Last Updated on November 20, 2025 by Ugurkan Demir
Acute Lymphoblastic Leukemia (ALL) is a cancer of immature lymphoid cells that grow rapidly in the bone marrow. Understanding the pathogenesis of acute lymphoblastic leukemia is key to recognizing how this disease develops and progresses.
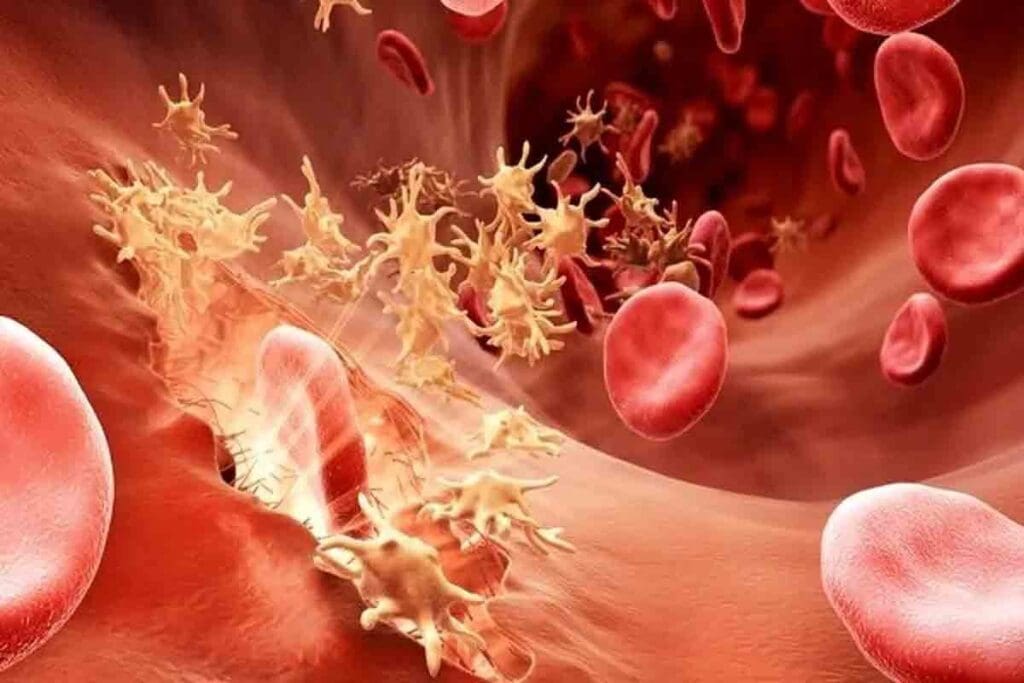
ALL affects both the blood and bone marrow, making it difficult for the body to produce healthy blood cells. The pathogenesis of acute lymphoblastic leukemia involves complex genetic mutations and environmental factors that lead to uncontrolled cell growth. These abnormal lymphoid cells crowd out normal cells, causing anemia, infections, and bleeding issues.
Studying the pathogenesis of acute lymphoblastic leukemia helps scientists and doctors discover better diagnostic tools and targeted treatments. By learning more about the underlying causes and molecular mechanisms of ALL, we can improve patient outcomes and quality of life.

It’s important to understand Acute Lymphoblastic Leukemia (ALL) to find good treatments. ALL is a serious blood cancer where lymphoblasts grow too much.
ALL is divided into types based on several factors. The World Health Organization (WHO) helps sort these types. It looks at the cell type and genetic changes.
The main types are B-cell ALL (B-ALL) and T-cell ALL (T-ALL). B-ALL is more common in kids. Knowing the type helps doctors plan treatment.
| Subtype | Characteristics | Prognosis |
| B-cell ALL | Most common in children, associated with specific genetic abnormalities | Generally favorable with modern treatment protocols |
| T-cell ALL | More common in adolescents and adults, often presents with higher risk features | Historically poorer than B-ALL, but improving with intensified therapy |
ALL symptoms can vary but often include anemia, infections, and bleeding. These happen because the bone marrow fails to work right.
To diagnose ALL, doctors use bone marrow tests and other methods. These help confirm the diagnosis and plan treatment.
The diagnosis involves several steps. Doctors look at blood and bone marrow, check for specific markers, and analyze genes. This helps understand the cancer better.
Knowing how ALL works is key to treating it right.

Acute Lymphoblastic Leukemia (ALL) starts with changes in lymphoid cells’ genes. Knowing how ALL begins helps us find better treatments.
ALL comes from bad changes in cells that make B and T lymphocytes. These changes mess up how lymphoid cells grow.
Genetic changes can affect how cells grow, die, and fix DNA. For example, TP53 and IKZF1 gene mutations are linked to ALL.
The process of ALL turning bad involves many genetic and epigenetic changes. These changes help the bad cells grow and live longer.
These changes often start with chromosomal breaks or other genetic issues. These issues create fusion genes that mess up cell functions.
Clonal evolution is key in ALL. The bad cell group gets more genetic changes over time. This makes the disease worse and can lead to relapse.
Knowing about clonal evolution helps us find ways to stop the disease from coming back. The table below shows important points about clonal evolution in ALL.
| Aspect | Description | Impact on Disease |
| Genetic Mutations | Acquisition of new mutations in leukemic cells | Contributes to clonal evolution and disease progression |
| Selective Pressure | Therapeutic interventions exerting selective pressure on leukemic cells | Drives the emergence of resistant clones |
| Clonal Heterogeneity | Presence of multiple clones within the leukemic cell population | Influences response to therapy and risk of relapse |
The pathogenesis of ALL is complex. It involves genetic changes, epigenetic shifts, and clonal evolution. More research is needed to better understand and treat this disease.
ALL development is tied to key genetic changes. These include chromosomal translocations and gene mutations. Understanding these changes helps us grasp the etiology of Acute Lymphoblastic Leukemia (ALL). We will look into the genetic alterations that lead to ALL.
Chromosomal translocations are a key feature of ALL. They create fusion genes that can start leukemia. For example, the BCR-ABL1 fusion gene, from the t(9;22) translocation, is seen in some ALL cases.
Gene fusions from chromosomal translocations can turn on oncogenes or disable tumor suppressor genes. These changes can greatly affect how the disease progresses and how well it responds to treatment.
The presence of certain gene fusions can dictate the aggressiveness of the disease and guide targeted therapy decisions.
Mutations in genes that control cell cycle, apoptosis, and DNA repair are common in ALL. These mutations help the disease grow and spread. For instance, TP53 gene mutations, a key tumor suppressor, can cause more genetic instability.
The “two-hit hypothesis” helps us understand how Acute Lymphoblastic Leukemia (ALL) starts. It says that both genetic changes before birth and after birth are key to the disease.
This idea says ALL starts with two genetic events. The first happens before birth, and the second after. This idea has really helped us understand how ALL develops.
Prenatal genetic changes are the first hit in the “two-hit hypothesis.” These changes can be chromosomal translocations or other genetic issues. Studies show many kids with ALL have these changes before birth.
Some important prenatal genetic changes include:
The second hit is about secondary mutations that happen after birth. These changes can make cells grow out of control, leading to leukemia.
These mutations can affect many things, like:
Knowing about the “two-hit hypothesis” is key for finding new treatments. It helps us understand how ALL starts and how to stop it.
Dysregulation of molecular pathways is key in Acute Lymphoblastic Leukemia (ALL) development and progression. ALL’s complexity comes from many signaling pathways that are vital for cell function but go wrong in leukemia.
The PI3K/Akt/mTOR pathway controls cell growth, proliferation, and survival. In ALL, it’s often messed up, making leukemic cells hard to kill and grow more. Targeting this pathway is seen as a promising treatment for ALL.
The JAK/STAT pathway is critical and often goes wrong in ALL. It’s involved in cytokine signaling and blood cell production. Mutations or dysregulation in this pathway can make leukemic cells live longer and grow more.
Other pathways like Notch, Wnt/β-catenin, and cell cycle regulators are also messed up in ALL. These disruptions add to ALL’s complexity and variety.
| Pathway | Role in ALL | Therapeutic Potencial |
| PI3K/Akt/mTOR | Enhanced cell survival and proliferation | High |
| JAK/STAT | Abnormal cytokine signaling and hematopoiesis | Moderate to High |
| Notch Signaling | Regulation of cell fate decisions | Moderate |
Grasping the molecular pathways messed up in ALL is vital for better treatments and patient results. Research into these pathways and their interactions will keep finding new targets for therapy.
Epigenetic changes, like DNA methylation and histone modifications, are key in Acute Lymphoblastic Leukemia (ALL). This is true for b cell acute lymphocytic leukemia and childhood acute lymphocytic leukemia. These changes affect gene expression, helping the disease grow and spread.
DNA methylation adds a methyl group to DNA, often at cytosine bases. In ALL, wrong DNA methylation patterns can silence tumor suppressor genes. This helps leukemia grow. Research shows specific methylation patterns are linked to b cell acute lymphocytic leukemia subtypes.
Studying DNA methylation patterns helps us understand ALL’s molecular pathogenesis. It also helps in diagnosis and treatment. For example, some methylation patterns can predict disease prognosis and treatment response.
Histone modifications, like acetylation and methylation, are vital in ALL. They change chromatin structure, affecting gene expression. In childhood acute lymphocytic leukemia, certain modifications control genes for cell growth and survival.
Abnormal histone-modifying enzymes are seen in ALL subtypes, leading to leukemic transformation. Knowing these modifications helps us understand ALL’s development. It also points to new treatment targets.
Non-coding RNAs (ncRNAs), such as microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), are key in ALL. They can be oncogenes or tumor suppressors, depending on their targets. In b cell acute lymphocytic leukemia, certain miRNAs control cell survival and apoptosis pathways.
ncRNA dysregulation affects ALL pathogenesis by altering cell processes like proliferation and drug resistance. Studying ncRNAs in ALL improves our disease understanding. It also opens new therapeutic possibilities.
Environmental exposures are key in the development of ALL. It’s important to know these risk factors. Acute Lymphoblastic Leukemia is a complex disease. It is influenced by both genetic and external factors.
Ionizing radiation is a known risk factor for ALL. This includes exposure from nuclear accidents, medical radiation, and certain industrial settings. Studies have shown that high levels of radiation exposure can significantly increase the risk of leukemia.
Certain chemical exposures have been linked to an increased risk of ALL. These include:
The exact mechanisms by which these chemicals contribute to ALL development are not fully understood.
Some viral infections have been associated with an increased risk of developing ALL. For instance:
“The role of viral infections in the etiology of ALL is an area of ongoing research, with evidence suggesting that certain viruses may trigger or contribute to the development of leukemia in susceptible individuals.”
Understanding these environmental and external risk factors is key. It helps in developing strategies to prevent ALL. It also helps in identifying individuals at higher risk. They may benefit from early screening and intervention.
Some groups face a higher risk of getting Acute Lymphoblastic Leukemia (ALL). This is due to certain genetic and demographic factors. We will look into these high-risk groups and what conditions make them more likely to get ALL.
People with certain genetic syndromes are more likely to get ALL. For example, children with Down syndrome have a higher chance of developing ALL.
Other genetic syndromes that may raise the risk include:
Age, gender, and ethnicity also affect who gets ALL and how well they do.
Age: ALL is most common in kids under 5, with the highest rate between 2 and 3 years. Adults can also get ALL, with age-related genetic changes affecting their chances of recovery.
| Age Group | Incidence Rate | Prognosis |
| 0-4 years | High | Favorable |
| 5-19 years | Moderate | Generally favorable |
| 20+ years | Lower | Variable, often less favorable |
Gender and Ethnicity: Some studies show slight differences in who gets ALL and how well they do, based on gender and ethnicity. But these factors are less important than genetic predispositions and age.
Knowing who is at higher risk is key to catching ALL early and treating it better. By focusing on these high-risk groups, we can make our treatments more effective.
Our study of Acute Lymphoblastic Leukemia (ALL) shows how genetics, epigenetics, and the environment work together. Knowing how acute lymphoid leukemia pathophysiology works is key to finding better ways to diagnose and treat it.
The growth of lymphoblastic leukemia involves many molecular pathways. This includes changes in chromosomes, gene fusions, and mutations in important genes. These changes mess up how cells work, leading to leukemia.
The “two-hit hypothesis” helps us understand how ALL develops. It shows how genetic changes before birth and later mutations work together. Also, things like radiation and some chemicals can cause this disease.
It’s important to understand how these factors interact to improve care for patients. We need to keep studying how genetics and the environment affect lymphoblastic leukemia. We also need to find new treatments that target the specific problems in this disease.
By learning more about acute lymphoid leukemia pathophysiology, we can better manage and treat this complex disease.
Acute Lymphoblastic Leukemia (ALL) is a cancer that affects the blood and bone marrow. It’s caused by too many immature lymphoid cells growing without control.
Symptoms of ALL include feeling very tired, losing weight, and having fever. You might also experience bone pain, easy bleeding, and swollen lymph nodes.
ALL is classified by the World Health Organization (WHO). They look at cell shape, immune markers, and genetic features.
The “two-hit hypothesis” says ALL needs two genetic changes. The first happens before birth, and the second after.
ALL’s genetic changes include chromosomal shifts, gene fusions, and mutations in key genes. These changes mess up normal cell function and lead to leukemia.
Epigenetic changes, like DNA methylation and histone modifications, are key in ALL. They control gene expression and affect how cells behave.
Yes, exposure to radiation, some chemicals, and viruses can raise the risk of getting ALL.
Certain genetic syndromes, like Down syndrome, make people more likely to get ALL.
Age, gender, and ethnicity can affect who gets ALL and how well they do. Some groups are more at risk.
Knowing how ALL starts is key to finding better ways to diagnose and treat it.
B cell Acute Lymphocytic Leukemia is a type of ALL. It’s when B cell lymphoblasts grow too much.
Doctors use a mix of clinical checks, lab tests, and bone marrow exams to spot ALL.
Acute Lymphoblastic Leukemia is a cancer where lymphoid cells grow too much in the bone marrow and blood.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!