
A blocked bile duct can cause serious health problems. But, with the right care, finding solutions is easier than before. At places like Liv Hospital, we offer top-notch care and focus on our patients.
It’s important to know how the bile duct system works. We’ll show you how to fix a blocked bile duct. We’ll cover what causes it, its symptoms, and how to treat it.
Our detailed guide will help you every step of the way. You’ll get the care and support you need.
Key Takeaways
- Knowing the causes and symptoms of a blocked bile duct is key to treating it.
- If not treated, a blocked bile duct can cause serious health issues.
- Getting expert care and patient-focused treatment is vital.
- There are many ways to treat it, including surgery and non-surgical methods.
- Places like Liv Hospital offer trusted care and a full range of services.
Understanding the Bile Duct System and Its Function
To understand a blocked bile duct, we need to know about the biliary system. This system includes ducts and organs that are key to our digestion. It makes, stores, and moves bile, which helps digest fats and absorb vitamins.
Anatomy of the Biliary System
The biliary system has the liver, gallbladder, and bile ducts. The liver makes bile, which goes to the gallbladder. The bile ducts join to form the common bile duct. This duct carries bile to the small intestine for digestion.
Normal Bile Flow and Its Importance
Good bile flow is key to digestive health. Bile breaks down fats for enzymes to digest. It also helps absorb vitamins A, D, E, and K. Any problem with bile flow can cause digestive issues and serious health problems.
How Blockages Affect Overall Health
A blockage in the bile duct, or bile duct blockage, is serious. It can cause jaundice, with yellow skin and eyes. Long-term blockage can harm the liver and even cause liver failure if not treated.
Common Causes of Blocked Bile Ducts
Knowing why bile ducts get blocked is key to treating them right. Many things can cause a blockage. These can be grouped into a few main areas.
Gallstones and Biliary Sludge
Gallstones are a big reason for bile duct blockages. These stones can move from the gallbladder into the bile duct. This causes a blockage. Biliary sludge, a mix of bile, cholesterol, and other stuff, can also block the bile duct.
Key factors contributing to gallstone formation include:
- Cholesterol supersaturation
- Bile stasis
- Nucleation factors
Tumors and Malignancies
Tumors, both good and bad, can block the bile duct. Pancreatic cancer, cholangiocarcinoma, and ampullary cancer are examples. These cancers can block the bile duct.
“The presence of a tumor in the bile duct or surrounding areas can significantly impact the flow of bile, leading to obstruction and potentially severe complications.”
Medical Expert, Gastroenterologist
Strictures and Inflammatory Conditions
Strictures, or narrowing of the bile duct, can happen due to chronic inflammation, injury, or infection. Conditions like primary sclerosing cholangitis can cause fibrosis and stricture. This leads to bile duct obstruction.
Iatrogenic and Traumatic Causes
Iatrogenic causes, like surgical complications or endoscopic procedures, can damage the bile duct. Traumatic injuries to the abdomen can also harm the bile duct. This leads to obstruction.
| Cause | Description | Potential Complications |
| Gallstones | Stones migrating from the gallbladder | Infection, pancreatitis |
| Tumors | Benign or malignant growths | Obstruction, metastasis |
| Strictures | Narrowing due to inflammation or injury | Cholangitis, cirrhosis |
Understanding these causes helps doctors create better treatment plans. This way, they can effectively address bile duct blockages.
Recognizing Symptoms of a Blocked Bile Duct
It’s key to spot the signs of a blocked bile duct early. A blocked bile duct can cause serious health problems if not treated quickly. We’ll look at the symptoms, from the first signs to severe cases that need urgent care.
Early Warning Signs
The first signs of a blocked bile duct are often subtle but important. Some early symptoms include:
- Jaundice: Yellow skin and eyes from too much bilirubin.
- Fatigue: Feeling very tired or weak.
- Loss of Appetite: Eating less or feeling full too soon.
- Nausea and Vomiting: Feeling sick or vomiting, often after eating fatty foods.
These signs might mean you have a bile duct problem. Don’t ignore them. If you notice any, see a doctor right away.
Severe Symptoms Requiring Immediate Medical Attention
As the blockage gets worse, symptoms can get much worse. Look out for:
- Severe Abdominal Pain: Sharp pain in the upper right belly that might spread to the back.
- High Fever: A high fever, often with chills.
- Dark Urine: Urine that’s darker than usual.
- Pale Stools: Stools that are pale or clay-colored.
If you have these severe symptoms, get medical help fast. They could mean a serious infection or other serious problems.
Complications of Untreated Biliary Blockages
Ignoring a blocked bile duct can lead to serious issues. These include:
- Biliary Cirrhosis: Scarring of the bile ducts that can harm the liver.
- Cholangitis: Infection of the bile duct, which can be deadly if not treated quickly.
- Pancreatitis: Inflammation of the pancreas, causing severe belly pain.
Knowing these risks shows why it’s so important to catch the symptoms early and get medical help fast.
Diagnostic Procedures for Bile Duct Blockages
To find out if there’s a blockage in the bile ducts, we use several methods. These include lab tests, imaging, and taking tissue samples. These tools help us figure out what’s causing the blockage and how bad it is.
Laboratory Tests and Biomarkers
Lab tests are key in spotting bile duct blockages. We check blood for signs of liver health and blockages.
- Liver Enzymes: High levels of liver enzymes like ALT and AST mean liver damage or blockage.
- Bilirubin Levels: Too much bilirubin can turn your skin yellow and is a sign of blockage.
- Alkaline Phosphatase (ALP): If ALP is too high, it might mean there’s a blockage in the bile ducts.
| Laboratory Test | Normal Range | Significance of Bile Duct Blockage |
| ALT | 0-40 U/L | Elevated levels indicate liver damage |
| AST | 0-40 U/L | Elevated levels indicate liver damage or other conditions |
| Bilirubin | 0.1-1.2 mg/dL | High levels cause jaundice and indicate bile duct blockage |
| ALP | 30-120 U/L | Elevated levels suggest cholestasis |
Imaging Techniques
Imaging is essential for seeing the bile ducts and finding blockages. We use different methods to diagnose and plan treatment for blockages.
- Ultrasound: It’s often the first choice because it’s non-invasive. It can spot bile duct swelling and gallstones.
- CT Scan: It gives detailed images, helping us find where and why the bile duct is blocked.
- MRI/MRCP: MRCP is great for seeing the bile and pancreatic ducts without needing contrast.
- ERCP: Though it’s more invasive, ERCP can both diagnose and treat blockages.
Tissue Sampling and Analysis
Sometimes, we need to take tissue samples to find out why the bile duct is blocked. This is important if we think it might be cancer.
- Biopsy: We can get tissue samples during ERCP or other procedures.
- Cytology: Examining cells from bile or ERCP can help spot cancers.
By using lab tests, imaging, and tissue samples, we can accurately diagnose bile duct blockages. Then, we can plan the best treatment.
Drainage of Bile Duct: Treatment Approaches Overview
Draining the bile duct is key to managing symptoms and complications from blockages. Blockages can cause jaundice, infection, and even liver damage. We will explore the treatment options for draining a blocked bile duct.
When Drainage Becomes Necessary
Drainage is needed when a blockage stops normal bile flow. This can be due to gallstones, tumors, or strictures. Symptoms like jaundice, itching, and pain often mean it’s time for action. We’ll discuss when drainage is needed and how doctors find the cause.
Types of Drainage Procedures
There are several ways to manage bile duct blockages. These include:
- Endoscopic Drainage: Uses an endoscope to clear the blockage.
- Percutaneous Biliary Drainage: A minimally invasive method using a catheter.
- Surgical Drainage: Sometimes surgery is needed to bypass or remove the blockage.
We’ll look at each procedure’s benefits and risks. This helps patients understand their options.
Selecting the Appropriate Intervention
Choosing the right procedure depends on several factors. These include the blockage’s cause and location, the patient’s health, and past treatments. A team of doctors works together to decide the best approach. We’ll explain how they make this choice.
Preparing for a Drainage Procedure
Getting ready for a procedure is important. This includes tests, imaging, and patient education. We’ll guide patients through the preparation steps. This ensures they are informed and comfortable with what’s to come.
| Procedure | Indications | Benefits | Potential Complications |
| Endoscopic Drainage | Blockages accessible via an endoscope | Minimally invasive, quick recovery | Bleeding, infection, pancreatitis |
| Percutaneous Biliary Drainage | Blockages not accessible endoscopically | Effective for complex blockages | Catheter-related complications, infection |
| Surgical Drainage | Complex or recurrent blockages | Long-term solution | Surgical risks, longer recovery |
It’s important for patients to understand their options for bile duct blockages. By working with healthcare providers, patients can make informed decisions. This leads to the best possible outcomes.
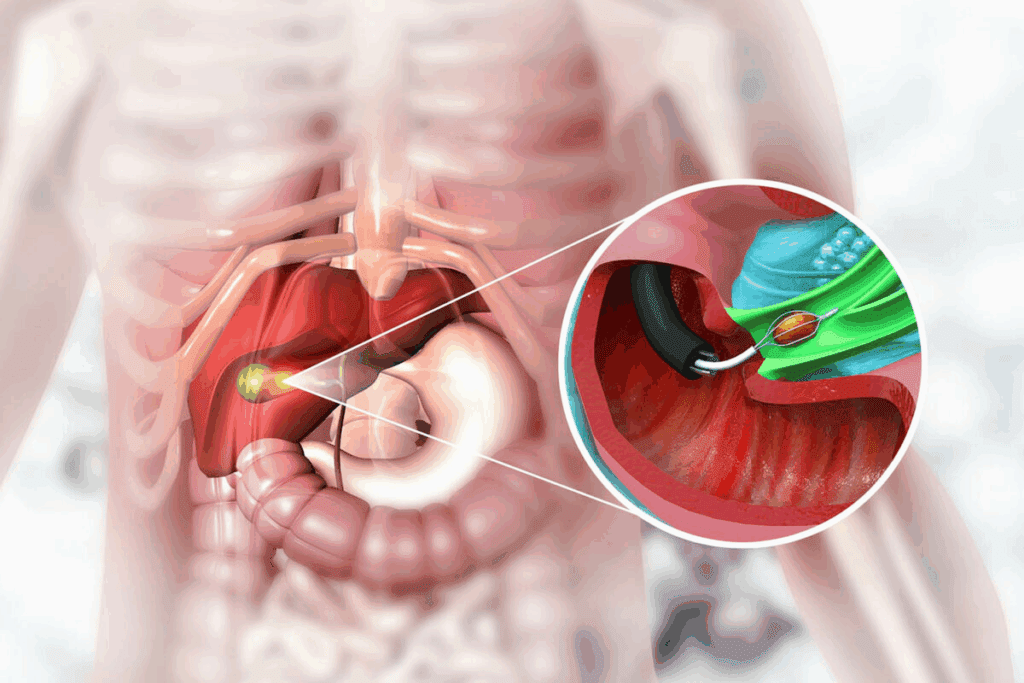
Endoscopic Techniques for Unclogging Bile Ducts
Endoscopic methods are often the first choice for clearing blocked bile ducts. They are less invasive and have a high success rate. These techniques have greatly improved treatment for bile duct obstructions, leading to faster recovery times than surgery.
ERCP Procedure: Step-by-Step Guide
Endoscopic Retrograde Cholangiopancreatography (ERCP) combines endoscopy and fluoroscopy. It’s used to diagnose and treat bile and pancreatic duct issues. We start by sedating the patient and then insert an endoscope through the mouth.
Next, we inject a contrast agent into the bile ducts. This helps us see any blockages or problems on an X-ray. We can then do interventions like sphincterotomy to remove stones or debris.
Stent Placement for Bile Duct Drainage
Stent placement is key for bile duct drainage during ERCP. It keeps the bile duct open, allowing bile to flow into the intestine. This is vital for patients with certain obstructions or those who can’t have surgery.
The type of stent used depends on the patient’s condition and the obstruction. We often choose metal stents because they’re more durable and less likely to block.
Stone Extraction and Debris Removal
Stone extraction is a critical part of ERCP. We use tools like balloon catheters and baskets to remove stones. For big stones, we might need to break them down with lithotripsy.
Removing stones and debris effectively is key. It helps restore normal bile flow and prevents serious complications like cholangitis or pancreatitis.
Risks and Complications of Endoscopic Procedures
While endoscopic procedures are generally safe, there are risks. These include pancreatitis, bleeding, infection, and gastrointestinal tract perforation. We take careful steps to reduce these risks, including choosing the right patients and using precise techniques.
It’s important for patients to know about these risks. Following post-procedure instructions carefully can help ensure a smooth recovery.
Percutaneous Biliary Drainage: Detailed Process
Percutaneous biliary drainage is a detailed process we’ll explain step-by-step. It’s key for those with blocked bile ducts, helping them feel better and move forward with treatment.
Pre-Procedure Preparation
Before starting, patients go through several steps. Imaging tests like ultrasound, CT scans, or MRI are used to check the blockage and plan the best way in.
- Laboratory tests check blood clotting and liver health.
- Patients learn about the procedure’s risks and benefits.
- They sign consent forms and ask any questions.
Step-by-Step Drainage Technique
The procedure has several important steps:
- The patient lies down, and the skin is cleaned.
- A needle is guided into the liver and bile duct under imaging.
- A guidewire is inserted, and the tract is widened for a catheter.
- The catheter is placed to drain bile externally or into the intestine.
Catheter Management and Maintenance
Managing the catheter right is key to avoiding problems and keeping it working long-term.
- The catheter site is kept clean and dressed.
- Patients learn to flush the catheter to avoid blockages.
- Regular check-ups are set to monitor the catheter and the patient’s health.
Potential Complications and Their Management
Though safe, complications like infection, bleeding, or catheter issues can happen.
Quick action to address these is vital. This might mean antibiotics for infection, stopping bleeding, or replacing the catheter.
Knowing how percutaneous biliary drainage works helps patients prepare better. It improves their chances of a good outcome and a better quality of life.
Surgical Interventions for Complex Bile Duct Blockages
Surgery is often needed for complex bile duct blockages when other treatments fail. We know surgery is usually a last resort. It’s used when less invasive methods can’t work or when complications arise.
Indications for Surgical Management
Surgery is needed for complex blockages that can’t be fixed by other means. Indications for surgery include tumors or strictures that can’t be stented, significant bile duct injuries, or when other treatments fail.
We look at each patient’s case carefully. We consider the blockage cause, the patient’s health, and any other conditions that might affect surgery.
Types of Surgical Procedures
Several surgical procedures can treat complex bile duct blockages. These include:
- Hepaticojejunostomy: This creates a new bile flow path by connecting the bile duct to the small intestine.
- Bile duct resection: Removing the affected bile duct is needed for tumors or strictures.
- Liver resection: Sometimes, part of the liver must be removed if the blockage harms liver function or if there are liver tumors.
Post-Surgical Recovery and Care
Post-surgical recovery is key. We focus on thorough care to help patients recover well. This includes watching for complications, managing pain, and supporting nutrition.
After surgery, patients are closely monitored. We check if the surgery worked and address any issues. We also help with lifestyle changes for better bile duct health.
Understanding bile duct blockages and surgery options helps us tailor care. This improves outcomes and quality of life for each patient.
Conclusion: Long-Term Management and Prevention
Managing bile duct blockages well needs a full plan. This includes quick action, right care, and long-term steps to stop it from happening again. We talked about different treatments like endoscopic methods, percutaneous biliary drainage, and surgery. Each one is chosen based on the blockage’s cause and how bad it is.
Keeping bile ducts open long-term means watching them closely and following up. This might mean regular tests and visits to the doctor. It helps catch problems early and keeps the bile duct flowing well.
Stopping bile duct blockages before they start is key. This means dealing with causes like gallstones, tumors, or inflammation. Knowing what causes problems helps people take steps to avoid them. This includes eating well, managing health issues, and avoiding medicines that can harm the bile duct.
Combining good treatment with long-term care and prevention helps a lot. It makes life better for people with bile duct blockages. Knowing how to keep bile ducts open and manage them is vital for staying healthy.
FAQ
What are the common causes of a blocked bile duct?
Gallstones and biliary sludge are common causes. Tumors, strictures, and inflammatory conditions also play a role. Trauma or medical procedures can cause blockages, too.
What symptoms indicate a blocked bile duct?
Early signs include mild jaundice. Severe symptoms are intense pain, dark urine, and pale stools. It’s important to notice these signs to get medical help quickly.
How is a blocked bile duct diagnosed?
Tests like MRI and CT scans are used. Lab tests and tissue analysis help find the cause. These tools accurately diagnose blockages.
What is the purpose of draining a blocked bile duct?
Draining it helps restore bile flow. It relieves symptoms and prevents serious problems. This improves patient health.
What are the different types of drainage procedures for bile duct blockages?
Procedures include ERCP with stent placement and percutaneous biliary drainage. Surgery is also an option. The right procedure depends on the blockage and the patient’s health.
How is percutaneous biliary drainage performed?
A catheter is inserted through the skin into the bile duct. This drains the blocked bile. Proper care is needed before and after the procedure to avoid complications.
What are the risks associated with endoscopic procedures for bile duct drainage?
Risks include pancreatitis, bleeding, and infection. Stent problems can also occur. Knowing these risks helps manage patient care and expectations.
How can bile duct blockages be prevented?
Manage gallstones and eat well. Avoid too much alcohol and get regular check-ups. Early intervention and care can prevent problems.
What is the role of stent placement in bile duct drainage?
Stents keep the bile duct open. They are placed during ERCP. This is key for bile flow.
What is liver drainage, and how does it relate to bile duct blockages?
Liver drainage is when bile is drained from the liver due to blockages. Various procedures, like percutaneous biliary drainage, can achieve this.
How do you manage a drain in the liver?
Care for a liver drain includes maintaining the catheter and watching for infection or blockage. Regular follow-ups with a healthcare provider are vital.
References
- Shojaiefard, A., et al. (2009). Various techniques for the surgical treatment of common bile duct stones. World Journal of Surgery, 33(8), 1660-1669. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2722154/


































