
At Liv Hospital, we are dedicated to top-notch healthcare for all. Advances in brain neoplasm treatment have greatly improved care for brain cancer patients. This brings new hope to those facing this disease.
Recent guidelines highlight the value of maximal safe tumor resection, new radiation methods, and genetic testing in brain tumor management. Our team creates personalized treatment plans for each patient. We use the latest therapies like radiation and chemotherapy.
We know every patient’s story is different. We aim to offer caring support that meets their unique needs. By using the newest in oncology, we aim to enhance life quality for brain cancer patients.
Key Takeaways
- Personalized treatment plans for brain cancer patients
- Advanced radiation modalities for effective tumor management
- Molecular profiling to inform treatment decisions
- Maximal safe tumor resection to improve patient outcomes
- Comprehensive support for international patients
Current Landscape of Brain Cancer Diagnosis and Care
Our understanding of brain tumors is growing. This change is leading to more personalized treatments. Brain cancer diagnosis and care now use the latest medical science to offer better treatment options.
Understanding Brain Tumor Types and Classifications
Brain tumors are divided into primary and metastatic types. Primary tumors start in the brain, while metastatic tumors spread from other parts. Each type has its own characteristics and treatment needs. Accurate classification is key to choosing the right treatment.
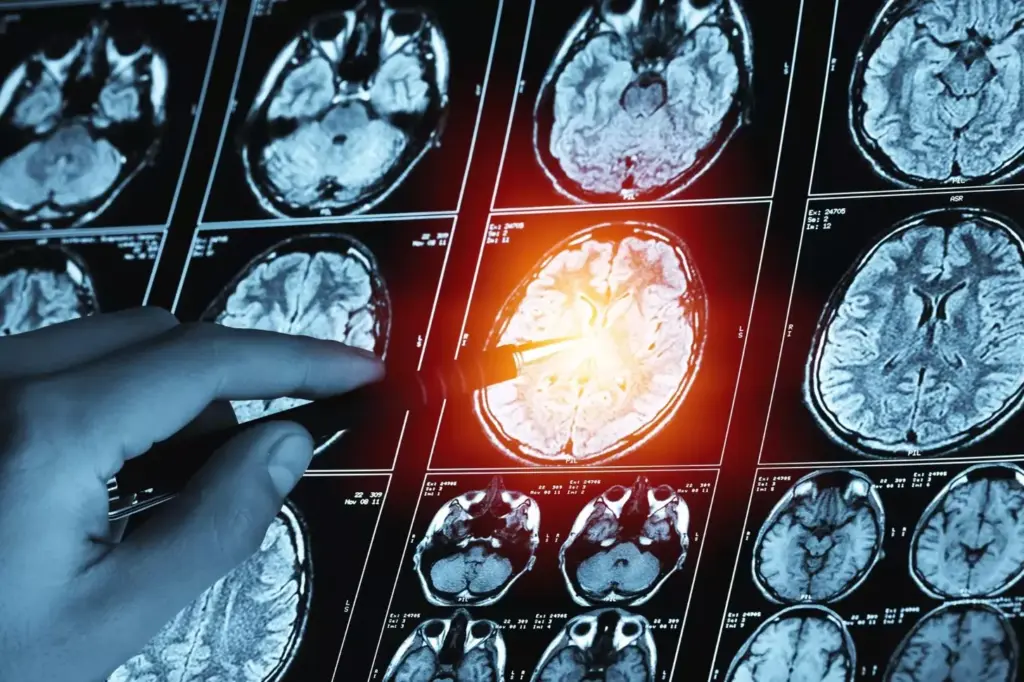
We use MRI and CT scans, along with histopathological examination, to classify tumors. This detailed approach helps us tailor treatments to each patient’s needs.
The Importance of Molecular Profiling in Treatment Planning
Molecular profiling is now a vital part of brain cancer treatment planning. It helps us understand a tumor’s genetic and molecular makeup. This way, we can find the best targets for therapy and predict how well a patient will respond. This info is essential for making treatment decisions.
Research shows molecular profiling is key in choosing treatments for brain cancer patients. We use this data to create personalized treatment plans. Our team works with patients to understand their needs and develop a plan that fits their situation.
Surgical Resection: The Foundation of Brain Neoplasm Treatment

Brain neoplasm treatment often starts with surgical resection. This procedure needs precision and advanced technology for the best results. At our institution, we’ve made big strides in surgical techniques. This allows us to give our patients the highest level of care.
Maximal Safe Tumor Resection Techniques
Maximal safe tumor resection is key in surgery. It aims to remove as much tumor as possible while keeping brain tissue safe. We use many techniques, like intraoperative MRI and functional mapping, to achieve this.
Intraoperative MRI lets us see how much tumor we’ve removed in real-time. This helps us make changes during surgery. Functional mapping helps us find important brain areas. This way, we can keep essential functions safe.
Advanced Surgical Navigation Technologies
Advanced navigation technologies are vital for precise tumor removal. We use systems with 3D imaging and real-time tracking to guide our surgeons. These technologies help us:
- Find tumors and important structures accurately
- Plan the best surgical approach
- Check progress and make changes as needed
Awake Craniotomy for Functional Preservation
Awake craniotomy is a valuable technique for some patients. It lets us operate while the patient is awake and can respond. This is helpful for tumors near important brain areas.
During an awake craniotomy, we can:
- Watch the patient’s brain function in real-time
- Adjust our technique to avoid brain damage
- Keep the patient comfortable and able to handle the procedure
Here’s a summary of the benefits of these advanced surgical techniques in a tabular form:
| Technique | Benefits | Clinical Application |
|---|---|---|
| Intraoperative MRI | Real-time assessment of tumor removal | Maximizing tumor resection while preserving brain tissue |
| Functional Mapping | Identification of critical brain areas | Preserving neurological function |
| Awake Craniotomy | Real-time neurological monitoring | Tumors near critical brain areas |
Conventional Radiation Therapy Approaches
Our team uses conventional radiation therapy to treat brain tumors. We use the latest techniques for the best results. Radiation therapy is key in treating brain cancer, with different methods for each patient.
Whole-Brain Radiation Therapy (WBRT)
Whole-Brain Radiation Therapy (WBRT) treats brain tumors that have spread. WBRT gives a uniform dose of radiation to the whole brain. It helps control tumor growth and eases symptoms.
The benefits of WBRT include:
- Effective in treating multiple brain metastases
- Can help reduce symptoms such as headaches and seizures
- May be used in combination with other treatments like surgery or chemotherapy
Fractionated External Beam Radiation
Fractionated External Beam Radiation treats brain tumors. It delivers highly targeted radiation beams to the tumor. This method protects the healthy brain tissue around it.
The advantages of Fractionated External Beam Radiation include:
- Precise targeting of tumors, reducing damage to surrounding brain tissue
- Can be fractionated into multiple sessions, allowing for better tolerance
- Effective for treating a wide range of brain tumor types and sizes
Managing Radiation-Related Side Effects
Radiation therapy is effective but can cause side effects. Our team works hard to reduce these effects. We aim to improve our patients’ quality of life.
Common side effects include:
- Fatigue
- Hair loss
- Nausea and vomiting
We use various strategies to manage these side effects. This includes:
- Medications to alleviate symptoms
- Dietary counseling to maintain nutrition
- Supportive care to address emotional and psychological needs
By understanding and managing side effects, we enhance the benefits of radiation therapy for our patients.
Stereotactic Radiosurgery for Precise Tumor Targeting
Stereotactic radiosurgery is a non-invasive method that targets brain tumors with great accuracy. It delivers high doses of radiation to specific areas. This minimizes damage to healthy tissue nearby.
Gamma Knife and CyberKnife Technologies
We use advanced technologies like Gamma Knife and CyberKnife for this procedure. Gamma Knife radiosurgery is great for treating certain brain tumors and vascular malformations. It uses cobalt sources for precise radiation.
CyberKnife technology is flexible, treating tumors in various brain and body locations. It uses a robotic arm to deliver radiation from different angles.
Both technologies are highly effective in treating brain tumors. They offer a non-invasive option compared to traditional surgery.
Linear Accelerator (LINAC) Based Treatments
LINAC-based stereotactic radiosurgery is another technique we use. It employs a linear accelerator to create high-energy X-rays. These X-rays are tailored to the tumor’s shape and size. LINAC-based treatments are versatile, suitable for many tumor types and sizes.
Ideal Candidates for Stereotactic Approaches
Not every patient is a good fit for stereotactic radiosurgery. We assess each case carefully. Factors like tumor size, location, and patient health are considered.
Patients with small to medium-sized tumors that are well-defined are often good candidates. By choosing the right technology for each patient, we improve outcomes.
Systemic Chemotherapy Protocols
Systemic chemotherapy is key in treating brain tumors. It offers different plans for each patient. Our goal is to make treatments work well and have fewer side effects.
Temozolomide and Other First-Line Agents
Temozolomide is a top choice for treating brain tumors, like glioblastoma. It can get past the blood-brain barrier, making it effective. We use it with surgery and radiation to treat patients.
“Temozolomide has changed how we treat glioblastoma, giving patients a better chance,” studies say. Our team keeps up with new research to offer the best treatments.
Blood-Brain Barrier Considerations
The blood-brain barrier is a big challenge in treating brain tumors. We pick chemotherapy that can get past this barrier. This is key to making a good treatment plan.
Combination Chemotherapy Strategies
Combination chemotherapy uses several drugs to fight brain cancer. This method can beat resistance to single drugs and may help patients more. We create these plans based on the latest research and each patient’s needs.
A leading oncologist says, “Combination chemotherapy is a hopeful strategy against brain cancer.” Our team works hard to keep up with research to give our patients the best care.
Targeted Molecular Therapies Based on Tumor Genetics
Targeted molecular therapies are a big step forward in treating brain cancer. They focus on the unique genetic traits of each tumor. This approach aims to improve treatment results and lessen side effects.
EGFR, BRAF, and Other Molecular Targets
The genetics of brain tumors are complex, with many mutations that can cause growth. EGFR (Epidermal Growth Factor Receptor) and BRAF are key targets in brain cancer. These genes, when mutated, can lead to unchecked cell growth and tumor spread.
Other targets include IDH1 and IDH2 mutations, important in some gliomas. Finding these targets has led to new drugs that can block the mutated proteins. This could stop tumor growth.
Tyrosine Kinase Inhibitors in Brain Cancer
Tyrosine kinase inhibitors (TKIs) are a promising drug class for brain cancer. They target specific tyrosine kinases, enzymes that control cell division and survival. By blocking these enzymes, TKIs can slow or stop cancer cell growth.
In brain cancer, TKIs work well for patients with certain genetic changes. For example, TKIs targeting EGFR are used when this receptor is overactive or mutated. Researchers are working to find the best TKI combinations and ways to beat resistance.
Overcoming Resistance to Targeted Therapies
While targeted therapies are promising, overcoming resistance is a big challenge. Tumors can adapt to the therapy, making it less effective over time. Researchers are exploring combination treatments with chemotherapy or radiation therapy.
Another approach is to develop new targeted therapies that can bypass resistance. For instance, newer TKIs aim to target specific resistance mutations. This could keep targeted therapies effective for longer.
Immunotherapy Approaches for Brain Cancer
Immunotherapy is a new hope in treating brain cancer. It uses the body’s immune system to fight cancer. This is a big change in how we manage brain tumors.
We’re leading the way in using checkpoint inhibitors, vaccine-based immunotherapies, and cellular therapies like CAR T-cells. These methods help boost the body’s defense against cancer.
Checkpoint Inhibitors: PD-1 and CTLA-4 Targeting
Checkpoint inhibitors have changed cancer treatment. They help the immune system fight cancer better. In brain cancer, they target PD-1 and CTLA-4 to improve treatment.
Studies are checking if these inhibitors work well in brain cancer. So far, the signs are good. They might become a key part of treatment.
Vaccine-Based Immunotherapies
Vaccine-based treatments are also promising. They help the immune system find and destroy cancer cells. By focusing on specific brain tumor markers, they aim for a strong immune response.
Researchers are working to make these vaccines better. They want to get past the blood-brain barrier. Early trials are showing hope, leading to more research.
Cellular Therapies Including CAR T-Cells
CAR T-cell therapy is a new way to fight cancer. It changes T-cells to attack cancer cells. This method has worked well in some cancers and is being tested in brain cancer too.
We’re studying CAR T-cell therapy in brain cancer patients. It’s a tough challenge to get these cells to the brain tumor. But, early results are promising. They suggest it could be a good option for some patients.
Local Drug Delivery Systems and Implants
Local drug delivery systems are a big step forward in treating brain cancer. They offer targeted therapy with fewer side effects. We aim to use these new methods to give our patients the best care possible.
These systems send drugs straight to the tumor, avoiding healthy tissues. This cuts down on the bad effects of traditional treatments.
Carmustine Wafers (Gliadel)
Carmustine wafers, or Gliadel, are a key local drug delivery system for brain cancer. They are made of a material that breaks down and release carmustine, a chemotherapy drug. They are placed in the tumor during surgery.
a leading neurosurgeon, noted, “Carmustine wafers have changed how we treat glioblastoma. They give a steady dose of chemotherapy right where it’s needed.”
Convection-Enhanced Delivery Methods
Convection-enhanced delivery (CED) is a new way to put drugs directly into brain tumors. It uses catheters implanted during surgery. This method spreads the drug evenly in the tumor.
CED is being tested in clinical trials for different brain tumors. It’s a flexible way to deliver many types of drugs, including chemotherapy and immunotherapies.
Emerging Local Treatment Technologies
New technologies in local drug delivery systems are coming fast. We’re seeing new implants, hydrogel systems, and nanoparticle therapies. These could be big improvements.
“The future of brain cancer treatment is all about innovation,” said
.
As research keeps moving forward, we expect these new technologies to make local drug delivery systems even better. They could bring new hope to those with brain tumors.
Tumor Treating Fields (TTFields) Therapy
Tumor Treating Fields (TTFields) therapy is a new way to fight brain cancer. It uses electric fields to stop cancer cells from growing. This gives hope to those with brain tumors.
Mechanism of Action and Application
TTFields therapy sends electric fields to tumors to slow down cancer cell growth. It’s often used with other treatments like chemo or radiation. The device is easy to carry, so patients can keep up with their daily life.
The mechanism involves:
- Disrupting mitotic spindle formation
- Interfering with cell division
- Inducing apoptosis in cancer cells
Experts say TTFields therapy is helping patients with glioblastoma, a tough brain cancer type.
“The use of TTFields therapy represents a significant advancement in our fight against brain cancer, providing patients with an additional treatment option that is both effective and tolerable.”
Clinical Evidence for Effectiveness
Studies show TTFields therapy works well against brain cancer. It’s been shown to increase survival and time without cancer growth in glioblastoma patients.
The evidence for TTFields therapy is strong. It shows:
- Improved survival rates
- Enhanced quality of life
- Minimal additional toxicity
Patient Experience and Compliance Considerations
It’s important for patients to stick with TTFields therapy. They need to wear the device for at least 18 hours a day. Our team helps patients understand and manage the treatment.
Key considerations for patient compliance include:
- Understanding the importance of continuous treatment
- Managing device-related skin irritation
- Integrating TTFields therapy into daily routines
We offer full support and education to help patients get the most from TTFields therapy. This improves their treatment experience.
Advanced Clinical Trials and Experimental Brain Cancer Therapies
We are leading the way in brain cancer clinical trials, bringing the newest treatments to our patients. Our goal is to give our patients the best care by using the latest treatments.
Advanced clinical trials are key in fighting brain cancer. They offer new hope and help us learn more about effective treatments. These trials test new therapies that could improve patient outcomes.
Gene Therapy Approaches
Gene therapy is a promising area in brain cancer treatment. It targets the genetic causes of tumors, aiming to kill cancer cells or slow their growth. We’re involved in trials that explore different gene therapy methods, including those that boost the immune system against cancer.
The table below shows some gene therapy strategies being tested in trials:
| Gene Therapy Strategy | Description | Potential Benefits |
|---|---|---|
| Suicide Gene Therapy | Introduces a gene that makes cancer cells susceptible to a specific drug | Selective killing of cancer cells |
| Immunogene Therapy | Genetically modifies cells to enhance immune response against cancer | Boosts body’s natural defenses |
| Oncogene Inhibition | Targets and inhibits genes driving cancer growth | Slows or stops tumor progression |
Oncolytic Virus Treatments
Oncolytic virus therapy is another innovative method being tested. It uses viruses that target and kill cancer cells, leaving healthy cells alone. Our institution is part of trials that look at the safety and effectiveness of these viruses in treating brain cancer.
These viruses can carry genes to cancer cells, making them even more effective. The promise of oncolytic virus therapy to treat cancer with fewer side effects is very exciting.
How to Access Cutting-Edge Treatment Options
Getting into clinical trials for cutting-edge treatments needs a team effort. Our team helps patients find trials that fit their needs. We support them from the start to joining the trial.
For more information on our clinical trials and experimental therapies, talk to your doctor or reach out to our clinical trials team.
Multidisciplinary Approach to Brain Neoplasm Treatment
Brain neoplasms are complex and need a team effort for treatment. This team ensures patients get care that fits their needs.
Coordinating Care Across Specialties
Working together is key in treating brain cancer. Our team includes neurosurgeons, radiation oncologists, and more. They create a treatment plan just for each patient.
Key elements of coordinated care include:
- Regular team meetings to talk about patient cases
- Decisions made together by specialists
- Open talks with patients and their families
a top neuro-oncologist, says,
“A team-based approach allows us to leverage the expertise of various specialists, ultimately improving patient outcomes.”
Supportive and Palliative Care Integration
Adding supportive and palliative care to treatment plans is vital. It helps manage symptoms, relieve pain, and support the mind and spirit.
| Aspect of Care | Description | Benefits |
|---|---|---|
| Symptom Management | Controlling symptoms like nausea, fatigue, and seizures | Improved quality of life |
| Pain Relief | Strategies to manage pain effectively | Less discomfort, better function |
| Psychological Support | Counseling and emotional support for patients and families | Better coping, less stress |
Quality of Life Considerations in Treatment Planning
We focus on quality of life when planning treatments. We make sure treatments match the patient’s well-being and goals.
Our multidisciplinary approach to treating brain neoplasms improves outcomes and quality of life. We’re dedicated to providing top-notch, patient-focused care.
Conclusion: The Future of Brain Cancer Care
We are dedicated to giving our patients with brain cancer the best care possible. New treatments and technologies will keep improving how well patients do. Studies show great results in median overall survival rates and how long patients stay without their cancer getting worse.
We take a whole-person approach to treating brain tumors. This means we care for our patients’ physical, emotional, and social health. We think the best way to fight brain cancer is by using all the latest treatments together.
We aim to lead in brain cancer care and make it better for our patients. Our promise to offer top-notch healthcare to everyone, including international patients, never changes.
FAQ
What are the most common treatment options for brain neoplasms?
We offer many treatments, like surgery, radiation, and chemotherapy. We also use targeted therapies and immunotherapy. Each treatment is chosen based on the patient’s needs.
How is molecular profiling used in brain cancer treatment planning?
Molecular profiling helps us plan treatments. It lets us find specific genetic mutations. This way, we can tailor treatments to each patient’s tumor.
What is the role of surgical resection in brain neoplasm treatment?
Surgery is key in treating brain tumors. Our neurosurgeons use advanced tools and techniques. They aim to remove tumors safely and effectively.
What types of radiation therapy are available for brain tumor treatment?
We use different radiation therapies. These include whole-brain radiation and stereotactic radiosurgery. We use tools like Gamma Knife and CyberKnife for precision.
How is chemotherapy used in brain cancer treatment?
Our team uses chemotherapy to fight brain cancer. We consider the blood-brain barrier when choosing agents. Often, we use a combination of drugs.
What are targeted molecular therapies, and how are they used in brain cancer treatment?
Targeted therapies aim at specific genetic mutations. We keep up with new tyrosine kinase inhibitors. We also work to overcome resistance to these treatments.
What is Tumor Treating Fields (TTFields) therapy, and how is it used in brain cancer treatment?
TTFields therapy uses electric fields to stop cancer cells from dividing. We carefully review the evidence. We consider patient factors to ensure the best results.
How can patients access cutting-edge treatment options, such as gene therapy and oncolytic virus treatments?
We help patients get access to new clinical trials and treatments. We guide them through the process. This way, they can try innovative therapies.
What is the importance of supportive and palliative care in brain neoplasm treatment?
We focus on supportive and palliative care. We aim to improve quality of life. Our team works with other specialties for complete care.
How is brain cancer treatment coordinated across different specialties?
Our team takes a multidisciplinary approach. We work with various specialties for a complete treatment plan. This ensures the best outcomes for patients.
FAQ
What are the most common treatment options for brain neoplasms?
We offer many treatments, like surgery, radiation, and chemotherapy. We also use targeted therapies and immunotherapy. Each treatment is chosen based on the patient’s needs.
How is molecular profiling used in brain cancer treatment planning?
Molecular profiling helps us plan treatments. It lets us find specific genetic mutations. This way, we can tailor treatments to each patient’s tumor.
What is the role of surgical resection in brain neoplasm treatment?
Surgery is key in treating brain tumors. Our neurosurgeons use advanced tools and techniques. They aim to remove tumors safely and effectively.
What types of radiation therapy are available for brain tumor treatment?
We use different radiation therapies. These include whole-brain radiation and stereotactic radiosurgery. We use tools like Gamma Knife and CyberKnife for precision.
How is chemotherapy used in brain cancer treatment?
Our team uses chemotherapy to fight brain cancer. We consider the blood-brain barrier when choosing agents. Often, we use a combination of drugs.
What are targeted molecular therapies, and how are they used in brain cancer treatment?
Targeted therapies aim at specific genetic mutations. We keep up with new tyrosine kinase inhibitors. We also work to overcome resistance to these treatments.
What is Tumor Treating Fields (TTFields) therapy, and how is it used in brain cancer treatment?
TTFields therapy uses electric fields to stop cancer cells from dividing. We carefully review the evidence. We consider patient factors to ensure the best results.
How can patients access cutting-edge treatment options, such as gene therapy and oncolytic virus treatments?
We help patients get access to new clinical trials and treatments. We guide them through the process. This way, they can try innovative therapies.
What is the importance of supportive and palliative care in brain neoplasm treatment?
We focus on supportive and palliative care. We aim to improve quality of life. Our team works with other specialties for complete care.
How is brain cancer treatment coordinated across different specialties?
Our team takes a multidisciplinary approach. We work with various specialties for a complete treatment plan. This ensures the best outcomes for patients.




































