Chemotherapy is a key treatment for colorectal cancer. It offers many options to patients. Drugs like 5-fluorouracil (5-FU), oxaliplatin, and capecitabine are often used.
The path through chemotherapy is complex. It involves oral and intravenous chemotherapy drugs. It’s important for patients to understand these options to make good choices about their care.
Liv Hospital is known for its focus on patients. It offers advanced chemotherapy regimens and new oral drugs.
Key Takeaways
- Chemotherapy is a critical treatment for colorectal cancer.
- Various chemotherapy drugs are available, including oral options.
- Liv Hospital offers advanced chemotherapy regimens.
- Understanding treatment options is key to patient care.
- Oral chemotherapy drugs provide an alternative to traditional intravenous treatments.
Understanding Colorectal Cancer and Its Treatment Landscape
Colorectal cancer is a complex disease that requires a deep understanding of its types and stages for the best treatment. Knowledge of chemo for colorectal cancer, along with other therapies, helps both patients and healthcare providers make informed decisions.
Types and Staging of Colorectal Cancer
Colorectal cancer can be classified into different types. The most common is adenocarcinoma, making up about 90% of cases. Other types include carcinoid tumors and gastrointestinal stromal tumors. Knowing the type is key to choosing the right treatment.
The staging of colorectal cancer is also important. The TNM system is commonly used. It looks at the tumor size, lymph node involvement, and metastasis. Stages range from I to IV, with Stage I being the least severe and Stage IV being advanced.
Overview of Treatment Approaches
Treatment for colorectal cancer varies based on several factors. These include the type, stage, and location of the tumor, as well as the patient’s health. The main treatments are surgery, chemotherapy, radiation therapy, and targeted therapy.
Surgery is often the first step for early-stage colorectal cancer. It aims to remove the tumor and the affected colon or rectum. Chemotherapy may be used before or after surgery to kill any remaining cancer cells. Radiation therapy is often used for rectal cancer to lower the risk of recurrence.
In advanced cases, treatment aims to control symptoms and improve quality of life. The treatment plan is tailored to each patient. A team of healthcare professionals works together to find the best approach.
The Role of Chemotherapy for Colorectal Cancer

Chemotherapy is key in treating colorectal cancer. It helps patients at all stages of the disease. This treatment uses drugs to kill cancer cells, making it a vital part of treatment plans.
How Chemotherapy Works Against Cancer Cells
Chemotherapy targets fast-growing cells, like cancer cells. Cytotoxic chemotherapy drugs mess with the DNA of these cells. This stops them from growing and eventually kills them. It helps shrink tumors and stop cancer from spreading.
How well chemotherapy works depends on several things. These include the cancer’s type and stage, and the patient’s health. Knowing how it works helps patients understand its importance in their treatment.
When Chemotherapy Is Recommended
Chemotherapy is suggested for certain stages of colorectal cancer. For stage III, it’s used after surgery to kill any leftover cancer cells. This lowers the chance of cancer coming back. In stage IV, it helps manage symptoms, slow the disease, and improve life quality.
Choosing to use chemotherapy is based on each patient’s situation. Adjuvant chemotherapy aims to prevent cancer from coming back. Neoadjuvant chemotherapy makes tumors smaller before surgery.
Goals of Treatment at Different Stages
The goals of chemotherapy change with the cancer’s stage. Early-stage aims to get rid of cancer cells and stop them from coming back. In advanced stages, it focuses on controlling symptoms, managing pain, and keeping the quality of life good.
Knowing the treatment goals at each stage helps patients talk better with their doctors. They can discuss their treatment options and what to expect.
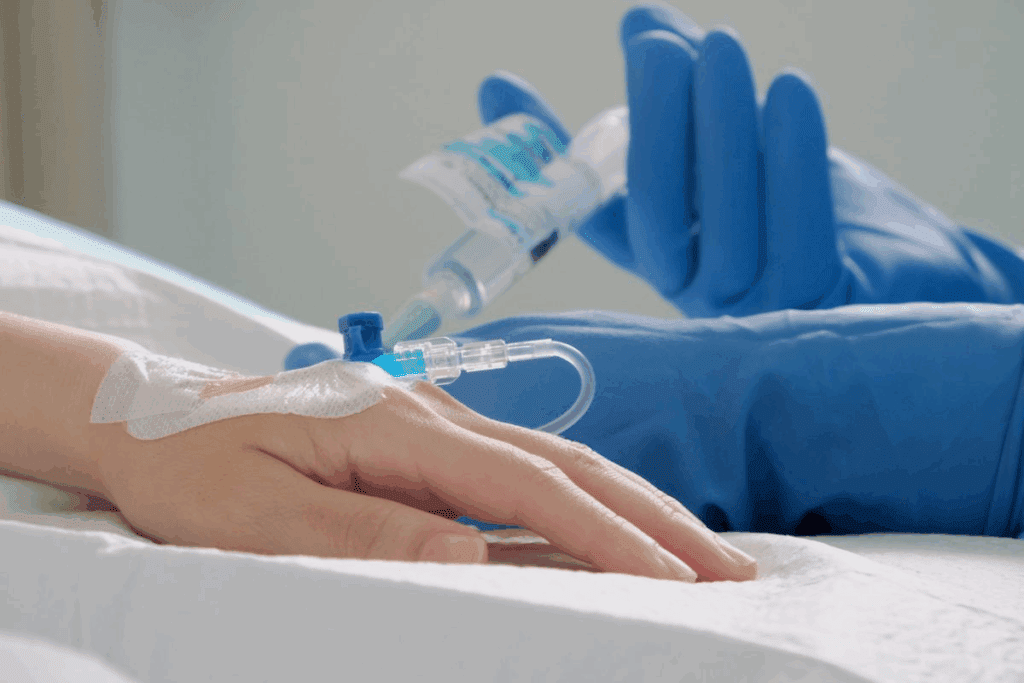
Traditional Intravenous Chemotherapy Drugs
For decades, traditional intravenous chemotherapy drugs have been key in treating colorectal cancer. These drugs are given directly into the bloodstream. They target cancer cells all over the body.
Intravenous chemotherapy treats cancer cells that have spread. This is very important for colorectal cancer. The cancer often spreads to other parts of the body.
5-Fluorouracil (5-FU)
5-Fluorouracil (5-FU) is a mainstay in colorectal cancer treatment. It stops cancer cells from growing by messing with DNA. 5-FU is often mixed with other drugs to work better.
Oxaliplatin
Oxaliplatin is another important drug for colorectal cancer. It damages cancer cells’ DNA, stopping them from making copies. Oxaliplatin is often used in FOLFOX, which has greatly improved survival rates.
Irinotecan
Irinotecan blocks an enzyme that cancer cells need to grow. It’s used in treatments like FOLFIRI. It’s very helpful for patients who haven’t responded to other treatments.
Over the years, how these drugs are used has improved. This makes them more effective and less harsh. Knowing about 5-FU, oxaliplatin, and irinotecan helps doctors create better treatment plans for colorectal cancer patients.
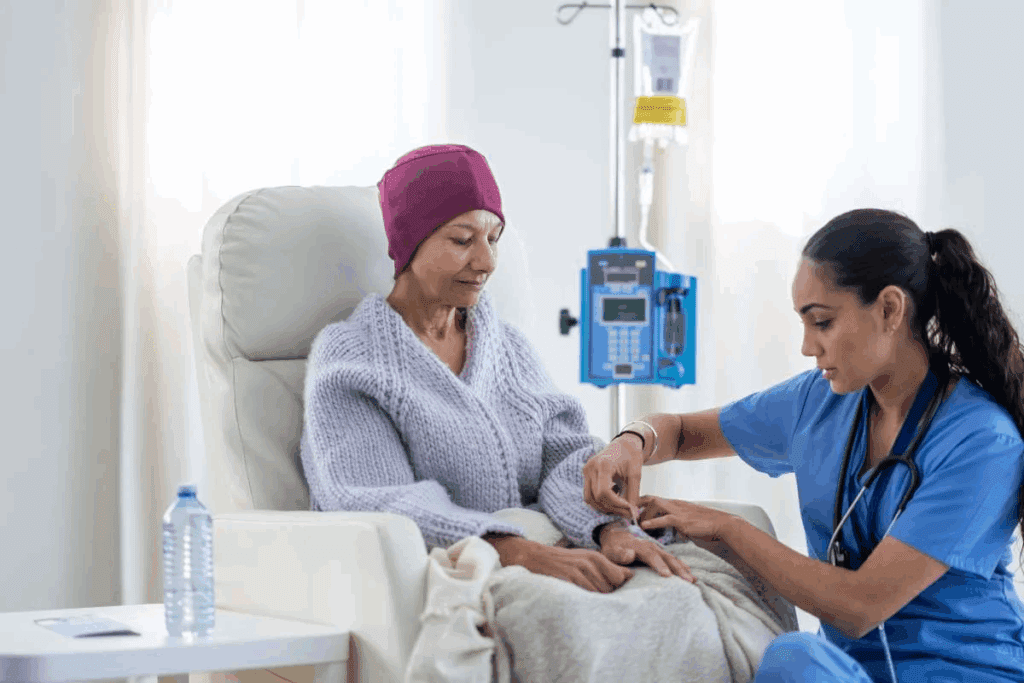
Oral Chemotherapy Drugs for Colon Cancer
Oral chemotherapy drugs have changed how we treat colon cancer. They offer patients easier options. These drugs are a big step forward from traditional intravenous treatments.
Capecitabine (Xeloda)
Capecitabine, or Xeloda, is a key oral drug for colon cancer. It stops cancer cells from growing and kills them. Doctors often give it to patients with stage III colon cancer or those with cancer that has spread.
The doctor will decide how much capecitabine to take and when. This depends on the patient’s health, kidney function, and other medicines they’re on.
Trifluridine-Tipiracil (Lonsurf)
Trifluridine-tipiracil, or Lonsurf, is another oral treatment for colon cancer. It combines trifluridine with tipiracil to boost its effect. This combo is used for patients with advanced colorectal cancer who have tried other treatments.
Lonsurf has been shown to help these patients live longer. It’s a valuable option for those facing tough cancer challenges.
Benefits of Oral Administration
Oral chemotherapy drugs bring many benefits. They’re easy to take at home, which means no more frequent hospital visits. This makes treatment more convenient and flexible.
Being able to manage treatment at home can greatly improve a patient’s quality of life. It’s a big plus for those undergoing chemotherapy.
Adherence and Monitoring Considerations
While oral chemotherapy has many advantages, it’s important to stick to the treatment plan. Patients must take their medicine exactly as told by their doctor. This ensures the best results.
It’s also key for doctors to keep a close eye on patients. They’ll check for side effects and adjust the treatment if needed. This might include blood tests, physical checks, and tracking how well the treatment is working.
Oral Chemotherapy Drugs for Rectal Cancer
Oral chemotherapy drugs are key in treating rectal cancer. They offer a home-based option, reducing hospital visits. This makes treatment more convenient.
Differences in Treatment Approaches
Rectal cancer treatment differs from colon cancer due to location. Oral drugs are used in various stages, often with radiation. This boosts treatment success.
Capecitabine is a top choice for rectal cancer. It’s a prodrug that turns into 5-fluorouracil (5-FU) in the body. This offers a similar effect to 5-FU but is easier to take orally.
Tablet Chemo Options for Bowel Cancer
Several oral chemotherapy options are available for bowel cancer. Capecitabine (Xeloda) and Trifluridine-Tipiracil (Lonsurf) have proven effective in studies.
| Oral Chemotherapy Drug | Mechanism of Action | Common Use in Rectal Cancer |
| Capecitabine (Xeloda) | Converted to 5-FU in the body, inhibiting DNA synthesis | Neoadjuvant and adjuvant therapy, often with radiation |
| Trifluridine-Tipiracil (Lonsurf) | Inhibits thymidylate synthase and DNA synthesis | Used in metastatic disease or when other treatments fail |
Combining Oral Agents with Radiation
Combining oral chemotherapy with radiation is common in rectal cancer treatment. This makes cancer cells more vulnerable to radiation.
Using oral drugs like capecitabine with radiation improves outcomes. This combo can shrink tumors before surgery, leading to better results.
Common Chemotherapy Regimens for Colorectal Cancer
There are several chemotherapy regimens for colorectal cancer. Each has its own strengths and is used in different ways. They aim to kill cancer cells while keeping side effects in check.
FOLFOX Regimen
The FOLFOX regimen combines 5-fluorouracil (5-FU), leucovorin, and oxaliplatin. It’s a top choice for treating colorectal cancer, mainly after surgery to lower the chance of it coming back.
Key Components:
- 5-Fluorouracil (5-FU): A drug that stops DNA synthesis in cancer cells.
- Leucovorin: Makes 5-FU work better.
- Oxaliplatin: Damages DNA in cancer cells.
FOLFIRI Regimen
The FOLFIRI regimen mixes 5-fluorouracil (5-FU), leucovorin, and irinotecan. It’s for advanced colorectal cancer and for those who haven’t responded to other treatments.
Key Components:
- 5-Fluorouracil (5-FU): Stops DNA synthesis in cancer cells.
- Leucovorin: Boosts the effect of 5-FU.
- Irinotecan: Blocks topoisomerase I, an enzyme in DNA replication.
CAPEOX (XELOX) Regimen
The CAPEOX, or XELOX, regimen pairs capecitabine and oxaliplatin. It’s an oral treatment, making it easy to take.
Key Components:
- Capecitabine: Turns into 5-FU in the body.
- Oxaliplatin: Damages DNA in cancer cells.
Single-Agent Regimens
Single-agent chemotherapy is sometimes used. It involves one drug, like capecitabine or 5-FU. It’s for patients who can’t handle combination treatments.
| Regimen | Key Drugs | Common Use |
| FOLFOX | 5-FU, Leucovorin, Oxaliplatin | Adjuvant treatment, reducing recurrence risk |
| FOLFIRI | 5-FU, Leucovorin, Irinotecan | Advanced colorectal cancer |
| CAPEOX (XELOX) | Capecitabine, Oxaliplatin | Oral chemotherapy option |
| Single-Agent | Capecitabine or 5-FU | For patients intolerant to combination regimens |
Adjuvant Chemotherapy After Surgery
After surgery for colorectal cancer, doctors might suggest adjuvant chemotherapy. This treatment aims to kill any cancer cells left behind. It’s given after the main treatment, like surgery.
Reducing Recurrence Risk
The main goal of adjuvant chemotherapy is to reduce the risk of cancer coming back. It targets tiny cancer cells that might have spread. This can greatly improve survival chances and lower the need for more treatments.
Research shows adjuvant chemotherapy works well, mainly for stage III colorectal cancer. The right chemotherapy depends on the patient’s health, cancer stage, and other factors.
Timing and Duration Considerations
The timing and duration of adjuvant chemotherapy are key. It usually starts a few weeks after surgery, when the patient is well enough.
How long it lasts varies, often months. The exact plan depends on the cancer stage, patient health, and how well they respond to treatment.
Patient Selection Criteria
Patient selection criteria for adjuvant chemotherapy are detailed. They look at the cancer stage, overall health, and chemotherapy risks. Those with stage III colorectal cancer usually get it.
Choosing adjuvant chemotherapy is a personal decision. It considers the benefits and risks. Age, other health issues, and personal preferences are important in this choice.
Neoadjuvant Chemotherapy Before Surgery
Neoadjuvant chemotherapy is a key treatment for colorectal cancer. It aims to shrink tumors before surgery. This is very important for patients with large tumors, as it can make surgery easier and safer.
Tumor Shrinkage Goals
The main goal of neoadjuvant chemotherapy is to make tumors smaller. This makes them easier to remove during surgery. It also helps lower the chance of cancer coming back.
Tumor shrinkage happens when chemotherapy drugs kill cancer cells. Doctors use CT scans or MRI to see how much the tumor has shrunk.
Combined Approaches with Radiation
Neoadjuvant chemotherapy is often paired with radiation therapy for better results. This combo helps shrink tumors more and boosts success chances.
This method works well for rectal cancer patients. It helps control the tumor better and lowers the recurrence risk.
Assessing Treatment Response
It’s important to check how well neoadjuvant chemotherapy works. Doctors use CT scans or MRI to see if the tumor has shrunk.
Patients respond differently to treatment. Some tumors shrink a lot, while others don’t change much. Knowing how well the treatment works helps decide what to do next.
Chemo for Colorectal Cancer in Advanced and Metastatic Disease
Chemotherapy helps improve life quality and survival for those with advanced colorectal cancer. It’s used when cancer spreads to other parts of the body, known as metastatic disease.
Palliative Treatment Goals
The main goal of chemotherapy in advanced and metastatic colorectal cancer is palliative care. It aims to ease symptoms and enhance life quality. Chemotherapy can shrink tumors, reducing pain and other symptoms.
Palliative chemotherapy focuses on comfort, not curing the cancer. Treatment choices depend on the patient’s health, disease extent, and personal wishes.
Maintenance Therapy Approaches
Maintenance therapy is used after initial chemotherapy to control the disease. It aims to keep the disease in check and prevent it from getting worse.
- Maintenance therapy may involve a less intense chemotherapy regimen.
- It can also include targeted therapies to control the disease.
- The choice of maintenance therapy depends on the patient’s response to initial treatment and their tolerance.
Integration with Targeted Therapies
Targeted therapies target specific cancer cell traits, stopping their growth and spread. Combining targeted therapies with chemotherapy is now standard for treating advanced and metastatic colorectal cancer.
| Treatment Approach | Description | Benefits |
| Chemotherapy alone | Using chemotherapy drugs to kill cancer cells. | It can be more precise in targeting cancer cells, potentially reducing side effects. |
| Targeted therapy alone | Using drugs that target specific cancer cell characteristics. | It can improve treatment outcomes by attacking cancer cells in multiple ways. |
| Combination of chemotherapy and targeted therapy | Combining chemotherapy with targeted therapies to enhance treatment effectiveness. | Can improve treatment outcomes by attacking cancer cells in multiple ways. |
Combining chemotherapy with targeted therapies is a big step forward in treating advanced and metastatic colorectal cancer. This approach offers more effective treatments tailored to each patient’s needs.
Side Effects of Chemotherapy for Rectal Cancer
Patients with rectal cancer need to know about chemotherapy side effects. Chemotherapy helps fight cancer, but can cause problems that affect daily life.
Common Physical Side Effects
People getting chemotherapy for rectal cancer often face physical side effects. These include fatigue, hair loss, and skin changes. Fatigue is a big issue, making everyday tasks hard.
Managing Gastrointestinal Symptoms
Patients with rectal cancer often have stomach problems from chemotherapy. Symptoms like nausea, diarrhea, and abdominal pain are common. Finding ways to manage these symptoms is key to keeping patients comfortable.
“Using antiemetic drugs and changing what you eat can help a lot with nausea and vomiting from chemo.”
Neurological and Hematological Complications
Chemotherapy can also cause problems with the nervous system and blood. Neuropathy is a common issue, causing numbness and pain in the hands and feet. Blood problems like anemia and neutropenia can make infections more likely.
- Neuropathy can be treated with medicine and other therapies.
- Checking blood regularly is important to catch blood problems early.
Long-Term Effects to Consider
It’s important for patients to know about the long-term effects of chemotherapy. These can include long-term neuropathy, infertility, and a higher risk of getting other cancers. Knowing these risks helps patients make better choices about their treatment.
The American Cancer Society says, “Chemotherapy is good for treating rectal cancer, but talking about long-term effects with your doctor is important for full care.”
Preparing for Chemotherapy and Supportive Care
Getting ready for chemotherapy involves several steps. Knowing what to expect, getting the right nutrition, and managing daily tasks are key. These are all part of supportive care.
What to Expect During Treatment
Chemotherapy can affect your body in many ways. Being prepared can make a big difference. Common side effects include fatigue, nausea, and hair loss.
Your healthcare team will help you manage these side effects. Having a support system is also important. This could be family, friends, or a support group.
Nutritional Support During Therapy
Nutrition is vital during chemotherapy. A balanced diet with fruits, vegetables, and lean proteins can help. Staying hydrated is also key.
Consider talking to a nutritionist for personalized advice. They can help with your dietary needs during treatment.
Managing Daily Activities
Chemotherapy can make it hard to do daily tasks. Prioritizing tasks, taking breaks, and asking for help are important. Plan your schedule around treatment days to avoid disruptions.
Understanding what to expect and having support can help you through chemotherapy. Good preparation and care are essential for a better treatment experience and well-being.
Colorectal Cancer Chemotherapy: The Essential Guide to Oral Drugs, Regimens, and Side Effects
Chemotherapy is a key treatment for colorectal cancer. It uses different regimens and oral drugs.
Drugs like 5-fluorouracil (5-FU), oxaliplatin, and capecitabine help fight colon and rectal cancer.
Liv Hospital offers cutting-edge treatments. They give people the latest knowledge and options.
Key Takeaways
- Chemotherapy is a vital treatment for colorectal cancer.
- Oral drugs like capecitabine are used in various regimens.
- 5-FU and oxaliplatin are commonly used chemotherapy drugs.
- Liv Hospital provides patient-centered care and internationally recognized expertise.
- Advanced regimens and innovative oral drugs are available for treatment.
Understanding Colorectal Cancer and Its Treatment Landscape
It’s important to know about colorectal cancer, including its types and stages. This knowledge helps in choosing the best treatment. Colorectal cancer affects the colon and rectum, with different treatment needs.
Types and Staging of Colorectal Cancer
Colorectal cancer has several types, based on where it starts and how it looks under a microscope. The most common is adenocarcinoma, which comes from glandular cells. Other types include carcinoid tumors and gastrointestinal stromal tumors (GISTs).
The stage of colorectal cancer is key in planning treatment. The TNM system is used to stage it. It looks at the tumor size, lymph node involvement, and whether it has spread. Stages range from I (local) to IV (metastatic).
| Stage | Description | 5-Year Survival Rate |
| I | Cancer is limited to the colon or rectum wall | 90% |
| II | Cancer has grown through the wall, but not tothe nearby lymph nodes | 70-80% |
| III | Cancer has spread to nearby lymph nodes | 40-60% |
| IV | Cancer has metastasized to distant organs or tissues | 10-20% |
Overview of Treatment Approaches
Treatment for colorectal cancer often involves surgery, chemotherapy, radiation therapy, and targeted therapy. The right treatment depends on the cancer’s stage, location, and the patient’s health.
Surgery is key for early-stage cancer, aiming to remove the tumor and affected area. Chemotherapy may be used before or after surgery to kill any remaining cancer cells. Radiation therapy and chemotherapy are often used together for rectal cancer to lower the chance of it coming back.
In summary, knowing about colorectal cancer’s types, stages, and treatments is vital for the best care. A team approach, using the latest in medical technology and research, is essential in fighting this complex disease.
The Role of Chemotherapy for Colorectal Cancer
Chemotherapy plays a key role in treating colorectal cancer. It kills cancer cells by destroying them. This treatment is a big part of the plan for many patients.
How Chemotherapy Works Against Cancer Cells
Chemotherapy drugs target fast-growing cells, like cancer cells. They can be taken by mouth or given through an IV. This helps kill cancer cells all over the body.
Cytotoxic chemotherapy is common for colorectal cancer. It messes with the DNA of cancer cells, stopping them from growing. This is good for cancers that have spread or are likely to spread.
When Chemotherapy Is Recommended
Chemotherapy is suggested for stages III and IV of colorectal cancer. For stage III, it’s used after surgery to kill any leftover cancer cells. This lowers the chance of cancer coming back. In stage IV, it helps control the cancer, ease symptoms, and improve life quality.
Doctors decide on chemotherapy based on the cancer’s stage, the patient’s health, and other conditions. Personalized treatment plans are made for each patient’s needs.
Goals of Treatment at Different Stages
The goals of chemotherapy change with the cancer’s stage. In the early stages, it aims to get rid of any cancer cells left after surgery. This helps prevent it from coming back. In later stages, it focuses on controlling the cancer, easing symptoms, and keeping the quality of life good.
- For stage I and II colorectal cancer, chemotherapy may not be needed unless there are high-risk features.
- For stage III, chemotherapy is standard to reduce recurrence risk.
- For stage IV, chemotherapy is used to control cancer growth and alleviate symptoms.
It’s important for patients and doctors to understand chemotherapy’s role at different cancer stages. This helps make better treatment choices.
Traditional Intravenous Chemotherapy Drugs
Intravenous chemotherapy drugs like 5-fluorouracil, oxaliplatin, and irinotecan are key in treating colorectal cancer. They are used at different stages of the disease, alone or with other treatments.
5-Fluorouracil (5-FU)
5-Fluorouracil (5-FU) is a mainstay in colorectal cancer treatment. It stops cancer cells from growing by messing with DNA synthesis. 5-FU is often given with other drugs to boost its power.
Oxaliplatin
Oxaliplatin is another important drug for colorectal cancer. It harms cancer cells’ DNA, stopping them from multiplying. Oxaliplatin is often part of FOLFOX, which has greatly improved survival rates.
Irinotecan
Irinotecan works by blocking an enzyme cancer cells need to grow. Irinotecan is used for metastatic colorectal cancer and is given with other drugs.
The table below shows the main points of these drugs:
| Drug | Mechanism of Action | Common Use |
| 5-Fluorouracil (5-FU) | Interferes with DNA synthesis | Colorectal cancer treatment |
| Oxaliplatin | Colorectal cancer, often in the FOLFOX regimen | Colorectal cancer, often in FOLFOX regimen |
| Irinotecan | Inhibits topoisomerase I | Metastatic colorectal cancer |
It’s vital to know how these drugs work for effective treatment plans. By mixing these drugs, doctors can create treatments that fit each patient’s needs.
Oral Chemotherapy Drugs for Colon Cancer
Oral chemotherapy drugs are key in fighting colon cancer. They are easy to take and cut down on hospital visits. This makes treatment more flexible for patients.
Capecitabine (Xeloda)
Capecitabine, or Xeloda, is a pill for colon cancer. It stops cancer cells from growing and kills them. It’s often given to stage III colon cancer patients or those with spread disease.
Trifluridine-Tipiracil (Lonsurf)
Trifluridine-tipiracil, or Lonsurf, is another pill for colon cancer. It’s for those who’ve tried other treatments. It helps these patients live longer.
Benefits of Oral Administration
Oral chemotherapy has many advantages:
- It’s easy to take at home, cutting down on hospital trips.
- It fits well into daily life.
- It lowers the chance of getting infections.
Adherence and Monitoring Considerations
Oral chemotherapy needs careful following and checking up. Patients must take their pills as told. Regular visits are key to watching for side effects and adjusting doses. Doctors are vital in teaching patients how to use these pills and handling side effects.
Knowing about oral chemotherapy helps colon cancer patients make smart choices. They can work with their doctors to get the best results.
Oral Chemotherapy Drugs for Rectal Cancer
Oral chemotherapy drugs are becoming more common for treating rectal cancer. They offer a new option compared to traditional intravenous treatments. This change aims to better patient outcomes and improve their quality of life.
Differences in Treatment Approaches
Rectal cancer treatment differs from colon cancer treatment. This is mainly because of the rectum’s location and the risk of local recurrence. Oral chemotherapy drugs are key in these treatments.
One big difference is the use of radiation therapy with chemotherapy for rectal cancer. This combo aims to shrink tumors before surgery. It makes the surgery easier and could lead to better results.
Tablet Chemo Options for Bowel Cancer
Capecitabine (Xeloda) is a popular oral chemotherapy drug for rectal cancer. It turns into 5-fluorouracil (5-FU) in the body, killing cancer cells. Taking it orally means fewer hospital visits compared to intravenous treatments.
Trifluridine-tipiracil (Lonsurf) is another option for advanced colorectal cancer, including rectal cancer. It’s great for patients who have tried other treatments.
Combining Oral Agents with Radiation
Using oral chemotherapy with radiation therapy is common for rectal cancer. This mix makes radiation work better by making cancer cells more sensitive.
For instance, capecitabine is often paired with radiation therapy for rectal cancer. This combo can help tumors shrink more and lead to better surgery results.
It’s important for patients to talk to their healthcare provider about the benefits and risks of this combination. This helps find the best treatment plan for each patient.
Common Chemotherapy Regimens for Colorectal Cancer
Colorectal cancer treatment often includes specific chemotherapy plans. Each plan has its own benefits and side effects. These plans aim to kill cancer cells and help patients recover.
FOLFOX Regimen
The FOLFOX regimen combines folinic acid (leucovorin), 5-fluorouracil (5-FU), and oxaliplatin. It’s used to treat colorectal cancer, mainly after surgery, to lower the recurrence risk.
Key components:
- Folinic acid (leucovorin): Boosts 5-FU’s effectiveness
- 5-Fluorouracil (5-FU): Stops DNA synthesis in cancer cells
- Oxaliplatin: Damages DNA in cancer cells, stopping them from replicating
FOLFIRI Regimen
The FOLFIRI regimen includes folinic acid (leucovorin), 5-fluorouracil (5-FU), and irinotecan. It’s for advanced colorectal cancer and for those who didn’t respond to other treatments.
Key components:
- Folinic acid (leucovorin): Enhances 5-FU’s effect
- 5-Fluorouracil (5-FU): Stops DNA synthesis in cancer cells
- Irinotecan: Blocks topoisomerase I, an enzyme in DNA replication
CAPEOX (XELOX) Regimen
CAPEOX, or XELOX, combines capecitabine and oxaliplatin. It’s an oral treatment for colorectal cancer, making it easy to take.
Key components:
- Capecitabine: Becomes 5-FU in the body, stopping DNA synthesis in cancer cells
- Oxaliplatin: Damages DNA in cancer cells, stopping them from replicating
Single-Agent Regimens
Single-agent chemotherapy is sometimes recommended. This is for patients who can’t handle combination treatments or have certain health issues. Common single agents are capecitabine, 5-FU, or irinotecan.
| Regimen | Key Drugs | Common Use |
| FOLFOX | 5-FU, Oxaliplatin, Leucovorin | Adjuvant treatment, advanced disease |
| FOLFIRI | 5-FU, Irinotecan, Leucovorin | Advanced colorectal cancer |
| CAPEOX (XELOX) | Capecitabine, Oxaliplatin | Adjuvant and metastatic colorectal cancer |
| Single-Agent | Capecitabine, 5-FU, Irinotecan | Patients with contraindications to combination therapy |
Choosing a chemotherapy plan for colorectal cancer depends on many factors. These include the cancer’s stage, the patient’s health, and past treatments. Knowing about these plans helps patients make better choices for their care.
Adjuvant Chemotherapy After Surgery
After surgery for colorectal cancer, doctors might suggest adjuvant chemotherapy. This treatment aims to kill any cancer cells left behind. It helps lower the chance of cancer coming back.
Reducing Recurrence Risk
The main goal of adjuvant chemotherapy is to fight cancer cells that might have spread. These cells are too small to see, but they can cause cancer to come back. By getting rid of these cells, chemotherapy can help patients live longer and avoid more treatments.
- Key Benefits: Reduces the risk of cancer recurrence
- Improves long-term survival rates
- Minimizes the need for additional treatments
Timing and Duration Considerations
The timing and length of adjuvant chemotherapy vary. It depends on the cancer’s stage, the patient’s health, and treatment goals. Usually, it starts a few weeks after surgery, when the body is recovering.
Duration: How long chemotherapy lasts can be from a few months to several. It depends on the treatment plan and how well the patient responds.
Patient Selection Criteria
Not every colorectal cancer patient needs adjuvant chemotherapy. Doctors look at the cancer’s stage, lymph node involvement, and overall health. Patients with stage III cancer usually get chemotherapy. Those with stage II might get it if they have certain risk factors.
Neoadjuvant Chemotherapy Before Surgery
Neoadjuvant chemotherapy is a treatment used before surgery. It aims to shrink the tumor and kill any cancer cells that may have spread.
Tumor Shrinkage Goals
The main goal of neoadjuvant chemotherapy is to make the tumor smaller. This makes surgery easier and less invasive. Tumor shrinkage also boosts the chances of a successful surgery.
Combined Approaches with Radiation
Neoadjuvant chemotherapy is often paired with radiation therapy. This combo is great for patients with rectal cancer. It helps control the tumor and lowers the risk of it coming back. The mix of chemotherapy and radiation can lead to better results.
Assessing Treatment Response
After neoadjuvant chemotherapy, it’s key to check how well the treatment worked. Imaging, like an MRI or CT scan, shows how much the tumor has shrunk. This helps doctors decide if they should go ahead with surgery or change the treatment plan.
Chemo for Colorectal Cancer in Advanced and Metastatic Disease
For those with advanced or metastatic colorectal cancer, chemotherapy is key. It aims to improve life quality and extend life. Treatment involves different chemotherapy plans and targeted therapies.
Palliative Treatment Goals
The main goal of chemotherapy in advanced and metastatic colorectal cancer is palliative care. It focuses on easing symptoms, improving life quality, and extending life. Palliative treatment goals are met by choosing the right chemotherapy agents and plans.
Good palliative care manages symptoms like pain, nausea, and fatigue. This helps patients do daily activities better. Chemotherapy plans are made to fit each patient’s needs and health.
Maintenance Therapy Approaches
Maintenance therapy is key in managing advanced and metastatic colorectal cancer. It keeps treating the disease after the first round of chemotherapy. Maintenance therapy approaches might include less intense chemotherapy or targeted therapy.
Choosing maintenance therapy depends on several things. These include how well the patient responded to initial treatment, how well they can handle therapy, and their overall health. The aim is to keep the disease under control while keeping the quality of life high.
Integration with Targeted Therapies
Combining chemotherapy with targeted therapies is now common in treating advanced and metastatic colorectal cancer. Targeted therapies, like bevacizumab and cetuximab, target specific cancer growth and progression mechanisms.
Adding targeted therapies to chemotherapy can improve treatment results. It can lead to better response rates and longer survival. The choice of targeted therapy depends on the tumor’s molecular characteristics, like KRAS mutation status.
Side Effects of Chemotherapy for Rectal Cancer
Patients with rectal cancer need to know about chemotherapy side effects. Chemotherapy helps fight cancer, but can cause issues that affect daily life.
Common Physical Side Effects
People with rectal cancer who get chemotherapy often face physical side effects. These can include:
- Fatigue
- Nausea and vomiting
- Diarrhea or constipation
- Hair loss
- Mouth sores
Managing these side effects is key to keeping quality of life high. For example, there are medicines to help with nausea and vomiting.
Managing Gastrointestinal Symptoms
Gastrointestinal symptoms are common in chemotherapy patients with rectal cancer. Effective management of these symptoms can greatly improve comfort and treatment adherence.
Strategies for managing these symptoms include:
- Dietary changes
- Medications to control diarrhea or constipation
- Adequate hydration
Neurological and Hematological Complications
Chemotherapy can also cause neurological and hematological complications. Neurological issues might include neuropathy, while hematological problems can be anemia, neutropenia, or thrombocytopenia.
Monitoring and managing these complications is vital. Regular blood tests can catch hematological issues early. Adjustments to chemotherapy can help lessen neurological effects.
Long-Term Effects to Consider
Some chemotherapy side effects for rectal cancer can last a long time. These may include:
- Permanent neuropathy
- Increased risk of secondary cancers
- Cardiovascular issues
Knowing about these long-term effects is key for patients to make informed treatment choices.
Preparing for Chemotherapy and Supportive Care
When you start chemotherapy, knowing what to expect is key. It’s a big part of treating colorectal cancer. Being ready can help you handle the treatment better.
What to Expect During Treatment
Chemotherapy gives you medicine that fights cancer cells. You’ll get treatment in cycles, with breaks in between. Knowing your treatment plan helps you prepare.
Common side effects include feeling tired, nausea, and losing hair. Your doctor will talk about these and how to deal with them.
Nutritional Support During Therapy
Eating well is important during chemotherapy. A balanced diet keeps you strong and full of energy. Eat lots of fruits, veggies, whole grains, and lean meats.
Drinking water is also key. It helps with side effects like constipation and tiredness.
Managing Daily Activities
Chemotherapy changes how you do daily tasks. You need to pace yourself and choose what’s most important. Making a schedule helps balance rest and activity.
Having support from loved ones is vital. Don’t be afraid to ask for help with chores, errands, or just being there for you.
Conclusion
Chemotherapy is key in treating colorectal cancer. It offers many options, like oral and intravenous drugs. Knowing about different treatments, like FOLFOX and CAPEOX, and oral drugs like capecitabine, is important.
Using chemotherapy for colorectal cancer can lower the risk of the cancer coming back. It can also make tumors smaller and help people live longer. Chemotherapy is used before or after surgery to help manage the disease.
People with colon cancer chemotherapy or rectal cancer chemotherapy should know about possible side effects. They should talk to their healthcare team to handle these issues. This way, patients can make good choices about their care.
In the end, colorectal cancer chemotherapy is a big part of treatment. Using it well can really help patients.
FAQ
What is chemotherapy for colorectal cancer?
Chemotherapy for colorectal cancer uses drugs to kill cancer cells. It can be taken by mouth or given through an IV. It’s often used with surgery and radiation therapy.
What are the different types of chemotherapy drugs used for colorectal cancer?
Chemotherapy drugs for colorectal cancer include 5-FU, oxaliplatin, and irinotecan. There’s also capecitabine and trifluridine-tipiracil. These drugs can be taken orally or through an IV. They’re often mixed or have better results.
What are the benefits of oral chemotherapy for colon cancer?
Oral chemotherapy for colon cancer is convenient. It means fewer hospital visits. You can take it at home. Drugs like capecitabine and trifluridine-tipiracil are commonly used.
How does chemotherapy work against cancer cells?
Chemotherapy stops cancer cells from growing and dividing. It damages their DNA. This makes it hard for them to reproduce and eventually kills them.
What are the common chemotherapy regimens used for colorectal cancer?
Common regimens include FOLFOX, FOLFIRI, and CAPEOX. Single-agent regimens are also used. These combinations aim to get the best treatment results.
What is adjuvant chemotherapy, and when is it used?
Adjuvant chemotherapy is given after surgery to lower cancer recurrence risk. It’s often used for colorectal cancer. The timing and length depend on the patient’s situation.
What are the side effects of chemotherapy for rectal cancer?
Side effects include fatigue, nausea, and diarrhea. There can also be neurological and hematological issues. Managing these side effects is key.
How can I prepare for chemotherapy and manage daily activities?
Preparing for chemotherapy means understanding what to expect and staying nourished. You can also plan how to manage daily tasks. Your healthcare team can help with a personalized plan.
What is the role of neoadjuvant chemotherapy in treating colorectal cancer?
Neoadjuvant chemotherapy is given before surgery to shrink tumors. It’s often paired with radiation therapy. This approach aims for the best treatment outcomes.
How is chemotherapy used to treat advanced and metastatic colorectal cancer?
Chemotherapy controls symptoms and slows disease growth in advanced cancer. It improves quality of life. Treatment goals focus on comfort and slowing disease progression.
What is the difference between chemotherapy for colon cancer and rectal cancer?
The same drugs are used for both, but treatment plans differ. Rectal cancer might need more intense treatment, like radiation therapy, for better results.
Can chemotherapy be used in combination with targeted therapies?
Yes, chemotherapy can be paired with targeted therapies for colorectal cancer. This combination targets specific cancer growth mechanisms, improving treatment results.
References
- Garruti, G., et al. (2018). Cholecystectomy: a way forward and back to metabolic disease? Current Opinion in Lipidology, 29(3), 189-195. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8114797/









