When you have rectal cancer, Anterior Perineal Resection (APR) is a key surgery. It’s used when saving the muscles around the anus is not possible. Get 7 key facts about anterior perineal resection (APR). Understand this critical surgery for rectal cancer, its risks, and recovery.
APR removes the lower colon, rectum, and anus to get rid of cancer. It’s a big part of colon surgery. It helps patients with rectal or anal cancer.
Liv Hospital is known for its care in treating rectal cancer with APR. Knowing about this surgery is important for patients and their families.

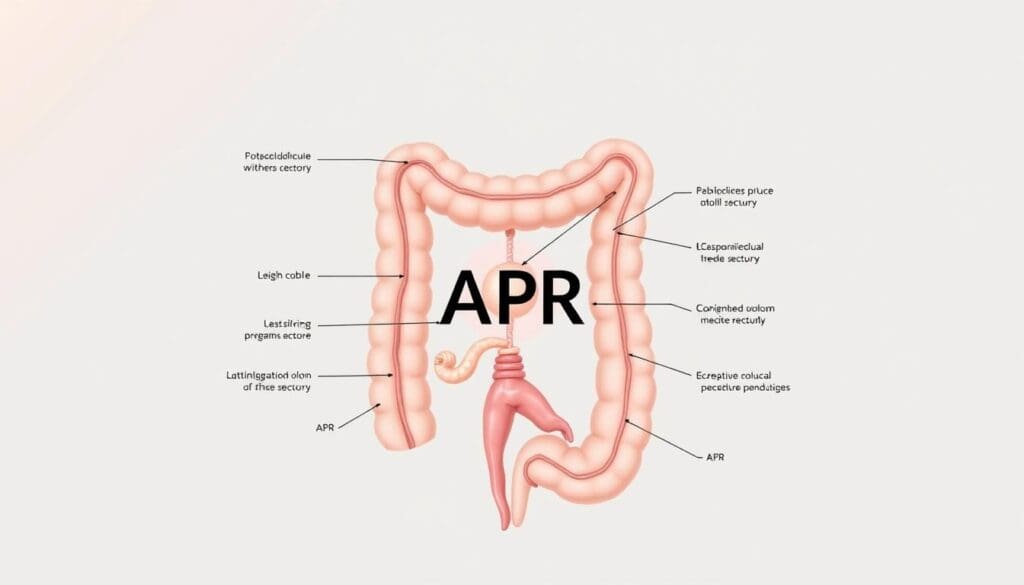
Anterior Perineal Resection, or APR, is a surgery mainly for rectal cancer. It’s used for tumors in the lower rectum. This surgery is complex and involves a team for care before and after surgery.
APR removes the anus, rectum, and part of the sigmoid colon. It’s done through the belly and bottom. This is for cancers near the anus where saving the sphincter isn’t possible.
The Miles Procedure was first described by W.E. Miles in the early 1900s. It was the main treatment for rectal cancer for many years. The Miles Procedure was a key moment in treating rectal cancer.
“Anterior Perineal Resection” and “Abdominoperineal Resection” are often mixed up. But, APR means surgery through the belly and bottom. Knowing the difference helps doctors talk better and understand each other.
| Aspect | APR (Abdominoperineal Resection) | LAR (Low Anterior Resection) |
| Surgical Approach | Both abdominal and perineal incisions | Primarily abdominal incision |
| Tumor Location | Lower rectum, close to the anus | Rectum, with possible sphincter saving |
| Outcome | Permanent colostomy | Potential for normal bowel function |
APR is important for colorectal surgery, even with new options. It’s chosen based on the tumor’s location, stage, and the patient’s health.
The APR acronym is used a lot in medicine, mainly in colon and rectal surgery. It stands for abdominoperineal resection, a big surgery.
This surgery removes the rectum and anus, making a permanent colostomy. Knowing about APR is key for both patients and doctors.
In colorectal surgery, APR is a big deal. It’s needed for treating low rectal tumors or when saving the sphincter isn’t possible.
In medical talks and studies, APR comes up a lot. It’s about treating rectal cancer and how surgeries go.
In colon and rectal surgery, APR is very important. It’s a complex surgery that needs skilled surgeons.
Using terms like APR helps doctors talk clearly. It makes sure patients get the same care everywhere.
| Context | Significance | Implications |
| Colon and Rectal Surgery | Represents abdominoperineal resection | Involves removal of rectum and anus, creation of permanent colostomy |
| Medical Literature | Frequently used in discussions on rectal cancer treatment | Impacts surgical decision-making and patient outcomes |
| Clinical Practice | Standardized terminology for clear communication | Ensures consistent care among healthcare providers |
Choosing Anterior Perineal Resection (APR) for rectal cancer depends on several factors. These include the tumor’s location and the patient’s health. APR is a big surgery that’s considered when other options won’t work.
Low rectal tumors are close to the anal sphincter. This makes surgery tricky. APR is needed to remove the cancer and the surrounding tissues.
Doctors decide on APR after looking at images and assessing the patient. For tumors near the sphincter, APR is usually the best choice.
When cancer invades the sphincter, saving it during surgery is hard. APR is a definitive treatment in these cases. It removes the tumor completely.
Keeping the sphincter intact is important for quality of life. But when it’s risky, APR is chosen.
Patient health and preferences are key in choosing APR. The cancer’s stage and location also matter. Patients with health issues might be better candidates for APR.
Being able to handle a permanent colostomy is also important. Thanks to better ostomy care, life with a colostomy is easier now.
In summary, deciding on APR for rectal cancer involves many factors. Understanding when it’s needed helps doctors offer the best care.
Knowing the anatomy of rectal cancer is key for planning treatment. The rectum is about 12 cm to 15 cm long. It’s in the pelvic area, near the sacrum and coccyx. This location makes treating rectal cancer complex.
Staging and knowing where the cancer is are vital for treatment. The stage shows how deep the tumor is, if it’s in lymph nodes, and if it has spread. Where in the rectum the tumor is also affects treatment choices.
The surgery for rectal cancer depends on the tumor’s location and size. Surgeons must think about how close the tumor is to important areas like the anus, nerves, and blood vessels.
By looking at these details, doctors can make a treatment plan that works best for each patient with rectal cancer.
APR surgery is a detailed process to remove the rectum, anal canal, and sphincter complex. This leads to a permanent colostomy. It’s mainly for patients with low rectal tumors where saving the sphincter is not possible.
Before APR surgery, patients go through detailed preparation. They have imaging studies like MRI and CT scans. These help see how big the tumor is and its position.
Accurate staging is key for planning the surgery and if they need therapy before surgery. Patients also get nutritional counseling to improve their health before surgery. This helps with healing and recovery. They learn about the permanent colostomy and how to manage it.
The APR surgery uses a combined abdominal and perineal approach. The abdominal part involves moving the sigmoid colon and rectum. It also includes stopping the inferior mesenteric artery and finding the ureters.
The perineal part is about dissecting around the anus and removing the rectum and anal canal. The team works carefully to remove the tumor safely.
Meticulous dissection is done to get clear margins around the tumor. This is important in the distal rectum and sphincter complex. The team aims for a safe and effective resection.
Creating a permanent colostomy is a key part of APR surgery. The sigmoid colon is brought out through the abdomen. The colostomy is then made at the skin level.
Patients learn about colostomy care and management. This helps them adjust to this new part of their life.
After removing the rectum and anal canal, the perineal wound is closed. The method of closure can vary, like primary closure or flaps. Postoperative wound care is vital to avoid infections or wound opening.
Good wound care means watching for infection signs, managing pain, and helping healing. Patients get instructions on postoperative care for recovery at home.
In the world of rectal cancer surgery, APR is a big deal. It’s part of a trend towards keeping the sphincter intact. The choice between APR and sphincter-sparing techniques depends on many things. These include where the tumor is, its stage, and what the patient wants.
Low Anterior Resection (LAR) is a way to treat rectal cancer without harming the sphincter. It removes the cancerous part of the rectum and then connects the rest. This method is chosen when the tumor isn’t too close to the sphincter, helping keep bowel function normal.
LAR Technique Advantages:
Choosing between APR and LAR is complex. Several factors play a role:
It’s important to do a detailed check-up and imaging to decide the best surgery.
When picking a surgery for rectal cancer, quality of life matters a lot. APR might be needed for tumors near the sphincter. But it means a permanent colostomy, which can really affect a patient’s life.
Quality of life factors to consider:
Looking at APR and LAR in terms of quality of life:
| Surgical Aspect | APR | Sphincter-Sparing (LAR) |
| Permanent Colostomy | Yes | No |
| Bowel Function Preservation | No | Yes |
| Potential for Complications | Similar risks, including wound complications | Similar risks, with possible anastomotic leak |
The table shows the main differences between APR and LAR. It shows why treatment plans need to be tailored for each patient with rectal cancer.
The journey to recovery after APR surgery for rectal cancer is complex. It involves both physical and emotional challenges. Knowing what to expect can help patients prepare and navigate their recovery better.
Patients usually spend 5 to 7 days in the hospital after APR surgery. This time can vary based on their health and any complications.
In the hospital, patients get pain management, wound care, and learn about colostomy management. The team also watches for complications like infection or colostomy issues.
After leaving the hospital, patients recover at home for several weeks. Having a support system is key for daily tasks and colostomy care.
Patients can usually return to normal activities in 6 to 8 weeks. But, it may take longer to fully recover and adjust to the colostomy.
Adapting to a permanent colostomy is a big challenge after APR surgery. Patients must learn to manage their colostomy, including changing the appliance and dealing with leakage or odor.
Effective colostomy care is vital for post-APR recovery. Patients get resources and support to manage their colostomy well.
Rehabilitation after APR surgery goes beyond physical recovery. It also includes psychological support. Patients may feel anxious, depressed, or experience grief and adjustment disorders.
A good rehabilitation plan includes physical therapy to regain strength and mobility. It also includes counseling or support groups for emotional and psychological challenges.
| Aspect of Recovery | Timeline | Key Considerations |
| Hospital Stay | 5-7 days | Monitoring, pain management, wound care, colostomy education |
| Home Recovery | 6-8 weeks | Support system, colostomy care, gradual return to activities |
| Colostomy Adjustment | Ongoing | Learning colostomy management, dealing with issues |
| Physical Rehabilitation | Variable | Physical therapy, regaining strength and mobility |
| Psychological Rehabilitation | Variable | Counseling, support groups, addressing emotional challenges |
APR is a common treatment for rectal cancer. But, it comes with several post-operative complications. It’s important for patients and healthcare providers to know about these complications to manage them well.
APR surgery can lead to short-term complications. These include:
A study in the Journal of Surgical Oncology found that
“The overall morbidity rate after APR can be as high as 40%, with wound complications being the most common issue.”
APR surgery can save lives but affects many aspects of life. It impacts physical function, psychological well-being, and social life.
| Aspect | Impact | Management |
| Physical Function | Reduced mobility, ostomy complications | Physical therapy, ostomy care education |
| Psychological Well-being | Body image changes, depression | Counseling, support groups |
| Social Life | Changes in social interactions, intimacy issues | Counseling, support groups |
A patient advocacy group noted that
“Living with a permanent colostomy requires significant lifestyle adjustments, but with proper support and education, patients can lead fulfilling lives.”
New techniques in APR aim to improve outcomes and quality of life. Minimally invasive surgery and ERAS protocols are being used to reduce complications.
APR is linked to significant morbidity, including urinary and sexual dysfunction. But, with careful patient selection and post-operative care, many complications can be managed.
Managing complications after APR surgery needs a team effort. This includes surgical expertise, nursing care, and patient education. Understanding complications and taking proactive steps can improve patient outcomes and quality of life.
New techniques in APR surgery are changing how we treat colorectal cancer. These changes bring hope to both patients and doctors. The goal is to improve results, reduce recovery time, and make patients’ lives better.
Minimally invasive surgery is making APR procedures better. It uses smaller cuts, causing less damage and pain. This means patients can heal faster and get back to their lives sooner.
Laparoscopic APR is a popular method. It uses a laparoscope for small incisions. This approach is gentler and lets doctors see better, which can lead to more precise surgery.
ERAS protocols are key to better APR surgery recovery. They include pre-op advice, nutrition plans, and early movement after surgery. These steps help patients heal faster and feel better.
Using ERAS, doctors can lower surgery stress and risks. It also makes patients happier and leaves them in the hospital less time.
New tech is making APR surgery better for fighting cancer. Tools like intraoperative navigation systems and fluorescence-guided surgery help doctors find and remove tumors better. This could lead to better survival rates.
Robotic surgery is also improving APR. Robots give doctors more control and clear views, making complex surgeries safer and more effective.
The future of APR surgery looks bright with new tech and techniques. Research into AI, machine learning, and better imaging could make surgery even more precise. This could lead to better results for patients.
As APR surgery keeps getting better, patients will have more chances for successful treatment and recovery from colorectal cancer.
Anterior Perineal Resection (APR) is a key surgery for treating rectal cancer, mainly for low rectal tumors. Even with more sphincter-sparing surgeries, APR is vital in today’s treatments.
APR is needed when saving the sphincter isn’t possible. It removes the tumor and affected tissue. Thanks to new surgical methods and care, patients do better after APR.
Choosing APR in modern treatments depends on the tumor’s location, stage, and the patient’s health. It shows a focus on treating cancer well while keeping the patient’s quality of life high.
As treatments for rectal cancer keep improving, APR stays a key part of surgery. It offers a reliable way to handle tough cases.
Anterior Perineal Resection, also known as Abdominoperineal Resection (APR), is a surgery for rectal cancer. It’s used for tumors near the anus. The procedure removes the anus, rectum, and part of the sigmoid colon. It also creates a permanent colostomy.
APR removes the anal sphincter and creates a permanent colostomy. LAR tries to keep the sphincter and normal bowel function. The choice between APR and LAR depends on the tumor’s location, size, and stage, and the patient’s health.
APR surgery can lead to infection, bleeding, and bowel obstruction. It can also cause urinary or sexual problems. Long-term issues might include colostomy problems and psychological impacts.
Recovery from APR surgery varies. Patients usually stay in the hospital for several days. At home, recovery can take weeks to months. They must adjust to a permanent colostomy and manage any complications.
New APR techniques include minimally invasive surgery and Enhanced Recovery After Surgery (ERAS) protocols. Robotic surgery is also being used. These aim to reduce recovery time, minimize complications, and improve outcomes.
APR can greatly affect a patient’s quality of life due to the permanent colostomy. While it saves lives, patients must adapt to their new situation. They may face changes in body image, bowel habits, and lifestyle.
Yes, alternatives include sphincter-sparing operations like Low Anterior Resection (LAR). The choice depends on the tumor and the patient’s condition. Neoadjuvant therapies may also be used to shrink tumors, making sphincter preservation possible.
APR is mainly known in colorectal surgery. But, it can mean different things in other medical fields. In colon and rectal surgery, APR is a specific term for this procedure.
Hawkins, A. T., Albutt, K., Wise, P. E., Alavi, K., Sudan, R., Kaiser, A. M., & The Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. (2018). Abdominoperineal Resection for Rectal Cancer in the Twenty-First Century: Indications, Techniques, and Outcomes. Diseases of the Colon & Rectum, 61(10), 1150–1162. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131379/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!