Last Updated on November 20, 2025 by Ugurkan Demir

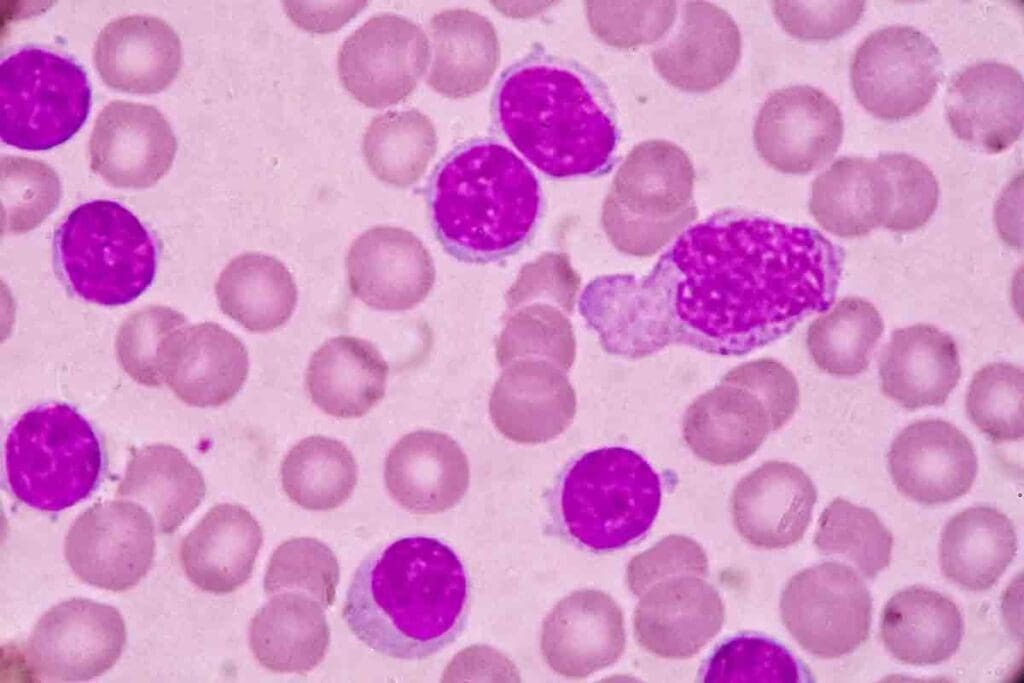
Getting a diagnosis of Acute Lymphoblastic Leukemia (ALL) can feel overwhelming. At Liv Hospital, we’re here to guide and support you through every step of your journey. ALL is a fast-growing cancer of the blood and bone marrow that develops when too many immature lymphocytes form and crowd out healthy cells.
Understanding the difference between acute lymphocytic vs lymphoblastic leukemia is essential for accurate diagnosis and treatment planning. While both terms are often used interchangeably, “lymphocytic” refers to the type of white blood cells affected, and “lymphoblastic” describes their immature, rapidly dividing nature.
At Liv Hospital, our expert team uses the latest research and technology to create personalized treatment plans. We’re dedicated to helping you understand your condition and make informed choices about care. No matter where you are in your journey, we’re here to provide support, compassion, and world-class medical expertise.

At Liv Hospital, we know how vital it is to teach patients about acute leukemia. This cancer grows fast if not treated right away. It affects the blood and bone marrow, making it key to grasp its basics for better treatment choices.
Acute leukemia is when immature blood cells grow too much in the bone marrow. This messes up the normal blood cell making process. It’s a serious condition that needs quick action because it affects blood cell production a lot.
Acute leukemia is different from chronic leukemia because it grows fast. Chronic leukemia moves slowly. The main difference is in the blood cells affected and how fast they grow. Acute leukemia makes lots of immature cells quickly, while chronic leukemia builds up mature cells slowly.
Acute leukemia has a big impact on the blood and bone marrow. It makes too many immature blood cells, causing problems like anemia, infections, and bleeding issues. Knowing how acute leukemia affects the body is vital for finding good treatments.
The terms ALL can be confusing. Both ‘lymphocytic’ and ‘lymphoblastic’ describe the same disease. We will look into where these terms come from and why they are used the same way in medicine.
The words ‘lymphocytic’ and ‘lymphoblastic’ come from the cells affected by the disease. ‘Lymphocytic’ talks about lymphocytes, important white blood cells for our immune system. ‘Lymphoblastic’ is about lymphoblasts, which are young cells that grow into lymphocytes.
Knowing where these terms come from helps us understand their use. The disease is marked by the growth of lymphoblasts, which are young lymphocytes.
Even though ‘lymphocytic’ and ‘lymphoblastic’ have slight differences, they both describe ALL. This is because of the disease’s nature and the cells it impacts.
The medical world agrees that ‘Acute Lymphocytic Leukemia’ and ‘Acute Lymphoblastic Leukemia’ mean the same thing. Which term is used often depends on where you are or who you’re talking to.
We will stick to calling it Acute Lymphocytic Leukemia (ALL) in this article. This is because both terms are used the same way by doctors.
Understanding Acute Lymphoblastic Leukemia (ALL) is key to knowing how it grows and how to treat it. ALL is a blood and bone marrow cancer. It’s caused by too many immature lymphocytes, called lymphoblasts.
ALL starts in the bone marrow, where blood cells are made. It happens when lymphoid precursors, cells meant to become lymphocytes, turn cancerous. These bad cells fill the bone marrow and stop normal blood cells from being made.
“The bone marrow is the spongy tissue inside some of your bones, such as your hips and thighbones, which produces blood cells,” explains the complex process of blood cell production. When lymphoid precursors become cancerous, they crowd out the normal cells, leading to a range of complications.
Lymphocytes are a type of white blood cell important for the immune system. They fight infections and are split into B cells and T cells. In ALL, these cells are affected early, turning into lymphoblasts that can’t mature right. These immature cells in the bone marrow and blood are what make up ALL.
Lymphoblasts are immature cells found in the bone marrow. In ALL, these cells are bad and grow too much, causing the disease to get worse.
Genetics are a big part of ALL. Some genetic problems can make people more likely to get the disease. For example, problems with genes that control cell growth can cause lymphoid cells to grow too much.
Knowing about these genetic factors helps doctors find better treatments for ALL.
ALL has different subtypes, mainly based on where they start. They can come from B-cell or T-cell lymphoid precursors. Knowing these types helps doctors predict how well a patient will do and what treatment to use.
ALL can start from either B-cell or T-cell lymphoid precursors. B-cell ALL is more common in kids and usually has a better outlook with the right treatment. T-cell ALL often has more white blood cells and can spread outside the bone marrow, leading to a worse prognosis.
“The difference between B-cell and T-cell ALL is key,” studies say. It affects how doctors treat and what the patient’s chances are.
The FAB system was used to sort ALL by how it looks under a microscope. It split ALL into L1, L2, and L3 types. Even though newer systems have come along, FAB is important for understanding ALL.
The WHO system is more modern and detailed. It looks at genetics and molecular features, not just how cells look. It groups ALL by cell type and genetic changes, giving a clearer picture of the disease.
The WHO system has types like B lymphoblastic leukemia/lymphoma, NOS and T lymphoblastic leukemia/lymphoma. This helps doctors make more accurate diagnoses and treatment plans.
How ALL is classified affects its outlook. Some genetic changes mean better or worse chances. Knowing these helps doctors plan treatments based on each patient’s risk.
By looking at cell origin, genetics, and other factors, doctors can predict outcomes better. This helps in creating targeted treatments for ALL patients.
Understanding Acute Lymphocytic Leukemia (ALL) is key to knowing its impact. ALL affects different groups in various ways.
ALL causes about 6,540 new cases each year in the U.S. This shows why we need to keep studying it.
ALL’s occurrence changes with age and other factors. Let’s look at the numbers more closely.
| Age Group | Incidence Rate (per 100,000) |
| 0-19 years | 4.1 |
| 20-39 years | 1.4 |
| 40-59 years | 1.1 |
| 60+ years | 1.4 |
ALL mostly hits kids under 20. But it also affects adults, who face different challenges.
Children: ALL is the top childhood cancer, making up 25% of all cancers in kids. It’s most common between 2 and 5 years old.
Adults: ALL in adults is rarer but more aggressive. It’s more common after 60.
Several factors increase the risk of ALL. These include genetic conditions, certain chemicals, and radiation.
Knowing these risk factors helps in early detection and treatment of ALL.
ALL is marked by too many immature lymphocytes. It shows symptoms that need quick medical help. Spotting these signs early is key for a good treatment.
Symptoms of ALL vary but include fatigue, pale skin, and frequent infections. Easy bruising and bone pain are also common. Some notice swollen lymph nodes too.
These signs happen because leukemic cells fill the bone marrow. This reduces normal blood cell production.
Diagnosing ALL involves a physical check, medical history, and tests. Doctors look for swollen lymph nodes, spleen, or liver.
The first step is a complete blood count (CBC). It checks blood cell levels.
Lab tests are vital for diagnosing ALL. A bone marrow biopsy and aspiration are key. They check bone marrow cells for leukemic cells.
Imaging like chest X-rays or CT scans might be used. They look for infections or other issues.
Distinguishing ALL from other conditions is important. This is called differential diagnosis. It’s about finding the right diagnosis.
A detailed diagnostic process helps doctors accurately diagnose ALL. This leads to the right treatment plan.
At Liv Hospital, we use the latest treatments for Acute Lymphocytic Leukemia (ALL). Each patient gets a treatment plan that fits their needs. This approach has greatly improved how we treat ALL.
Chemotherapy is key in treating ALL. We mix different drugs to help patients get better and stay better. The exact treatment plan depends on the patient’s age, health, and type of ALL.
Key Chemotherapy Agents:
Targeted therapies are also important in treating ALL. They aim at specific molecules in leukemia cells. This makes treatment more precise.
Examples of targeted therapies include:
Stem cell transplantation is an option for some ALL patients. It replaces the patient’s bone marrow with healthy stem cells from a donor. This is often for those at high risk of relapse or with relapsed disease.
| Treatment Aspect | Children | Adults |
| Chemotherapy Intensity | Generally more intensive | May be less intensive due to comorbidities |
| Targeted Therapies | Often used in combination with chemotherapy | Used based on specific genetic markers |
| Stem Cell Transplantation | Considered for high-risk or relapsed cases | More commonly considered due to higher risk |
Children and adults with ALL are treated differently. This is because of differences in disease biology and how well they can handle treatment. Children usually do better and can handle stronger treatments.
Adults might have health issues that make it hard to handle strong treatments. So, their treatment plans are more tailored to their needs.
At Liv Hospital, we focus on giving the best care for ALL patients. We use the newest treatments and care methods to help them.
Living with Acute Lymphocytic Leukemia (ALL) means more than just treatment. It’s about having a support system for the physical, emotional, and financial challenges. At Liv Hospital, we offer top-notch healthcare and support for our international patients.
It’s key to manage ALL treatment side effects to keep patients’ quality of life high. Side effects can range from fatigue and nausea to serious issues like infections and organ damage.
We suggest a few ways to tackle these side effects:
After ALL treatment, ongoing health checks are vital. Regular check-ups and tests help spot any signs of relapse or long-term side effects early.
Our care plan includes:
| Monitoring Aspect | Description | Frequency |
| Blood Tests | To check for signs of relapse or treatment side effects. | Regularly as advised by the healthcare provider. |
| Imaging Tests | To monitor the condition of organs and detect any abnormalities. | As necessary based on patient condition. |
| Physical Examinations | To assess overall health and detect any signs of complications. | At each follow-up visit. |
ALL diagnosis and treatment can deeply affect patients and their families. It’s important to offer psychosocial support to help them cope with emotional and social challenges.
“The emotional support we received during my daughter’s treatment for ALL was invaluable. It helped us navigate the challenging journey with more confidence and less fear.” – A patient’s family member.
We provide counseling, support groups, and educational resources to help patients and families through this tough time.
Treating ALL can be costly, and dealing with finances and insurance can be tough. We help patients and families find financial aid and understand their insurance options.
Our support includes:
At Liv Hospital, we aim to improve healthcare quality and patient experience. We’re committed to supporting our patients every step of the way, ensuring they get the care they need.
Acute Lymphoblastic Leukemia (ALL) is a complex condition. Knowing the difference between acute lymphocytic and lymphoblastic leukemia is key for patients and their families. At Liv Hospital, we offer top-notch healthcare and support for international patients.
The terms acute lymphocytic and lymphoblastic leukemia are often mixed up. They both describe the same condition: the fast growth of immature white blood cells. The real difference is in the words used, not the condition itself.
ALL is a serious condition that needs quick and effective treatment. Our hospital aims to be a leader in medical care and research. We hope this info helps you understand ALL and the care we offer for both types of leukemia.
If you’re looking for advanced medical care and support, Liv Hospital is here for you. Knowing about ALL is the first step to managing and treating it effectively.
Acute Lymphoblastic Leukemia (ALL) is a fast-growing cancer. It affects the blood and bone marrow. It’s caused by too many immature lymphocytes.
‘Lymphocytic’ and ‘lymphoblastic’ are often used to mean the same thing. They both describe Acute Lymphoblastic Leukemia (ALL).
Acute leukemia is more aggressive and has immature cells. It needs quick medical attention. Chronic leukemia is slower and has mature cells.
Symptoms include feeling tired, pale skin, infections, and easy bruising. These happen because of low blood cell counts.
Doctors use physical exams, lab tests, and imaging to diagnose ALL. This includes blood counts and bone marrow biopsies.
Treatments include chemotherapy, targeted therapies, and stem cell transplants. Treatment plans vary for children and adults.
Genetics are key in ALL. Certain genetic changes can lead to the disease.
ALL is classified by cell type (B-cell vs T-cell) and other features. The French-American-British (FAB) and World Health Organization (WHO) systems are used.
Support includes managing side effects, long-term health checks, and psychosocial help. There are also financial and insurance resources.
In the U.S., ALL causes about 6,540 new cases each year. It affects both kids and adults.
ALL causes too many immature blood cells in the bone marrow. This disrupts normal blood cell production.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!