable candidates.
- Liv Hospital performs EVAR with precision, safety, and patient-centered care.
Understanding Abdominal Aortic Aneurysm (AAA)
It’s important to know about Abdominal Aortic Aneurysm (AAA) to treat it. An AAA is a bulge in the aorta, the main artery from the heart to the abdomen. This bulge can burst, causing severe bleeding inside the body.
Definition and Pathophysiology of AAA
An AAA is when the aorta wall bulges more than 1.5 times its normal size, usually over 3 cm. It happens due to a mix of genetics, environment, and how the aorta works. This mix weakens the aorta wall, making it hard to handle blood pressure.
The aorta has three layers: intima, media, and adventitia. In AAA, the media layer gets inflamed and weakens. This is because elastin and collagen break down, making the wall less strong.
Risk Factors and Prevalence
Several things can increase the risk of getting AAA. These include:
- Smoking: It damages the aortic wall and makes aneurysms grow faster.
- Hypertension: High blood pressure adds stress to the aortic wall, raising the risk of aneurysms.
- Family History: Having a first-degree relative with AAA increases your risk.
- Age and Gender: Men and people over 65 are more likely to get AAA.
AAA is found in about 4-8% of men over 65. Many countries have screening programs to find AAA early. Early treatment can greatly improve outcomes.
Clinical Presentation and Diagnosis
AAA usually doesn’t show symptoms until it bursts. Symptoms might include:
- Abdominal or back pain
- Pulsatile abdominal mass
- Embolic events
Doctors use imaging to diagnose AAA. Ultrasound is often the first test because it’s non-invasive and works well. Computed Tomography (CT) scans give more detailed info about the aneurysm. This is key for planning treatment, like EVAR (Endovascular Aneurysm Repair).
Traditional vs. Endovascular Approaches for AAA Repair
There are two main ways to fix an Abdominal Aortic Aneurysm (AAA): open surgery and endovascular repair. Each method has its own good points and downsides. We’ll look at both, so you can understand your options for treating AAA.
Open Surgical Repair: Overview and Limitations
Open surgery for AAA means a big cut in the belly to reach the aorta. It’s been around for a long time and works well. But, it hurts a lot after and takes longer to get better. Studies show it’s riskier, mainly for people with other health issues.
The downsides of open surgery are:
- It hurts a lot after
- You’ll stay in the hospital longer
- It’s riskier
- It takes longer to feel better
Advantages of Endovascular Repair
EVAR is a newer, less invasive way to fix AAA. It uses a special graft through the legs to seal off the aneurysm. EVAR is better because it hurts less, you get out of the hospital faster, and it’s safer than open surgery.
The good things about EVAR are:
- It’s less invasive
- It hurts less after
- You’ll be out of the hospital sooner
- It heals faster
Comparative Outcomes and Evidence Base
Many studies have looked at how open surgery and EVAR compare. It’s important to understand the differences to make the right choice. We’ll look at the evidence to help doctors and patients decide.
| Outcomes | Open Surgical Repair | Endovascular Repair (EVAR) |
| Recovery Time | Longer | Shorter |
| Postoperative Pain | Significant | Less |
| Risk of Complications | Higher | Lower |
Studies from Northern Heart Hospital Penang show EVAR is better. It means quicker recovery and fewer risks than open surgery, just like many other studies say.
Patient Selection and EVAR Criteria
Choosing the right patients for EVAR is complex. It looks at aneurysm size, how well the anatomy fits, and the patient’s health. The goal is to pick those who will get the most from this less invasive surgery.
Size Thresholds for Intervention
The size of the aortic aneurysm is key in deciding if surgery is needed. Guidelines say EVAR is best for AAAs larger than 5.5 cm in diameter. This size is when the risk of rupture is high, making surgery safer.
A study in the Journal of Vascular Surgery shows risks. AAAs between 5 to 5.9 cm have a 1% to 7% yearly rupture risk. But, for those ≥6 cm, the risk jumps to 10% to 33% yearly.
Anatomical Considerations for EVAR Eligibility
How well the body fits the EVAR procedure is also important. The aortic neck and iliac artery anatomy must be right for the endograft. CT angiography helps check these areas.
Important things to look at include:
- Aortic neck diameter and length
- Angle and shape of the aortic neck
- Iliac artery size and twists
- Any big calcifications or clots
Patient Comorbidities and Risk Assessment
Looking at a patient’s health issues is key to see if EVAR is safe. Those with serious health problems, like heart or kidney disease, need extra checks before surgery.
Checking the patient’s:
- Heart health
- Kidney function
- Lung health
- Overall health
| Comorbidity | Impact on EVAR | Pre-procedural Consideration |
| Severe Heart Disease | Increased risk of cardiac complications | Cardiac evaluation and optimization |
| Chronic Kidney Disease | Risk of contrast-induced nephropathy | Hydration and minimization of contrast |
| Chronic Obstructive Pulmonary Disease (COPD) | Increased risk of respiratory complications | Pulmonary function tests and optimization of COPD management |
By carefully looking at these factors, we can find the best candidates for EVAR. This helps reduce the risks of the surgery.
Preoperative Planning for EVAR
Getting ready for an EVAR procedure is key to success. We focus on a detailed plan. This includes imaging studies, choosing the right endograft, and preparing the team.
Imaging Requirements and Protocols
Good imaging is the base of EVAR planning. We use CT scans and angiography to check the aneurysm’s details. Northern Heart Hospital Penang says this is vital for planning.
Endograft Selection and Sizing
Picking the right endograft is a big deal. We look at the aneurysm’s size and the neck’s length. This ensures a good fit and lowers risks.
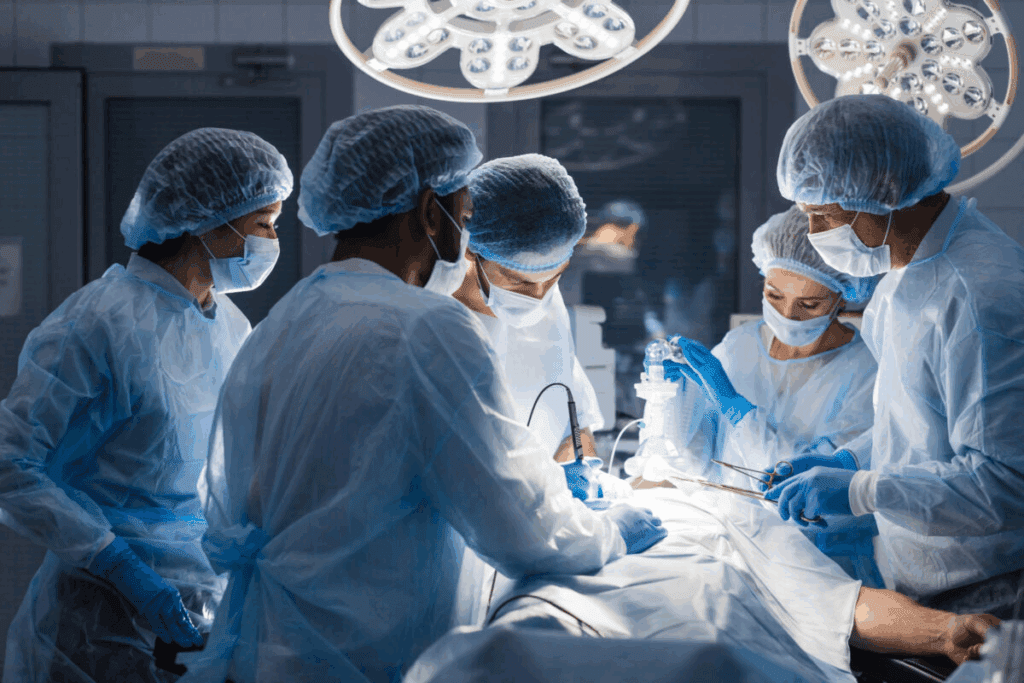
Procedural Team Preparation
A ready team is essential for EVAR success. Our team reviews the case and plans the procedure. They make sure all equipment is ready and know the endograft.
With careful planning, we aim for the best EVAR results. This way, we give our patients the best care.
EVAR Procedure Steps: A Complete Guide
Doing an EVAR procedure needs careful planning and skill. It’s all about choosing the right patient, planning well before surgery, and doing the surgery right.
Patient Preparation and Anesthesia Considerations
Getting ready for an EVAR procedure is key. We look at the patient’s health, past medical issues, and body shape to pick the best plan. Choosing the right anesthesia is also important. The right choice depends on the patient’s health, how complex the surgery is, and what the doctors think.
We make sure the patient is set up right on the table. This includes good monitoring and easy access for the team. Good preparation lowers risks and makes the surgery go smoothly.
Femoral Artery Access Techniques
Getting to the femoral artery is a big part of the EVAR procedure. We use imaging and surgery to get there. Getting it right is key for placing the endograft correctly.
We make a small cut in the groin and put in a guidewire and sheath. We use imaging to make sure we’re in the right spot.
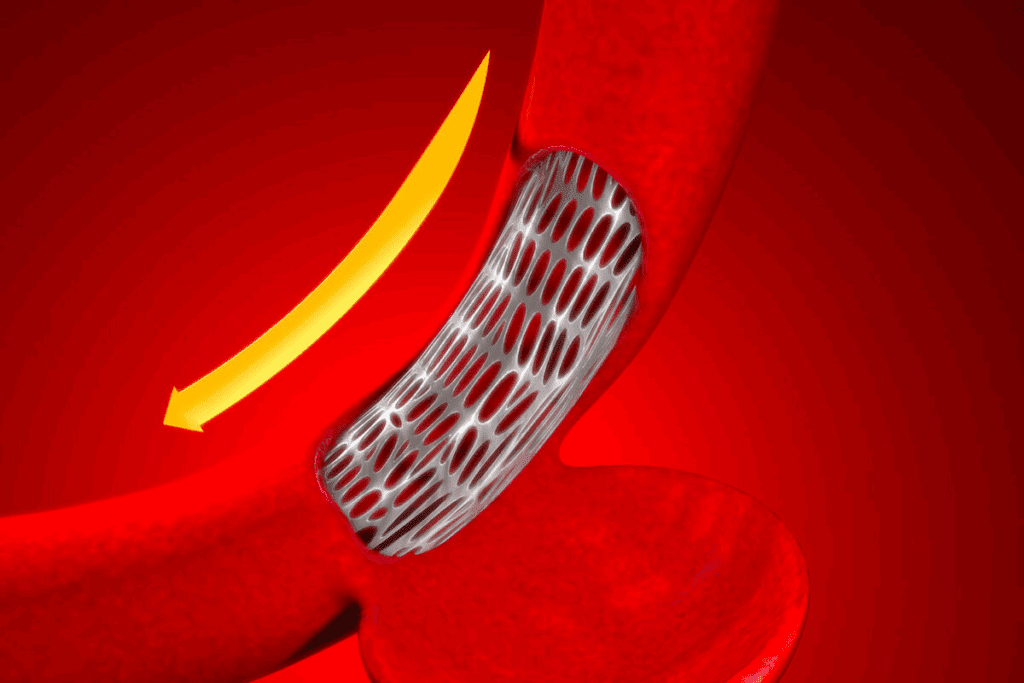
Endograft Delivery and Deployment
Putting in and setting up the endograft is a big step. We pick the right size for the patient’s body. We use imaging to make sure it’s in the right place.
After it’s in, we expand it and attach it to the aortic wall. Getting it right is important to avoid leaks and ensure the procedure works long-term.
Completion Angiography and Adjunctive Procedures
We do a final check with angiography to see if the endograft worked. We use imaging to check the aneurysm sac. If there are leaks, we do extra steps to fix them.
These extra steps might include putting in more stents or using coils. We do this to make sure the aneurysm sac is fully blocked.
Potential Complications and Management Strategies
It’s important to know about the possible problems with EVAR for good care. When we talk about endovascular repair of abdominal aortic aneurysm, we must see the risks and how to lessen them.
Intraoperative Complications
During EVAR, several issues can happen. These include:
- Bleeding or hematoma at the access site
- Stent graft malpositioning or migration
- Endoleak, which is the leakage into the aneurysm sac
- Vascular injury, such as dissection or rupture
We use different methods to handle these problems. This includes choosing the right stent graft size and careful access site care. Intraoperative imaging is key in spotting and fixing these issues quickly.
Early Postoperative Complications
Right after surgery, patients might face issues like:
- Endoleak, which needs close watching
- Access site problems, like infection or pseudoaneurysm
- Heart problems, such as myocardial infarction
- Kidney issues, like contrast-induced nephropathy
We tackle these problems with surveillance imaging and watching the patient closely. Finding these issues early is vital for good care.
Late Complications and Their Management
Later on, EVAR can lead to:
- Stent graft migration or endoleak
- Aneurysm rupture, a serious risk
- Device problems, like stent fracture
Handling late problems means watching patients over time and sometimes doing more surgery. We stress the need for long-term follow-up to catch and deal with these issues well.
In summary, EVAR is a good choice for AAA, but knowing and managing its possible problems is key for the best results. By understanding these issues and using good management strategies, we can give our patients the best care for evar for aneurysm repair.
Advanced EVAR Techniques for Complex Anatomy
Advanced EVAR techniques have changed how we treat complex abdominal aortic aneurysms (AAA). These new methods help vascular surgeons treat patients with hard-to-reach anatomy. This is for those who might not fit the standard EVAR procedures.
Fenestrated and Branched Endografts
Fenestrated and branched endografts are special devices for complex AAA cases. They help keep blood flowing to important organs like the kidneys and intestines.
Using these devices needs careful planning before surgery. This includes detailed images to figure out the best device setup.
| Device Type | Indications | Benefits |
| Fenestrated Endografts | AAA with short or angulated necks | Preserves blood flow to renal and visceral arteries |
| Branched Endografts | AAA with complex visceral artery anatomy | Maintains perfusion to vital organs |
Chimney and Snorkel Techniques
The chimney and snorkel techniques help with complex AAA cases. They use extra stents to keep blood flowing to important areas.
These methods are good for tough cases but come with higher risks. Risks include endoleaks and stent migration.
Managing Challenging Iliac Anatomy
Dealing with tricky iliac arteries can make EVAR harder. Using iliac branched devices and other advanced methods helps solve these problems.
Choosing the right devices and planning carefully is key for managing tough iliac anatomy.
With these advanced EVAR techniques, we can better treat complex AAA cases. This improves patient results and lowers the chance of problems.
Postoperative Care and Follow-up Protocols
After EVAR, a detailed care plan is key to handle any issues and keep an eye on the aneurysm. This plan includes immediate care, regular scans, and quick action for any problems.
Immediate Postoperative Management
Right after surgery, we focus on easing pain, watching for issues, and making sure the patient is stable. This early stage is very important for a good recovery and future health. Close monitoring in an ICU or step-down unit is sometimes needed, mainly for patients with serious health problems.
We use multimodal analgesia to manage pain well, cutting down on opioid use and its side effects. We also watch for signs of complications like bleeding, endoleak, or issues with the access site.
Surveillance Imaging Schedule
Regular scans are a big part of care after surgery. We use ultrasound or CT scans to check the aneurysm size and look for endoleaks or other issues. How often we do these scans depends on the patient’s risk factors and the surgery details.
| Time Frame | Imaging Modality | Purpose |
| 1 month | CT Angiography | Baseline assessment post-EVAR |
| 6 months | Ultrasound or CT | Monitor aneurysm sac size and detect endoleaks |
| 1 year | CT Angiography | Comprehensive assessment of aneurysm and endograft |
Managing Endoleaks and Other Complications
Endoleaks are a big worry after EVAR, as they can keep the aneurysm sac pressurized and might cause rupture. We sort endoleaks into types based on why they happen and how to treat them. Type I and Type III endoleaks are high-risk and often need quick action. Type II endoleaks might be watched or treated based on their type and the patient’s health.
Handling complications well needs a team effort. Vascular surgeons, interventional radiologists, and others work together. This teamwork helps improve patient results and lowers the chance of long-term problems.
Conclusion
Endovascular Aneurysm Repair (EVAR) has changed how we treat Abdominal Aortic Aneurysm (AAA). It’s a less invasive method compared to traditional surgery. By learning about the evar procedure steps, doctors can help patients recover faster and avoid complications.
EVAR for AAA is safe and works well, with few problems. Studies show it lowers the risk of serious issues compared to open surgery. Places like Liv Hospital are experts in EVAR, giving patients top-notch care for evar for aaa.
In short, EVAR is a big step forward in treating AAA. It offers a less invasive way to help patients, leading to better results. As technology gets better, EVAR’s role in treating AAA will grow, improving care even more.
FAQ
What is EVAR and how does it treat AAA?
EVAR stands for Endovascular Aneurysm Repair. It’s a way to treat Abdominal Aortic Aneurysm (AAA). A stent graft is inserted through small incisions in the groin. This reinforces the weakened aorta, preventing further growth and rupture.
What are the benefits of EVAR compared to traditional open surgery?
EVAR has many benefits. It leads to quicker recovery, less pain, and fewer complications. It’s a less invasive option, making it good for those at high risk for surgery.
What are the criteria for selecting patients for EVAR?
Doctors choose patients for EVAR based on several factors. These include the size of the aneurysm and the patient’s health. CT scans help determine if EVAR is right for a patient.
What are the possible complications of EVAR?
EVAR can have complications. These include bleeding and issues with the stent graft during surgery. After surgery, there are risks like endoleak and access site problems. Later, there’s a chance of stent graft migration and aneurysm rupture.
How is EVAR performed?
The EVAR procedure involves several steps. First, the patient is prepared and given anesthesia. Then, the femoral artery is accessed, and the stent graft is delivered and deployed. The procedure is guided by imaging to ensure the stent graft is placed correctly.
What is the role of imaging studies in EVAR?
Imaging studies, like CT scans and angiography, are key in EVAR. They help decide if EVAR is right for a patient, plan the procedure, and watch for complications. Regular imaging is also needed to catch any late complications.
What are fenestrated and branched endografts used for?
Fenestrated and branched endografts treat complex AAA cases. They involve the renal or visceral arteries. These advanced grafts help patients who can’t have standard EVAR.
What is the postoperative care and follow-up protocol for EVAR?
After EVAR, patients need careful postoperative care. This includes immediate management and a surveillance imaging schedule. It also involves managing endoleaks and other complications. Regular follow-ups are key to monitor for complications and ensure the procedure’s success.
How does EVAR compare to open surgical repair in terms of outcomes?
EVAR often has better outcomes than open surgery. It has lower morbidity and mortality rates. Yet, the choice between EVAR and open repair depends on the patient’s specific situation and anatomy.
References:
- Patel, R., et al. (2022). Outcomes and long-term durability of EVAR versus open repair: A systematic review. Journal of Vascular Surgery, 75(4), 1151-1164. https://pubmed.ncbi.nlm.nih.gov/35066389/






