At Liv Hospital, we know bowel obstruction is a serious issue that needs quick and effective care. We aim to meet international healthcare standards by diagnosing fast and creating personalized treatment plans. This helps avoid serious problems.
We focus on treating blockages quickly to get the best results for our patients. Our team is committed to top-notch healthcare and supporting international patients. In this article, we’ll look at the main steps in treating bowel obstruction and the usual complications it can cause.Learn 7 essential intestinal obstruction treatment steps. Our guide explains the process and common complications to avoid.
Key Takeaways
- Rapid diagnosis is crucial in managing bowel obstruction effectively.
- Personalized treatment plans help prevent serious complications.
- Liv Hospital is committed to advancing international healthcare standards.
- Comprehensive patient support is provided throughout the treatment process.
- Understanding bowel obstruction pathophysiology is essential for effective care.
The Pathophysiology of Bowel Obstruction
Understanding bowel obstruction is key to managing it well. It involves complex processes that stop the intestine from moving contents as it should.
Mechanical vs. Functional Obstruction
Bowel obstructions are either mechanical or functional. Mechanical obstruction happens when something physically blocks the intestine. On the other hand, functional obstruction is when the intestine’s muscles don’t work right, even without a blockage.
Fluid and Gas Accumulation Mechanisms
Fluid and gas building up above the blockage is a big part of bowel obstruction. This buildup raises pressure inside the intestine, causing swelling in the bowel wall.
Progression to Bowel Wall Edema
As pressure goes up, it cuts off blood to the bowel wall, causing swelling. This swelling makes the intestine smaller, making the blockage worse.
Development of Intestinal Ischemia
If not treated, the swelling and pressure can lead to a serious problem. Intestinal ischemia happens when the intestine doesn’t get enough blood, which can cause tissue death.
| Mechanism | Description | Consequences |
| Mechanical Obstruction | Physical blockage within the intestine | Fluid and gas accumulation, bowel wall edema |
| Functional Obstruction | Disruption in normal muscular contractions | Impaired intestinal motility, potential for ischemia |
| Fluid and Gas Accumulation | Increased intr al pressure | Bowel wall edema, ischemia |
| Bowel Wall Edema | Impaired blood flow | Ischemia, potential necrosis |
Small Bowel Obstruction Pathophysiology: A Closer Look
Understanding small bowel obstruction is key to managing it well. We’ll look into its unique features and why it matters.
Unique Features of Small Bowel Obstruction
Small bowel obstruction has special characteristics. Fluid and gas build up, causing bowel wall edema and possibly ischemia.
The presence of dilated loops of small intestine is a key sign. These can be seen on X-rays and are important for diagnosis.
Dilated Loops of Small Intestine: Clinical Significance
Dilated loops show how serious the obstruction is. They help doctors decide on treatment and if surgery is needed.
| Clinical Finding | Significance | Implication |
| Dilated Loops | Indicates obstruction severity | Guides treatment decisions |
| Bowel Wall Edema | Potential for ischemia | Increased risk of complications |
| Fluid and Gas Accumulation | Obstruction consequence | Requires decompression |
Closed-Loop Obstruction Mechanisms
A closed-loop obstruction happens when intestine is blocked at two places. This is very dangerous and needs quick action.
Fecalization in Small Bowel Obstruction
Fecalization means the intestine’s contents become solid and like feces. This is common in small bowel obstruction and is important for treatment.
We’ve looked into the complex details of small bowel obstruction. Its unique features and importance are crucial for proper care.
Most Common Causes of Small Bowel Obstruction
Small bowel obstruction often stems from a few main causes. Knowing these is key to creating good treatment plans and better patient care.
Adhesions: The Primary Culprit
Adhesions are the top reason for small bowel obstruction, especially in those who’ve had surgery before. These bands can tie loops of the intestine together or to other parts of the belly. This can block the intestine and affect how we treat SBO.
Hernias and Their Complications
Hernias also cause small bowel obstruction. If a hernia traps part of the intestine, it can block the intestine and lead to serious problems. Finding and fixing hernias early is crucial to avoid severe issues.
Tumors and Malignancies
Tumors, both good and bad, can block the intestine. They can either block the inside of the intestine or press on it from outside. We should think about cancer in people with SBO, especially those who’ve had cancer before.
Bowel Obstruction Due to Extraluminal Compression
Extraluminal compression happens when something outside the intestine, like a mass or abscess, presses on it. This shows how important it is to look at outside factors when diagnosing and treating SBO. We must watch out for this complication in our patients.
Clinical Presentation and SBO Diagnosis
Knowing the main symptoms of intestinal blockage is key for diagnosing SBO. The signs of small bowel obstruction (SBO) can change based on how bad the blockage is and where it is.
Cardinal Symptoms of Intestinal Obstruction
People with SBO usually have stomach pain, nausea, and vomiting. The pain often comes and goes and can make the belly look bigger. Nausea and vomiting are worse in blockages closer to the top, and a bigger belly is a sign of blockages further down.
Physical Examination Findings
Checking the belly might show tenderness, muscle tightness, and visible bowel loops. Listening to the belly with a stethoscope can reveal high-pitched sounds or tinkling, which means the bowel is blocked.
Visible Bowel Loops: What They Indicate
Seeing bowel loops means the belly is very swollen, often due to a complete or high-grade blockage. This is a big sign that might mean you need quick action.
Differentiating Partial vs. Complete Obstruction
Telling apart partial and complete blockages is important for choosing the right treatment. Complete blockages need stronger treatment, like surgery, while partial ones might be treated without surgery.
| Clinical Feature | Partial Obstruction | Complete Obstruction |
| Abdominal Pain | Intermittent | Constant |
| Nausea and Vomiting | May be absent or mild | Often severe |
| Bowel Distension | Mild to moderate | Significant |
| Visible Bowel Loops | Less common | More common |
Diagnostic Approaches for Intestinal Obstruction
Diagnosing intestinal obstruction needs a mix of clinical checks and advanced tests. We use many tools to find and treat intestinal blockages.
Radiological Assessment
Imaging is key in spotting intestinal blockages. It shows where and how bad the blockage is.
- X-rays: Plain X-rays of the belly can spot swollen bowel and air-fluid levels, signs of blockage.
- CT scans: CT scans give clear pictures of the bowel and nearby areas. They help find the cause and any problems.
- Ultrasound: Ultrasound is great for kids and thin people. It can spot intussusception or other blockage causes.
Laboratory Tests and Markers
Labs are vital to check the patient’s health and spot any blockage problems.
Important lab tests include:
- Complete Blood Count (CBC) to look for infection or inflammation signs.
- Electrolyte panels to check for imbalances from vomiting or fluid changes.
- Lactate levels to see if there’s bowel ischemia.
Small Bowel Obstruction Pathology
Knowing the cause of small bowel blockage is key for good treatment. Common causes are:
- Adhesions: Fibrotic bands that can tie bowel loops or the bowel to other parts of the belly.
- Hernias: When bowel bulges through a belly wall hole.
- Tumors: Growths, either benign or cancerous, that block the bowel.
By using imaging, lab tests, and knowing the cause, we can accurately diagnose and treat intestinal blockages.
Intestinal Obstruction Treatment: The 7 Key Steps
We treat intestinal obstruction with a detailed plan to help patients get better. This condition is complex, so we use a variety of strategies to care for patients fully.
Step 1: Initial Assessment and Stabilization
The first step is to check the patient’s condition and stabilize them. We look at their medical history, do a physical exam, and run tests. Stabilizing the patient is key and may include fixing dehydration, electrolyte issues, and pain.
Step 2: Nasogastric Tube Decompression
Using a nasogastric tube is a key step to reduce swelling and vomiting. It helps the bowel work better and eases symptoms. It’s important to place and manage the tube correctly to avoid problems.
Step 3: Fluid and Electrolyte Replacement
Replacing lost fluids and electrolytes is crucial. Patients often lose a lot of fluids and electrolytes because of vomiting and swelling. It’s important to replace them to keep the patient stable and help them recover.
Step 4: Pain Management Protocols
Managing pain is a big part of treating intestinal obstruction. We use different methods to keep patients comfortable. We watch and adjust how we manage pain as the patient’s situation changes.
As we move through the 7 key steps, it’s clear that treating intestinal obstruction is complex. Each step is important and builds on the last, making sure patients get the best care.
Conservative Management Approaches
We use conservative management to treat intestinal obstruction. This method is great for patients with partial obstructions or those who can’t have surgery right away.
Bowel Rest Protocol Implementation
Bowel rest is a key part of conservative management. We stop patients from eating to let their bowels rest. This is often done with nasogastric suction to help relieve symptoms.
Fluid Therapy Optimization
Fluid therapy is very important in treating intestinal obstruction. Patients get IV fluids to fix dehydration and electrolyte problems. We watch their fluid levels closely and adjust as needed to keep them hydrated.
Monitoring During Conservative Management
Monitoring is crucial during conservative management. We check the patient’s symptoms, physical condition, and lab results often. This helps us catch any problems early.
When to Escalate Care
Knowing when to move to surgery is important. If a patient doesn’t get better or gets worse, surgery might be needed. We watch for signs like more pain, bowel ischemia, or symptoms that don’t go away.
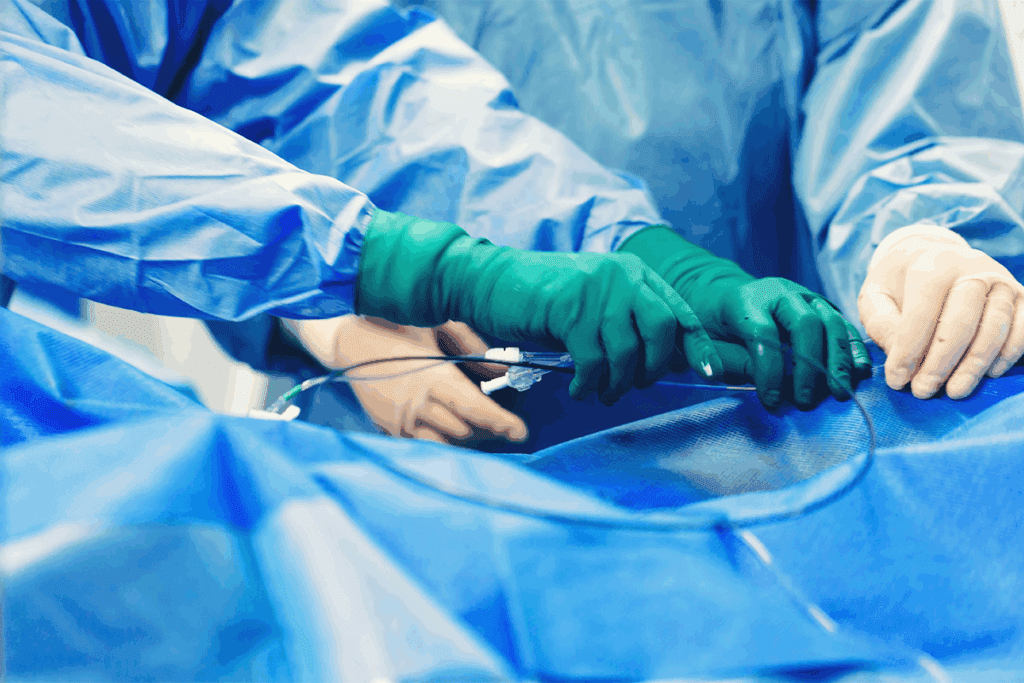
Surgical Interventions for Intestinal Obstruction
Surgery is key in treating intestinal obstruction, especially in emergencies. It’s needed when other treatments don’t work or when complications happen. Surgery helps fix the problem and keeps things from getting worse.
Indications for Emergency Surgery
Emergency surgery is needed for bowel ischemia, perforation, or strangulation signs. These are serious and need quick action to avoid damage and infection. We watch for signs like more pain, fever, or unstable blood pressure, which mean surgery is urgent.
Bowel ischemia is a serious issue that needs fast surgery. It happens when the bowel doesn’t get enough blood, causing damage and possibly gangrene.
Common Surgical Procedures
There are many surgeries for intestinal obstruction, based on the cause and how bad it is. These include:
- Adhesionlysis: Breaking up adhesions that block the bowel.
- Hernia repair: Fixing hernias that might be causing or adding to the blockage.
- Resection and anastomosis: Cutting out the blocked part and joining the healthy ends together.
These surgeries aim to fix the blockage, get the bowel working right, and find and fix the root cause.
Minimally Invasive Techniques
Laparoscopy is a minimally invasive method used for intestinal obstruction. It has benefits like less recovery time, less pain, and smaller scars. But, it depends on the patient’s health and the surgeon’s skill.
Managing Specific Causes
Each cause of intestinal obstruction needs a special surgical plan. For example:
- Adhesions: Usually from past surgeries and might need adhesiolysis.
- Hernias: Must be fixed to stop problems from coming back.
- Tumors: May need the affected part of the bowel removed and possibly chemotherapy.
Knowing the cause of the blockage is key to picking the right surgery.
Complications of Small Bowel Obstruction
It’s important to know about the complications of small bowel obstruction. These can include bowel ischemia, perforation, and sepsis. Quick action is key to avoid long-term damage and improve patient care.
Bowel Ischemia and Gangrene Development
Bowel ischemia happens when the intestine doesn’t get enough blood. This can cause tissue damage. In small bowel obstruction, it might be due to high pressure, swelling, or blocked blood vessels.
If not treated, it can turn into gangrene. This is when parts of the intestine die.
Bowel ischemia is a serious emergency. It needs quick attention. Risks include long blockages, severe blockages, and closed-loop obstructions.
Perforation and Peritonitis
Perforation is another serious issue. It happens when the intestine tears. This lets bacteria into the belly, causing peritonitis.
Peritonitis leads to severe pain, fever, and sepsis. It’s a big deal and needs fast action.
Perforation risks go up with conditions like ischemia or necrosis. Surgery is often needed to fix it and stop more problems.
Sepsis: Recognition and Management
Sepsis is a deadly condition. It happens when the body overreacts to an infection. In SBO, it can come from peritonitis, ischemia, or other infections.
Spotting sepsis early is key. Look for fever, fast heart rate, and low blood pressure. Quick antibiotics and care can help manage it.
SBO Complications: Risk Factors and Prevention
Several things can lead to complications in SBO. These include late diagnosis, health problems, and strangulated obstructions. Knowing these risks helps prevent problems.
Prevention involves early diagnosis and treatment. Also, watching patients closely can help. This way, we can lower the chance of bad outcomes.
Prevention Strategies and Recurrence Reduction
Effective prevention strategies can greatly lower the risk of intestinal obstruction coming back. By knowing and using these strategies, we can help patients get better faster and avoid needing more medical help.
Post-Surgical Adhesion Prevention Techniques
One key way to stop intestinal obstruction from happening again is to prevent post-surgical adhesions. We can do this with several methods, including:
- Using bioresorbable membranes or barriers to prevent adhesion formation
- Employing minimally invasive surgical techniques to reduce tissue trauma
- Administering anti-adhesive agents during surgery
Table: Post-Surgical Adhesion Prevention Techniques
| Technique | Description | Benefits |
| Bioresorbable Membranes | Placing a barrier between tissues to prevent adhesion | Reduces adhesion formation, minimizes complications |
| Minimally Invasive Surgery | Reducing tissue trauma through smaller incisions | Lessens recovery time, reduces adhesion risk |
| Anti-Adhesive Agents | Using agents to prevent adhesions during surgery | Effective in reducing adhesion formation |
Hernia Management and Follow-up
Managing hernias properly is key to preventing intestinal obstruction. This means fixing hernias that could cause problems quickly. It also means following up with patients to watch for any signs of trouble or if the problem comes back.
Dietary and Lifestyle Modifications
Changing what we eat and how we live can help a lot with intestinal obstruction. Patients should:
- Eat a balanced diet full of fiber to help with regular bowel movements
- Avoid foods that can make constipation or gas worse
- Drink plenty of water to keep the bowels healthy and prevent dehydration
Patient Education and Warning Signs
Telling patients about the signs of intestinal obstruction coming back is very important. They should know about symptoms like belly pain, vomiting, and constipation. If they see these signs, they should get help right away.
By using these prevention strategies, we can lower the chance of intestinal obstruction coming back. This helps patients get better faster and avoid needing more medical help.
Conclusion: The Critical Importance of Timely Intervention
Timely intervention is key for treating intestinal obstruction well. At Liv Hospital, we know how important quick medical help is. It helps manage intestinal obstruction and prevents serious problems.
We are dedicated to top-notch healthcare for our patients with intestinal obstruction. We offer support and guidance for international patients. This ensures they get the best treatment.
Good treatment for intestinal obstruction needs a team effort. We are committed to giving our patients the best care. By acting fast, we can greatly improve their chances of recovery and lower the risk of complications.
At Liv Hospital, we aim to make a big difference in our patients’ lives. Our team of experts works hard to make sure our patients get the care they need. This helps them recover from intestinal obstruction.
FAQ
What is intestinal obstruction and how does it occur?
Intestinal obstruction happens when something blocks the intestine. This stops the normal flow of contents. Causes include adhesions, hernias, tumors, or compression from outside.
What are the common symptoms of intestinal obstruction?
Symptoms include abdominal pain, nausea, vomiting, constipation, and swelling. Seeing bowel loops on scans is also a clue.
How is small bowel obstruction diagnosed?
Doctors use scans, lab tests, and tissue exams to diagnose. Seeing dilated bowel loops on scans helps confirm it.
What are the key steps in treating intestinal obstruction?
First, doctors assess and stabilize the patient. They use a tube to drain the stomach and replace lost fluids. They also manage pain. Treatment can be non-surgical or surgery, depending on the cause.
What are the complications of small bowel obstruction?
Complications include bowel ischemia, perforation, peritonitis, and sepsis. Knowing the risks helps prevent these issues.
How can recurrence of intestinal obstruction be prevented?
To prevent recurrence, doctors use special techniques after surgery. They also manage hernias and advise on diet and lifestyle. Educating patients on warning signs is key.
What is the role of surgical intervention in treating intestinal obstruction?
Surgery is crucial for emergencies like bowel ischemia or perforation. It also helps manage adhesions, hernias, and tumors.
How is bowel obstruction due to extraluminal compression managed?
Management focuses on treating the cause of compression. This might need surgery or other treatments, depending on the issue.
What are the unique features of small bowel obstruction pathophysiology?
Small bowel obstruction has unique aspects, like closed-loop obstruction and fecalization. Seeing dilated small intestine loops is a key sign.
References:
Antoniv, M., et al. (2025). Impact of Multi-Institutional Enhanced Recovery after Surgery (ERAS) on morbidity following elective colorectal surgery: A retrospective cohort study. Annals of Surgery. https://pubmed.ncbi.nlm.nih.gov/39812414/



































