Last Updated on November 26, 2025 by Bilal Hasdemir

Epidurals are safe for most people, and typical back soreness at the insertion site fades within days to weeks; there is no consistent evidence that epidurals cause chronic back pain, and long-term issues are uncommon and usually relate to pregnancy, delivery mechanics, or rare complications rather than the epidural itself. Serious causes of lasting back problems—like epidural abscess or hematoma—are very rare, but severe back pain with fever, new leg weakness, numbness, or bladder/bowel changes needs urgent assessment to prevent long-term harm; for the vast majority, the “long term effects of epidural” on the back are minimal when modern safety practices are followed.
Key Takeaways
- Epidurals are generally safe, but some patients report back pain.
- Research indicates that persistent back pain directly caused by epidurals is rare.
- Temporary back pain after an epidural is more common.
- Understanding the risks can help you make informed decisions.
- Liv Hospital provides complete care and advice for patients.
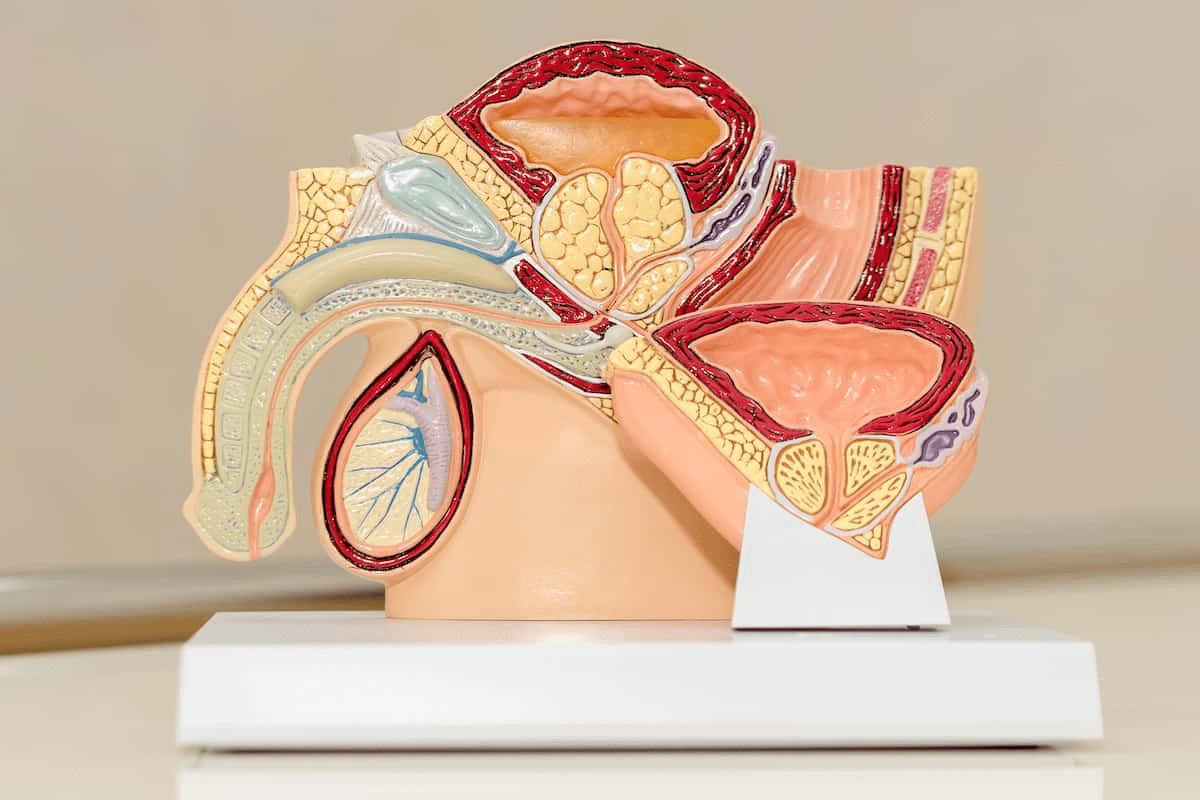
Understanding Epidural Anesthesia

Epidural anesthesia is a method of pain relief. It involves injecting medication around the spinal cord. This is why it’s often used during childbirth to manage pain.
What Is an Epidural and How Does It Work?
An epidural is given in the epidural space, a fatty area around the spinal cord. This space has nerves that carry pain signals. By injecting medication here, epidural anesthesia blocks these signals.
To give an epidural, a needle and catheter are inserted. The catheter lets medication flow continuously. This keeps pain away during labor.
Common Uses for Epidural Anesthesia
Epidural anesthesia is well-known for pain relief during childbirth. But it’s also used for other purposes:
- Pain relief during labor and delivery
- Post-operative pain management for surgeries involving the lower abdomen and legs
- Relief for chronic pain conditions in some cases
A study in the Journal of Pain Research shows epidural anesthesia is effective for labor pain. It’s a popular choice for many mothers.
“Epidural analgesia is considered one of the most effective methods of pain relief during labor.” – Journal of Pain Research
The Epidural Administration Process
Administering epidural anesthesia needs skill and care. Here’s what happens:
- Preparation: Checking vital signs and getting the mother ready.
- Insertion: Putting in the epidural needle and catheter.
- Administration: Giving the medication through the catheter.
- Monitoring: Watching the mother’s and baby’s health and adjusting the medication as needed.
| Step | Description |
| Preparation | Monitoring vital signs and positioning |
| Insertion | Inserting epidural needle and catheter |
| Administration | Delivering medication through the catheter |
| Monitoring | Adjusting medication based on vital signs |
Knowing how epidural anesthesia is given helps understand its effects. While it’s generally safe, there are risks and side effects. We’ll look at these in the next sections.
Common Short-Term Side Effects of Epidurals

Epidurals are usually safe, but it’s good to know about common side effects. Knowing these can help you feel better about your epidural experience.
Immediate Reactions at the Injection Site
Right after an epidural, you might feel some soreness, redness, or swelling at the site. These reactions are usually mild and go away in a few days.
Temporary Back Soreness and Discomfort
Many people feel sore or uncomfortable in their back after an epidural. This is often because of the needle or catheter insertion. But don’t worry, this soreness is usually short-lived and can be eased with over-the-counter pain meds.
Other Expected Short-Term Effects
You might also experience headaches, numbness, or weakness in your legs. These effects are usually temporary and go away as the epidural fades. It’s important to talk to your doctor about any worries you have.
Here are some common short-term side effects to watch out for:
- Mild soreness at the injection site
- Temporary back pain
- Headaches
- Numbness or weakness in the legs
Knowing about these side effects can help you get ready for your epidural. It also helps you understand what to expect during recovery.
The Long-Term Effects of Epidural Anesthesia
Epidurals help with pain during labor, but what about their long-term effects on back health? We’ll look into the lasting impacts of epidural anesthesia. We’ll also talk about what “long-term” means in medicine and the documented effects.
Defining “Long-Term” in Medical Context
In medical studies, “long-term” means effects seen over a long time, usually six months or more. For epidural anesthesia, long-term effects are symptoms or changes lasting months or years after the procedure.
Knowing this time frame is key to understanding if epidural anesthesia leads to chronic back pain. We’ll look at the data to answer this question.
Documented Persistent Effects
Research shows that while back pain after an epidural is common, chronic pain is rare. Pregnancy and childbirth changes might play a bigger role in lasting pain than the epidural itself.
Key findings include:
- Most women have back pain during pregnancy, which can last after giving birth.
- The strain of labor and delivery can cause ongoing back pain.
- Back problems before pregnancy can get worse during and after childbirth.
Differentiating Between Association and Causation
It’s important to tell the difference between association and causation when looking at epidural anesthesia’s long-term effects. Just because two things happen together doesn’t mean one causes the other.
If a woman has back pain a year after an epidural, it’s hard to say the epidural caused it without looking at other factors. We need to carefully examine the evidence to understand the link between epidural anesthesia and long-term back pain.
By exploring this complex issue, we can better understand the long-term effects of epidural anesthesia. This helps patients and healthcare providers make better choices.
Research Findings: Studies on Epidurals and Chronic Back Pain
Studies have looked into how epidural anesthesia affects back pain over time. They aim to see if epidurals can lead to chronic back pain years later.
Studies Suggesting a Connection
Some studies hint at a link between epidural anesthesia and chronic back pain. For example, a study might show that women who got epidural pain relief during labor are more likely to have back pain later. Nerve irritation or damage during the epidural procedure could be the reason.
Other research found that the method used for the epidural and the provider’s experience can affect the risk of long-term back pain. This means the connection is not the same for everyone and can depend on several factors.
Studies Finding No Significant Relationship
But, many studies have found no big difference in long-term back pain between those who got epidural anesthesia and those who didn’t. A study in the PMC journal is a good example. It found that epidural pain relief during labor doesn’t increase the risk of long-term back pain.
These results are reassuring. They show that epidural anesthesia is usually safe for most people’s back health in the long run. Yet, it’s important to remember that individual factors can play a role.
Limitations of Existing Research
Even though the research is helpful, there are some limits. Many studies rely on what people say, which can be biased. Also, the different ways epidurals are done and the varied patient groups make it hard to draw clear conclusions.
To really understand the link between epidurals and chronic back pain, we need more research. This should include bigger, more varied study groups and longer follow-ups.
| Study | Findings | Limitations |
| Randomized PMC Journal Study | No significant difference in long-term back pain | Reliance on self-reported data |
| Review of Multiple Studies | Potential link between epidural and chronic back pain | Variability in study methodologies |
Rare Complications That May Lead to Long-Term Back Pain
Epidural anesthesia is usually safe, but rare complications can cause long-term back pain. These issues, though uncommon, can greatly affect a person’s life. It’s important for patients to know about these risks and for doctors to take steps to avoid them.
Nerve Damage and Injury
Nerve damage is a rare but serious side effect of epidural anesthesia. It can happen if the needle hits a nerve or if the solution irritates the area. Nerve damage can lead to chronic pain, numbness, or tingling that lasts long after the procedure.
To lower the risk of nerve damage, doctors use the right technique and imaging. Experienced healthcare providers are more skilled at reducing complications.
Infection and Epidural Abscess
Infection is a rare but serious issue that can happen with epidural anesthesia. An epidural abscess forms if bacteria get in during the procedure. This needs quick medical attention to avoid more problems, like long-term back pain and nerve damage.
Following strict sterile procedures and proper care after the procedure can help prevent infection. Patients should watch for signs of infection, like fever, redness, or swelling at the injection site.
Hematoma Formation
Hematoma, or blood outside blood vessels, is a rare but serious side effect. A big hematoma can press on nerves and cause long-term pain or nerve problems. People taking blood thinners or with bleeding disorders are at higher risk.
Choosing the right patients and managing blood thinners before the procedure can lower this risk. Quick action to treat a hematoma is key to avoiding long-term issues.
| Complication | Description | Risk Factors |
| Nerve Damage | Damage to nerves during the procedure | Improper technique, lack of imaging guidance |
| Infection | Introduction of bacteria during the procedure | Poor sterile technique, inadequate post-procedure care |
| Hematoma | Accumulation of blood outside blood vessels | Anticoagulant therapy, bleeding disorders |
Distinguishing Between Epidural-Related Pain and Other Causes
It’s key to tell epidural pain from other back pain causes for good treatment. When looking at long-term back pain after an epidural, we must think about several things. This helps find the real cause of the pain.
Pregnancy-Related Musculoskeletal Changes
Pregnancy changes the body a lot to fit the growing baby. This can put strain on the back muscles and joints. Pregnancy-related musculoskeletal changes can make the back hurt because of relaxed ligaments and joints.
Labor and Delivery Strain
Labor and delivery can also hurt the back. The physical effort and possible problems during delivery can cause lasting back pain. It’s important to see how labor and delivery strain affects back pain.
Pre-existing Back Conditions
Back problems before pregnancy can get worse with it and the epidural. Looking at a patient’s health history is key when checking back pain. Pre-existing back conditions like scoliosis or past injuries can play a part.
Postpartum Recovery Factors
The time after giving birth brings many physical changes that can hurt the back. Postpartum weight gain, posture changes, and muscle weakness can cause back pain. Knowing these can help figure out if the pain is from the epidural or other reasons.
Healthcare providers and patients can understand long-term back pain better by looking at these factors. This way, they can find better ways to manage and treat the pain.
Patient Experiences: Reported Cases of Back Pain After Epidurals
Some patients have reported persistent back pain after epidural anesthesia. This has sparked debate about its causes. We will look at common concerns and how doctors evaluate these claims.
Common Concerns
Patients often worry about the long-term effects of epidural anesthesia. They complain of persistent lower back pain, stiffness, and sharp pains. These symptoms can be very distressing, lasting long after recovery.
Many patients question if their pain is from the epidural or other factors. Knowing the cause is key to finding the right treatment. Doctors must carefully examine each case to find the root of the pain.
Patterns in Patient Reports
Research has found common patterns in patient reports. Many patients experience back pain within weeks after childbirth, with some pain lasting months or years. The pain’s severity and duration vary greatly.
Studies suggest certain factors may lead to long-term back pain after epidural anesthesia. These include a history of back problems, the complexity of the delivery, and individual pain perception.
Medical Evaluation of Patient Claims
When patients report back pain after epidural anesthesia, doctors conduct thorough evaluations. This includes a detailed medical history, physical examination, and sometimes more tests. The goal is to find any underlying conditions causing the pain.
In some cases, the pain may not be from the epidural. It could be due to pre-existing back conditions, pregnancy-related changes, or strain during labor and delivery. Accurate diagnosis is vital for effective treatment.
Understanding patient experiences and the factors behind back pain after epidural anesthesia helps healthcare providers. They can better support their patients and work to prevent long-term discomfort.
Risk Factors That May Increase Chances of Post-Epidural Back Issues
Back pain after an epidural can be influenced by several factors. Knowing these can help both patients and doctors make better choices. This can help avoid or lessen complications.
Pre-existing Medical Conditions
Medical conditions before an epidural can raise the risk of back pain afterward. Conditions like chronic back pain, arthritis, and previous spinal injuries can make patients more likely to experience back issues. It’s important for patients to share their full medical history with their doctor before the procedure.
| Pre-existing Condition | Risk Level | Precautions |
| Chronic Back Pain | High | Careful patient selection and monitoring |
| Arthritis | Moderate | Adjusting epidural technique and medication |
| Previous Spinal Injuries | High | Imaging studies before epidural placement |
Technique and Provider Experience
The way an epidural is given and the doctor’s experience can also affect the risk of back pain. Experienced providers are more likely to use the best methods, lowering the risk of problems. Using ultrasound-guided epidural placement can make the procedure safer and more accurate.
Multiple Epidural Attempts
Trying to place an epidural more than once can increase the risk of pain and other issues. Each try can cause minor damage, leading to inflammation and discomfort. Trying to limit attempts and using precise methods can help reduce this risk.
Post-Procedure Activity and Recovery
How a patient acts and recovers after an epidural can also affect the risk of back pain. Adequate rest and proper posture are key during recovery. Patients should follow their doctor’s advice on activity levels and recovery practices to lower the risk of back problems.
By understanding and addressing these risk factors, patients and doctors can work together to lower the chance of back pain after an epidural. This teamwork ensures the best results for those undergoing epidural procedures.
Preventative Measures and Alternative Pain Management Options
To lower the chance of back pain after an epidural, it’s key to take steps and look at other pain relief ways. Knowing how epidurals are given, how to care for yourself after, and other pain relief methods helps patients make smart choices.
Best Practices for Epidural Administration
The skill of the doctor giving the epidural greatly affects the risk of back pain. Research shows that the right technique, like placing the needle and catheter correctly, can lessen problems. It’s wise for patients to pick experienced doctors and talk about any worries they have.
Key considerations for epidural administration include:
- Choosing an experienced healthcare provider
- Discussing pre-existing medical conditions
- Understanding the epidural administration process
Post-Epidural Care Recommendations
Right after care is vital to avoid back pain. Patients should stick to certain rules to heal well. This means keeping a good posture, doing light exercises, and not lifting heavy or bending.
| Post-Epidural Care Tips | Benefits |
| Maintain good posture | Reduces strain on the back |
| Gentle exercises | Promotes healing and flexibility |
| Avoid heavy lifting or bending | Prevents strain on the epidural site |
Non-Epidural Pain Management Alternatives
For those looking for other options instead of epidural anesthesia, there are choices. These include physical therapy, using hot and cold packs, and taking certain medicines. Each has its own good points and should be thought about based on what each person needs.
By looking into these steps and other pain relief methods, patients can handle their pain better. This can also help cut down the risk of long-term back pain linked to epidurals.
Conclusion: The Current Medical Consensus on Epidurals and Long-Term Back Pain
We’ve looked into how epidurals affect long-term back pain. The research shows epidural anesthesia is safe and works well for pain relief. But, long-term back pain is a rare side effect.
Some studies found that back pain after an epidural might be due to other reasons. This includes pre-existing back issues or changes in the body during pregnancy. The chance of long-term back pain from epidurals is small. Most people don’t have ongoing back problems.
It’s key to know the good and bad of epidural anesthesia. Talking to a healthcare provider about your concerns helps you make a smart choice. Proper use of epidurals and care after the procedure can lower the risk of long-term back pain.
In summary, epidurals are mostly safe. Knowing the possible long-term effects and taking steps to avoid them can lead to a better experience. Long-term back pain from epidurals is rare. Whether epidurals can cause back pain depends on many personal factors.
FAQ
Can epidurals cause back pain years after the procedure?
Some studies link epidurals to long-term back pain. But, how likely and severe it is varies. We dive into the research to understand this better.
What are the common short-term side effects of epidurals?
Right after, you might feel pain or soreness at the injection site. You might also feel discomfort in your back. These symptoms are usually mild and go away quickly.
How can I differentiate between epidural-related pain and other causes of back pain?
It’s hard to tell if back pain comes from an epidural or other reasons. Pregnancy, labor, and pre-existing conditions can all play a part. Understanding these factors helps.
What are the risk factors that may increase the chances of post-epidural back issues?
Several things can raise your risk. These include your health before the epidural, the doctor’s skill, and how active you are after the procedure. These factors can affect your back health.
Are there any preventative measures or alternative pain management options available?
Yes, there are ways to lower your risk of back pain. Following best practices and exploring other pain relief options can help.
Can pre-existing back conditions affect the likelihood of experiencing back pain after an epidural?
Yes, having a pre-existing back condition can increase your risk. It’s important to talk to your doctor about your health history.
How do medical professionals evaluate patient claims of back pain after epidurals?
Doctors look at your medical history, the epidural details, and the pain’s characteristics. They might also do tests to find the cause of the pain.
Can epidurals cause chronic back pain?
Some studies suggest a link between epidurals and chronic pain. But, other studies disagree. More research is needed to understand this connection.
What are the rare complications that may lead to long-term back pain?
Rare but serious issues like nerve damage, infection, or hematoma can cause long-term pain. These complications are rare but serious if not managed right.
How can I minimize the risk of back pain after an epidural?
Follow best practices and post-epidural care. Being aware of risk factors can also help lower your chance of back pain.
References
- Friedly, J. L., Comstock, B. A., Heagerty, P. J., Bauer, Z., Rothman, M. S., Suri, P., & Jarvik, J. G. (2020). Long-term effects of repeated injections of local anesthetic with or without corticosteroid for lumbar spinal stenosis. The Spine Journal, 20(2), 203-213. https://pubmed.ncbi.nlm.nih.gov/31521751/