Last Updated on November 26, 2025 by Bilal Hasdemir
Bile duct surgery is a complex procedure that needs careful attention and skilled hands. At Liv Hospital, we focus on our patients, making sure they get the best care. It’s important to know about the possible complications and how to handle them.
The surgery comes with risks like infection, bleeding, and bile leaks. Knowing these risks helps us keep our patients safe and build trust with them.
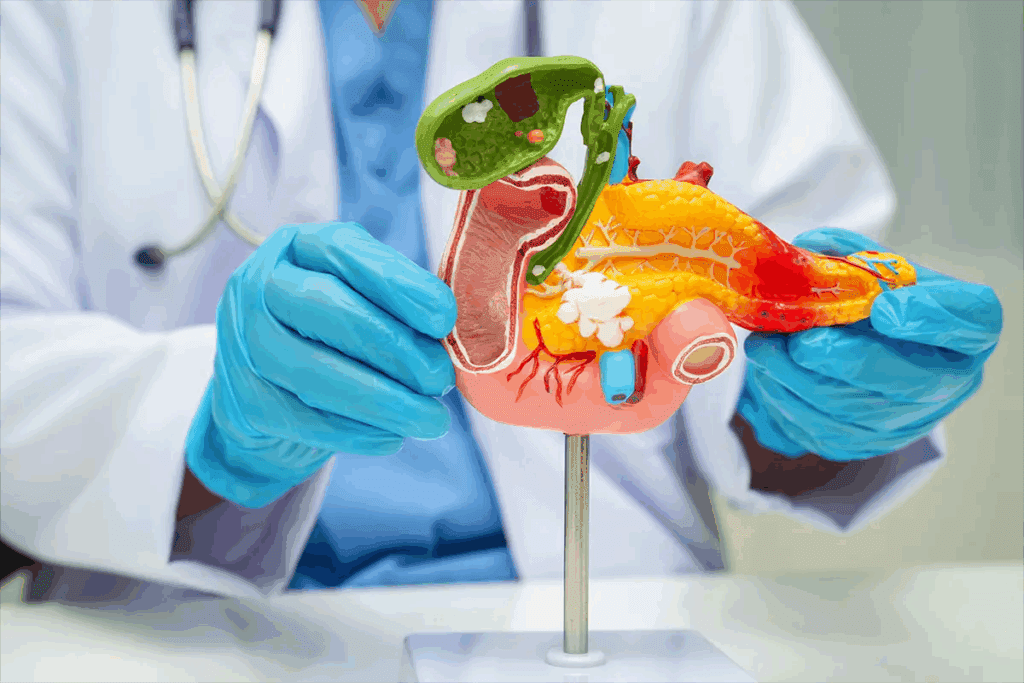
The biliary system is key to digestion. Knowing how it works is vital for successful surgery. It’s a network of organs and ducts that make, store, and move bile. Bile helps digest fats and absorb vitamins.
The biliary system includes the liver, gallbladder, and bile ducts. The liver makes bile, which the gallbladder stores. The bile ducts carry bile to the small intestine for digestion.
The anatomy of the biliary system is complex. The bile ducts merge into the common bile duct. It then joins the pancreatic duct to empty into the duodenum. This setup is key for digestion to work right.
Bile duct surgery treats many conditions. Some common ones are:
| Condition | Description | Treatment |
| Cholangiocarcinoma | Cancer of the bile ducts | Surgery, chemotherapy, radiation therapy |
| Bile Duct Stones | Stones in the bile ducts | Surgery, ERCP, lithotripsy |
| Biliary Strictures | Narrowing of the bile ducts | Dilation, stenting, surgery |
Knowing about these conditions and treatments is key. It helps patients and doctors make good choices. Understanding the biliary system and its problems is essential.

Bile duct surgery includes many procedures, each for different conditions. The choice of surgery depends on the condition, how far it has spread, and the patient’s health.
Bile duct resection removes the damaged part of the bile duct. It’s used for bile duct cancer or severe injuries. The goal is to remove the affected area and restore the bile duct’s function. The extent of the disease determines if it’s partial or complete.
The surgical team uses different techniques to reconnect the bile duct. This ensures bile flows normally into the intestine. Sometimes, a biliary reconstruction is needed to restore bile flow.
Biliary bypass surgery treats bile duct obstruction by creating a detour. This allows bile to flow into the small intestine, bypassing the blockage. Biliary bypass operations can provide significant relief for patients with bile duct blockages, improving their quality of life.
There are various methods for a biliary bypass, like the Roux-en-Y loop. This uses a segment of the intestine for a new bile flow pathway. The method chosen depends on the obstruction’s location and nature.
Minimally invasive surgery is popular for treating bile duct conditions. Techniques like laparoscopic surgery use small incisions for instruments and a camera. This approach can reduce recovery time and minimize scarring, making it appealing for many patients.
These procedures can be for diagnosis or treatment. They can check for blockages or remove stones or dilate narrowed bile ducts.
Surgery is a key part of treating bile duct cancer. It gives hope to those facing this tough disease. Bile duct cancer, or cholangiocarcinoma, needs a detailed treatment plan.
Cholangiocarcinoma surgery uses different methods to remove tumors and fix bile ducts. Surgical resection is usually the main treatment. It aims to remove the tumor completely. Sometimes, liver resection is needed to get rid of all cancer.
The type of surgery depends on the tumor’s location, size, and stage. The patient’s health also plays a role. Minimally invasive techniques are becoming more common. They help with faster recovery and less pain.
After surgery, caring for patients is very important. Monitoring for complications like infections or liver problems is key. Patients also need nutritional support to help with recovery and any digestive issues.
A good follow-up plan is needed to watch for cancer coming back. This includes regular doctor visits and possibly more treatments like chemotherapy or radiation.
The surgery to remove the bile duct is very tricky. This is because the bile duct is near important blood vessels and other organs. This makes the surgery even harder.
Removing the bile duct is like a puzzle. The proximity to vital organs like the liver and pancreas raises the risk of problems. Surgeons must be very careful to avoid harming these areas.
The success of bile duct removal surgery depends a lot on the surgical expertise of the team. Surgeons need a lot of experience in liver and bile duct surgery to handle the challenges.
Understanding the challenges and the need for skilled surgeons helps patients see how complex bile duct removal surgery is.
The time right after bile duct surgery is very important. It’s when doctors watch closely for any problems. These can come from the surgery itself or how the patient reacts to it.
Bleeding or damage to blood vessels is a big worry right after surgery. This can happen for a few reasons, like:
Bleeding can be very dangerous and needs to be found and fixed fast. Vascular injuries can also cause serious problems, like tissues not getting enough blood.
Infections are a big risk right after bile duct surgery. They can be:
Things like pre-existing bile duct obstruction, biliary stents, or immunosuppression can make infections more likely. It’s very important to catch and treat infections early to avoid sepsis.
Problems from anesthesia can also happen right after surgery. These might include:
Watching closely in the PACU is key to spotting and fixing these problems. This helps make sure the patient is safe while coming out of anesthesia.
In short, the time right after bile duct surgery is full of risks. Doctors need to watch closely and act fast to help patients recover well.
Bile leakage is a big problem after biliary procedures. These procedures are done to fix issues with the bile ducts. Even with better surgery and care, bile leaks are a big worry.
Bile leaks happen for many reasons. This includes technical issues during surgery, anatomical variations, and patient-related factors like health conditions. Knowing why they happen helps in preventing and treating them.
By planning carefully before surgery, using precise techniques, and watching patients closely after, we can lower the risk of bile leaks.
Finding bile leaks early is key to managing them well. Tools like imaging studies (e.g., ultrasound, CT scans) and endoscopic retrograde cholangiopancreatography (ERCP) help spot them.
| Diagnostic Tool | Description | Advantages |
| Ultrasound | Non-invasive imaging technique | Quick, non-invasive, and relatively inexpensive |
| CT Scan | Cross-sectional imaging | High sensitivity for detecting fluid collections and bile leaks |
| ERCP | Endoscopic procedure for diagnosing and treating bile duct issues | Allows for both diagnosis and therapeutic intervention |
Managing bile leaks includes conservative management with drainage and antibiotics, endoscopic interventions like stenting, and surgical revision for tough cases. The best approach depends on the leak’s severity, location, and the patient’s health.
Thanks to better diagnostic and treatment methods, outcomes for bile leak patients have gotten better. But, bile leakage is a serious issue that can cause a lot of harm and, in extreme cases, death.
Biliary strictures are a big worry for those who have bile duct surgery. These strictures are when the bile ducts get narrower. This can block bile flow into the intestine, causing problems.
Several things can cause biliary strictures after surgery. These include injury to the bile duct, scar tissue, or inflammation. Knowing what causes them is key to managing and maybe even preventing them.
The formation of biliary strictures is complex. It involves the surgery method, the patient’s body, and how well they recover. Scar tissue formation and chronic inflammation are major reasons for the narrowing.
There are several risk factors for getting biliary strictures. These include:
Dealing with biliary strictures often needs a mix of treatments. The right treatment depends on how bad the stricture is, where it is, and the patient’s health.
| Treatment Option | Description | Advantages |
| Endoscopic Balloon Dilation | A procedure using a balloon to widen the narrowed bile duct. | Minimally invasive, quick recovery |
| Stenting | Placement of a stent to keep the bile duct open. | Effective for maintaining bile duct patency |
| Surgical Revision | Surgical correction of the stricture. | Can be definitive for complex strictures |
Long-term care means watching for when it comes back and managing symptoms. Patients might need to have treatments again to keep the bile duct open.
In summary, biliary strictures are a big problem after bile duct surgery. It’s important to know the risks, how they develop, and the treatment options. This helps improve how well patients do.
It’s important to know about the complications of blocked bile duct surgery. This surgery is often lifesaving but can lead to serious issues. These problems include retained stones, recurrent blockage, and cholangitis.
One big problem is retained stones after surgery. These stones can cause more issues like jaundice and pain. They can even lead to serious infections.
The risk of retained stones comes from a few things:
To prevent and manage retained stones, doctors need to clear the bile duct well. They also watch for signs of problems after surgery.
Recurrent blockage is another issue after surgery. It can happen for reasons like tumor growth or new stones.
The signs of recurrent blockage include:
Early detection is key. Treatment might involve more surgery or endoscopy to fix the blockage.
Cholangitis, an infection of the bile duct, is a serious issue after surgery. If not treated quickly, it can turn into sepsis, a deadly condition.
Cholangitis signs are:
Quick antibiotic therapy and draining the infected bile duct are vital. This helps manage cholangitis and prevent sepsis.
In summary, blocked bile duct surgery can lead to serious complications. These include retained stones, recurrent blockage, and cholangitis. Knowing about these issues and how to manage them is key to better patient care.
It’s important to know about liver problems after biliary surgery. This surgery is often needed but can cause liver issues. These include liver dysfunction and other problems.
Liver problems can happen after bile duct surgery. The liver is key for digestion and metabolism. Any issue with it can cause big problems.
Liver dysfunction can show as jaundice, high liver enzymes, or even liver failure.
Many things can cause liver problems after surgery. These include the reason for surgery, the surgery method, and the patient’s health. Good pre-surgery checks and care after surgery can lower these risks.
The liver can grow back, but removing a big part is risky. This is usually for liver cancer or severe damage.
Removing the right lobe can lead to liver failure, infection, and bleeding. The liver’s ability to heal is important, but it can be weak in patients with liver disease.
In summary, biliary procedures can cause liver issues. Knowing these risks and how to avoid them is key to better patient care.
Complications from bile duct surgery might need a second surgery. This is a big decision that needs careful thought. It’s considered when the first surgery doesn’t work or new problems show up.
Several signs might mean you need another surgery after bile duct surgery. These include:
The results of a second surgery for bile duct problems can be different for everyone. While it can save lives or greatly improve life quality, it also has extra risks. These include:
It’s important for doctors and patients to understand these points before deciding on a second surgery. The choice to have another surgery should be made after weighing the benefits and risks carefully.
Biliary surgery is often needed but can cause long-term issues. These problems can really affect a person’s life quality. It’s key for patients and doctors to know about these risks to better care for them after surgery.
Chronic pain and discomfort are big issues after biliary surgery. This pain can come from surgical scarring, nerve damage, or adhesions. To handle this pain, doctors might use medicine, physical therapy, or even more surgery.
Other treatments like acupuncture or cognitive-behavioral therapy can also help. It’s important for doctors and patients to work together to find the best pain management plan.
Biliary surgery can also cause long-term digestive and nutritional problems. The surgery can mess with how the body digests fats and absorbs vitamins. This might lead to diarrhea, bloating, or fatty stools and could cause nutritional deficiencies if not managed right.
Patients often need to eat a low-fat diet and might need vitamin supplements. Regular check-ups with a doctor or dietitian are key to keep an eye on nutrition and make needed changes.
The mental effects of biliary surgery are also important. Patients might feel anxiety, depression, or fear of recurrence, which can be tough, even if the surgery was for cancer. This mental strain can really impact a person’s life quality.
Using counseling, support groups, and stress management can help a lot. Doctors should know about the mental side of recovery and offer help or refer to mental health experts when needed.
In summary, while biliary surgery is often a lifesaver, it can lead to long-term issues that affect life quality. By understanding these problems and using the right strategies, patients can get the best results from their surgery.
Bile duct surgery is a key treatment for many biliary issues. But, it comes with risks that can affect how well a patient does. We’ve looked at the dangers of these surgeries, from right after the operation to long-term effects on quality of life.
The complexity of bile ducts and their close location to important parts of the body make surgery tricky. Problems like bile leaks, strictures, and liver issues show why skilled surgeons and careful patient care are vital.
It’s key to know about the possible complications of bile duct surgery to improve patient care. By understanding these risks and working to reduce them, doctors can give patients the best chance for a good outcome.
Common issues after bile duct surgery include bleeding and infection. Bile leakage and biliary strictures are also possible. Knowing these risks helps manage patient expectations and aims for the best results.
Removing the bile duct is a complex task. It needs a lot of surgical skill because of its close location to important structures. The surgery’s complexity shows the importance of precise techniques and careful planning.
A biliary bypass operation reroutes bile flow around a blocked or damaged duct. It’s often used to treat bile duct cancer or other blockages.
Yes, the right lobe of the liver can be removed. But, it’s a risky procedure that needs careful thought. It’s usually done for liver cancer or severe liver damage.
Risks of bile duct resection include bleeding, infection, and bile leakage. The complexity of the surgery and the patient’s health can affect these risks.
Bile leakage is managed with drainage, antibiotics, and sometimes more surgery. Quick detection and treatment are key to avoiding more problems.
Biliary strictures are narrowings of the bile duct. They can happen after surgery or due to other reasons. Treatment includes dilation, stenting, and sometimes surgery to repair or bypass the stricture.
Long-term issues can include chronic pain and digestive problems. Nutritional issues and psychological impacts are also possible. Understanding these complications is key to providing full care.
Reoperation might be needed for failed surgery, recurrent blockage, or other complications. The decision to reoperate depends on the patient’s condition and the complication’s nature.
Cholangiocarcinoma surgery treats bile duct cancer. The goal is to remove the tumor and affected ducts. Liver resection might also be involved.
Surgery for bile duct cancer can greatly affect quality of life. Complications, digestive changes, and the psychological impact of cancer diagnosis are factors. Care should address these to improve outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!