Sickle cell disease symptoms is a group of inherited blood disorders. It affects how the body makes hemoglobin, leading to abnormal red blood cells. These cells can cause health problems like anemia, severe pain episodes, and a higher risk of infections.
At Liv Hospital, we know how important it is to spot the key symptoms of this condition.
Vaso-occlusive crises are a big problem in sickle cell disease. They happen when sickle-shaped red blood cells block blood flow, causing severe pain. It’s key to understand these episodes to manage and treat them well.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- Abnormal red blood cells can cause various health issues.
- Vaso-occlusive crises are characterized by severe pain due to obstructed blood flow.
- Recognizing key symptoms is key for effective management.
- Liv Hospital offers top-notch care for sickle cell disease patients.
What Is Sickle Cell Disease: Pathophysiology and Prevalence

Sickle cell disease is a complex condition caused by a genetic mutation. This mutation affects the structure of hemoglobin. It leads to the production of abnormal hemoglobin, known as hemoglobin S (HbS).
This abnormal hemoglobin can cause red blood cells to take on a sickle shape under certain conditions.
The Genetic Mutation Behind Sickle Cell Disease
The genetic mutation causing sickle cell disease happens when a person gets two abnormal copies of the β-globin gene. They get one from each parent. This leads to the production of HbS.
HbS polymerizes under low oxygen conditions. This causes red blood cells to sickle.
Key aspects of this genetic mutation include:
- Inheritance pattern: Autosomal recessive
- Effect on hemoglobin: Production of abnormal hemoglobin S
- Impact on red blood cells: Sickling under low oxygen conditions
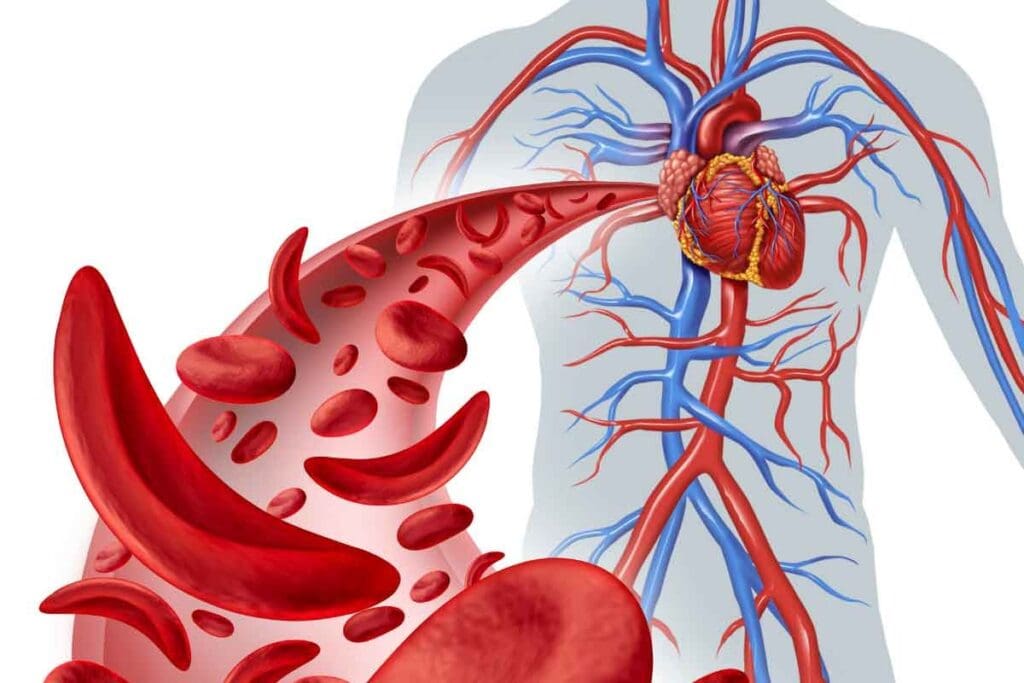
How Sickled Red Blood Cells Affect Circulation
Sickled red blood cells are less flexible and more prone to hemolysis. This leads to various circulatory issues. These include:
- Vaso-occlusion: Blockage of small blood vessels by sickled cells
- Hemolytic anemia: Premature destruction of red blood cells
- Inflammation: Activation of inflammatory pathways due to cell damage
These issues contribute to the symptoms and complications of sickle cell disease.
Global Distribution and Prevalence
Sickle cell disease is a significant global health issue. It’s most common in parts of sub-Saharan Africa, the Middle East, and India. This is because malaria has been prevalent in these areas historically.
Prevalence data highlights:
- High prevalence in areas with historical malaria endemicity
- Significant numbers of carriers in these regions
- Increasing prevalence in other areas due to migration
Understanding the global distribution and prevalence of sickle cell disease is key. It’s essential for developing effective public health strategies.
Common Sickle Cell Disease Symptoms and Their Onset
Sickle cell disease symptoms can start early in life. How severe they are can vary a lot. We’ll look at when symptoms start, how they differ, and what affects their severity.
When Symptoms Typically First Appear
Signs of sickle cell disease often show up in early childhood. Babies might start showing symptoms in the first few months. This is because adult hemoglobin, which can sickle, replaces fetal hemoglobin. Early diagnosis through newborn screening has greatly helped manage the disease.
Variability in Symptom Presentation
The severity and how often symptoms happen can differ a lot among people with sickle cell disease. Some might have mild symptoms, while others face frequent pain and other issues. This difference is because of many factors, like the specific genetic mutation and the environment.
Factors Affecting Symptom Severity
Many things can change how bad sickle cell disease symptoms are. These include genetics, the environment, and healthcare access. For example, staying hydrated and avoiding extreme temperatures can help manage symptoms. Genetic modifiers can also change how severe the disease is.
Knowing these factors is key to creating treatment plans that fit each patient’s needs.
Anemia: Chronic Fatigue and Shortness of Breath
Sickle Cell Disease causes anemia due to the quick breakdown of red blood cells. This leads to less oxygen in the blood. It causes symptoms that really affect patients’ lives.
Hemolysis and Reduced Oxygen-Carrying Capacity
Hemolysis is when red blood cells break down. This is a big problem in Sickle Cell Disease. It means there are fewer red blood cells and less oxygen for the body.
Patients often feel chronic fatigue and shortness of breath. This is because their red blood cells can’t carry enough oxygen. The abnormal hemoglobin S in these cells makes them sickle and break down faster.
Clinical Signs of Anemia in Sickle Cell Patients
People with Sickle Cell Disease show signs of anemia like:
- Pale skin and mucous membranes
- Fatigue and weakness
- Shortness of breath (dyspnea)
- Dizziness or lightheadedness
- Headaches
These symptoms can be different for everyone. Some people might feel worse than others, even if they have the same level of anemia.
Managing Anemia Symptoms
There are many ways to manage anemia in Sickle Cell Disease. The main goal is to stop the red blood cells from breaking down so fast. Here are some ways to help:
- Blood transfusions: Getting regular transfusions can increase normal red blood cells. This helps reduce anemia and its symptoms.
- Hydration: Drinking plenty of water can help lower hemoglobin S levels. This makes it less likely for red blood cells to sickle.
- Nutritional support: Eating enough folate and other nutrients helps make more red blood cells.
Understanding anemia in Sickle Cell Disease and using these strategies can improve patients’ lives. It can also lower the risk of serious problems from chronic anemia.
Vaso-Occlusive Crisis: Understanding Painful Episodes
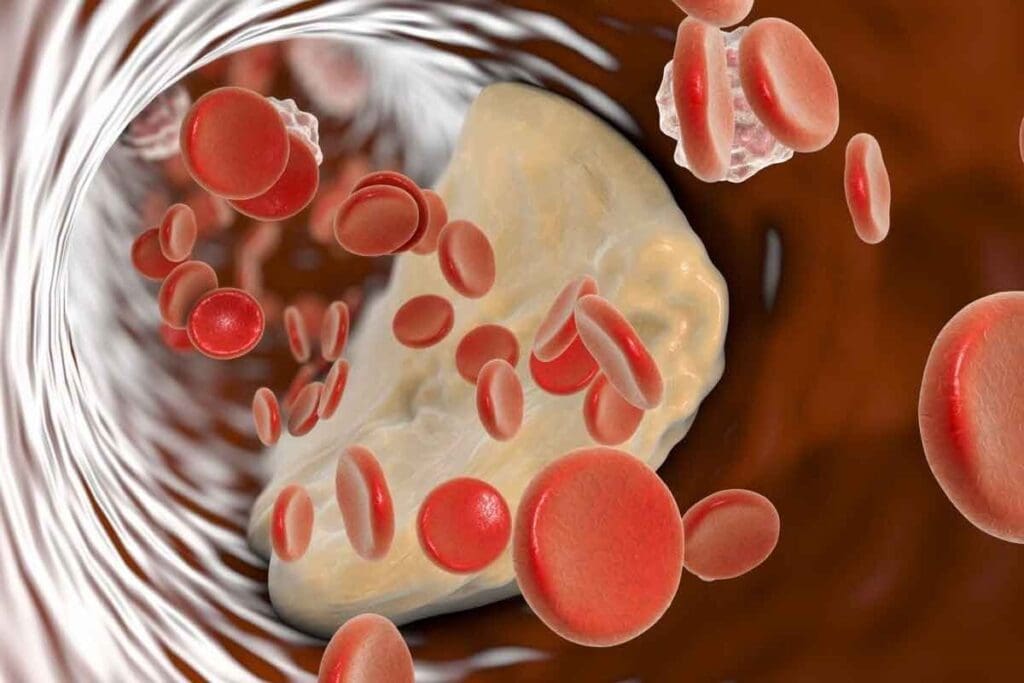
It’s important to know about vaso-occlusive crises to manage sickle cell disease. These episodes can be very hard to deal with. They happen when sickled red blood cells block small blood vessels, causing pain and tissue ischemia.
Mechanism of Blood Vessel Blockage
Vaso-occlusive crises occur when red blood cells sickle in low oxygen, dehydration, or acidosis. These sickled cells are stiff and stick together, blocking small vessels and stopping blood flow.
Common Triggers of Pain Crises
Several things can start a vaso-occlusive crisis, like cold weather, dehydration, infections, and stress. Knowing what triggers these crises helps prevent or lessen their pain.
- Cold weather can make blood vessels narrow, reducing blood flow.
- Dehydration makes red blood cells more concentrated, leading to sickling.
- Infections cause inflammation and increase the body’s need for oxygen, making sickling worse.
- Stress can change the body’s physiology, triggering a crisis.
Typical Duration and Intensity of Episodes
The length and severity of vaso-occlusive crises vary. Some last just a few hours, while others can go on for days. The pain can be mild or very severe, sometimes needing hospital care.
| Characteristics | Variability |
| Duration | A few hours to several days |
| Intensity | Mild to severe |
| Management | Home care to hospitalization |
To manage vaso-occlusive crises well, a full plan is needed. This includes preventing them, recognizing early signs, and using the right treatments. Knowing how these crises start and what triggers them helps doctors give better care.
Recognizing Signs of an Impending Vaso-Occlusive Crisis
Knowing the signs of a vaso-occlusive crisis can help prevent it. These crises are severe pain episodes common in sickle cell disease. Spotting early signs is key to managing them well.
Early Warning Symptoms
There are several early signs of a vaso-occlusive crisis. These include:
- Increased pain or discomfort
- Fatigue
- Fever
- Nausea or vomiting
- Changes in skin color or temperature
Knowing these symptoms helps patients start preventive actions early.
Preventive Strategies During Early Signs
When you notice early signs, you can take steps to prevent a crisis. Here are some strategies:
| Strategy | Description |
| Hydration | Drinking plenty of fluids to prevent dehydration |
| Pain Management | Using prescribed pain medications as directed |
| Rest | Avoiding strenuous activities and getting adequate rest |
These steps can lessen the crisis’s impact.
“Early recognition and intervention are key to managing vaso-occlusive crises effectively.”
Expert Opinion
When to Seek Emergency Care
Even with preventive steps, some crises need urgent medical help. You should go to the emergency room if:
- Pain is severe and not relieved by prescribed medications
- There are signs of infection, such as a high fever
- There is difficulty breathing or chest pain
- Neurological symptoms, such as confusion or weakness, occur
Dactylitis: Hand-Foot Swelling in Infants and Children
Dactylitis is a painful swelling in the hands and feet of infants. It’s a key early sign of sickle cell disease in young children. We’ll look at how to spot it, tell it apart from other conditions, and how to treat it.
Clinical Presentation in Children Under Age One
Dactylitis usually hits infants between 6 months and 2 years old. The swelling is often the same on both sides. It can also bring fever and fussiness.
The symptoms can differ, but often include:
- Swelling in hands and feet
- Pain when touching or moving the affected limbs
- Fever
- Irritability
Distinguishing Dactylitis from Other Conditions
Figuring out if it’s dactylitis means ruling out other causes of swelling or pain. Doctors look at the child’s history, do a physical check, and might run tests like blood counts and imaging.
What makes dactylitis stand out includes:
- The child’s age, as dactylitis is most common in infants under 1 year
- Known sickle cell disease or trait
- Swelling that affects both hands and feet equally
Treatment Approaches for Hand-Foot Syndrome
Managing dactylitis aims to ease symptoms and avoid serious problems. Treatment might include drinking lots of water, using pain meds, and resting the affected limbs. Parents are taught to watch their child closely and know when to get help.
Key treatment strategies include:
- Drinking enough water to avoid dehydration
- Managing pain well
- Watching for signs of complications or infection
Increased Infection Risk: A Major Complication
People with sickle cell disease face a higher risk of infections. This is mainly because their spleen doesn’t work right. The spleen is key to filtering blood and storing immune cells.
Splenic Dysfunction and Immune Compromise
The spleen helps fight off infections by removing certain bacteria from the blood. But, sickle cell disease can damage the spleen. This damage can lead to asplenia, making it hard to fight off infections.
Immune compromise in sickle cell disease goes beyond spleen issues. Other immune problems, like issues with the complement system and neutrophils, also raise the risk of getting sick.
Common Bacterial Infections in Sickle Cell Patients
Those with sickle cell disease are more likely to get infections from bacteria like Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis. These can lead to serious illnesses like pneumonia, meningitis, and septicemia.
Children under 5 and adults with sickle cell disease are at high risk. It’s important to catch and treat infections quickly to avoid serious problems.
Vaccination and Antibiotic Prophylaxis
Vaccination is key to lowering the risk of infections. People with sickle cell disease should get shots against Streptococcus pneumoniae, Haemophilus influenzae type b, and Neisseria meningitidis as advised by health experts.
Antibiotic prophylaxis is also recommended for kids with sickle cell disease. It starts at 2 months and lasts until at least 5 years old. Penicillin is often used, but other antibiotics are options for those allergic to penicillin.
By knowing why infections are more common and using preventive steps, we can help lower the infection rate in sickle cell disease patients.
Growth and Development Delays in Children
It’s important to know how sickle cell disease affects children’s growth and development. This disease can slow down growth and development because of chronic anemia and other problems.
Physical Development Impact
Children with sickle cell disease often grow slower physically. Chronic anemia makes it hard for their blood to carry oxygen. This leads to tiredness and less activity, which can slow their growth.
Studies show these kids might be shorter and lighter than their peers(PMC10413179).
Key factors affecting physical development include:
- Chronic anemia and reduced oxygen delivery to tissues
- Increased energy expenditure due to the disease
- Nutritional deficiencies
Delayed Sexual Maturation
Sickle cell disease can also delay puberty in children. This is partly because of the illness and lack of nutrients. Such delays can affect their physical and mental health.
Nutritional support is key in managing these delays. Getting enough nutrients is important for growth and development.
Nutritional Interventions and Monitoring
Nutritional help is vital for managing growth delays in sickle cell disease. It’s important to make sure kids get enough calories and nutrients. Regular checks on their growth are also essential.
Nutritional strategies include:
- Increased caloric intake to meet the heightened energy demands
- Supplementation with folate and other essential nutrients
- Regular assessment of growth and developmental milestones
Understanding sickle cell disease’s effects and using the right nutrition can help. Healthcare providers can lessen developmental delays with the right care.
Jaundice and Gallstones: Hepatobiliary Complications
Sickle cell disease can lead to problems like jaundice and gallstones. These issues affect the liver and gallbladder. They cause serious health problems for those with the disease.
Mechanisms of Jaundice Development
Jaundice makes the skin and eyes turn yellow. It happens when there’s too much bilirubin in the body. In sickle cell disease, breaking down red blood cells increases bilirubin levels.
The liver struggles to handle this extra bilirubin. This can cause jaundice. The liver’s job is to process bilirubin from broken-down red blood cells. But, when there’s too much, the liver gets overwhelmed.
Symptoms of Gallstone Formation
Gallstones are common in sickle cell disease. They form because of the extra bilirubin. Symptoms include stomach pain, nausea, and vomiting, often after eating fatty foods.
It’s important to notice these symptoms early. People with sickle cell disease should watch for them. If they have severe or ongoing pain, they should see a doctor.
Management Options for Liver Complications
Dealing with jaundice and gallstones in sickle cell disease requires a few steps. For jaundice, the goal is to manage the cause, like controlling hemolysis. For gallstones, treatment can range from pain relief to surgery, like a cholecystectomy.
Regular check-ups and care are key for those with sickle cell disease. This helps catch and manage liver problems early. It improves their quality of life and lowers the risk of serious issues.
Acute Chest Syndrome: A Life-Threatening Emergency
Acute chest syndrome is a serious emergency in sickle cell disease. It can quickly become life-threatening. This condition is marked by a new lung issue on chest X-rays, fever, breathing problems, or chest pain. It’s a major reason for sickness and death in those with sickle cell disease.
Distinguishing Features from Pneumonia
Acute chest syndrome looks like pneumonia but is different. It often comes with fat in the blood, infections, or other issues. Symptoms include coughing, chest pain, fever, and trouble breathing. To tell it apart from pneumonia, doctors use tests and imaging.
Diagnostic Challenges: It’s hard to tell acute chest syndrome from pneumonia because they look similar. Doctors must be careful to find the cause of breathing problems to treat it right.
Risk Factors and Prevention
Some things make you more likely to get acute chest syndrome. These include asthma, having had it before, and high hemoglobin levels. To prevent it, managing sickle cell disease well is key. This includes regular check-ups, taking medicine as told, not smoking, and treating infections fast.
Treatment Protocol and Hospitalization
Handling acute chest syndrome needs a team effort. This includes:
| Treatment Component | Description |
| Oxygen Therapy | To keep oxygen levels up |
| Fluid Management | Drinking enough water to avoid too much fluid |
| Antibiotics | To fight off infections |
| Pain Management | Enough pain relief to feel better |
| Blood Transfusion | In some cases, to lower the hemoglobin |
Most people need to stay in the hospital to watch their condition closely. Quick action and treatment are key to avoiding serious problems and achieving better outcomes.
Stroke and Neurological Manifestations
Sickle cell disease can cause severe brain problems, like stroke. This happens when sickled red blood cells block brain’s blood vessels. This blockage can damage brain tissue and lead to lasting or permanent brain problems.
Warning Signs of Cerebrovascular Events
It’s important to know the signs of a stroke or brain problems. These signs include:
- Weakness or numbness in the face, arm, or leg, typically on one side of the body
- Difficulty speaking or understanding speech
- Sudden vision changes or loss of vision in one or both eyes
- Severe headache with no known cause
- Dizziness or loss of balance
People with sickle cell disease and their caregivers should watch for these signs. If they see any, they should get medical help right away.
Transcranial Doppler Screening
Transcranial Doppler (TCD) screening is a safe way to check for stroke risk in kids with sickle cell disease. It uses ultrasound to see how fast blood flows in brain arteries. It finds problems that could lead to a stroke.
Regular TCD screenings are suggested for kids aged 2 to 16. Early detection helps prevent stroke with treatments like blood transfusions.
Cognitive Effects of Cerebrovascular Events
Brain problems, like stroke, can hurt thinking skills in people with sickle cell disease. They might struggle with memory, focus, speed, and making decisions.
It’s key to check brain and thinking skills well. Early help can make a big difference. It helps people get back lost skills and adjust to any lasting changes.
Chronic Organ Damage: Long-Term Complications
Living with sickle cell disease means facing chronic organ damage. This can affect many organs, leading to long-term issues that change life quality.
Kidney Dysfunction and Proteinuria
Sickle cell disease can harm the kidneys, causing chronic kidney disease and proteinuria. The kidneys struggle to filter waste because of sickled red blood cells. This leads to losing proteins in urine.
Key aspects of kidney dysfunction include:
- Reduced ability to filter waste products
- Proteinuria, or the presence of excess proteins in the urine
- Increased risk of progressing to end-stage renal disease
It’s important to regularly check kidney function. This helps catch and manage kidney problems early.
Pulmonary Hypertension
Pulmonary hypertension is a serious issue for those with sickle cell disease. It’s high blood pressure in the arteries that carry blood to the lungs.
The causes of pulmonary hypertension in sickle cell disease are multifactorial:
- Chronic hemolysis leading to nitric oxide depletion
- Chronic thromboembolic disease
- Left ventricular dysfunction
Early detection through echocardiography and other tools is key. It helps manage pulmonary hypertension well.
Leg Ulcers and Skin Manifestations
Leg ulcers are common in sickle cell disease patients. They happen due to chronic ischemia and poor wound healing.
Management strategies include:
- Wound care and dressing
- Pain management
- Prevention of infection
Vision Problems and Retinopathy
Sickle cell disease can harm the eyes, causing retinopathy and vision issues. Sickled red blood cells can block small vessels in the retina.
Regular eye examinations are key for:
- Early detection of retinopathy
- Monitoring disease progression
- Timely intervention to prevent vision loss
Good eye care is vital for managing sickle cell disease.
Conclusion: Comprehensive Management of Sickle Cell Disease
Managing sickle cell disease well needs a team effort. This includes medical care, prevention, and support. We stress the need for full care to better the lives of those with sickle cell disease.
Effective management means regular doctor visits, making lifestyle changes, and watching for problems. This way, we can lessen the pain and other issues caused by the disease.
We aim to give sickle cell patients the care they need to live well. By managing the disease fully, patients can enjoy a better life, despite its challenges.
By focusing on full management of sickle cell disease, we can greatly improve the lives of those affected. We provide the support and care they need to succeed.
FAQ
What are the common symptoms of sickle cell disease?
Symptoms include anemia, pain episodes, infections, and swelling in hands and feet. Jaundice and a higher stroke risk are also common. The severity and frequency vary among patients.
What is a vaso-occlusive crisis in sickle cell disease?
A vaso-occlusive crisis happens when sickled red blood cells block blood vessels. This causes tissue ischemia and pain. It can be triggered by dehydration, cold, and stress.
How does sickle cell disease affect red blood cells?
It causes a genetic mutation leading to abnormal hemoglobin. This makes red blood cells sickle. Sickled cells are more likely to be destroyed and block blood vessels.
What are the early warning signs of a vaso-occlusive crisis?
Early signs include increased pain, fever, swelling, and feeling unwell. Spotting these signs early is key for timely treatment.
How is anemia managed in sickle cell disease?
Anemia management includes blood transfusions, folic acid, and monitoring hemoglobin. The goal is to improve oxygen delivery and reduce symptoms.
What is dactylitis, and how is it treated?
Dactylitis, or hand-foot syndrome, causes swelling and pain in hands and feet, common in young children. Treatment involves hydration, pain management, and monitoring.
Why are patients with sickle cell disease at increased risk of infections?
The disease can cause splenic dysfunction, making it hard to fight infections. Vaccinations and antibiotics help prevent infections.
How does sickle cell disease affect growth and development in children?
It can affect physical development and sexual maturation due to chronic anemia. Nutritional support and regular monitoring are key for healthy development.
What are the hepatobiliary complications associated with sickle cell disease?
Complications include jaundice and gallstones from hemolysis and bilirubin buildup. Monitoring liver function and addressing gallstones are part of management.
What is acute chest syndrome, and how is it treated?
Acute chest syndrome is a serious condition with chest pain, fever, and respiratory symptoms. Treatment includes hospitalization, oxygen, pain management, and antibiotics.
What are the neurological manifestations of sickle cell disease?
Neurological issues include stroke and cognitive impairments. Screening and preventive transfusions can reduce stroke risk.
What long-term complications can arise from sickle cell disease?
Long-term issues include kidney dysfunction, pulmonary hypertension, leg ulcers, and vision problems. Regular monitoring and management are vital to prevent these complications.
How can sickle cell disease be comprehensively managed?
Management involves medical treatment, lifestyle changes, and ongoing monitoring. This approach improves the quality of life for patients.
References
- GeneReviews® Editorial Board. (2013). Sickle cell disease: Genetics, pathophysiology, clinical features. https://www.ncbi.nlm.nih.gov/books/NBK1377/
- Kato, G. J., Piel, F. B., Reid, C., et al. (2018). Sickle cell disease. Nature Reviews Disease Primers, 4, 18010. https://www.nature.com/articles/nrdp201810
- World Health Organization. (2024, June). Sickle-cell disease fact sheet. https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease
- Centers for Disease Control and Prevention. (2023). Data & statistics on sickle cell disease. https://www.cdc.gov/sickle-cell/data/index.htm


































