Last Updated on November 26, 2025 by Bilal Hasdemir
A broken back can change your life, but with the right care, you can heal. At places like Liv Hospital, you get all the help you need to get better.
We know how important the right broken back treatment is. We aim to teach you about the backbone fracture treatment choices and what to expect while you recover.
Key Takeaways
- Proper care and advanced medical technology are key for healing a broken back.
- Trustworthy medical centers offer detailed guidance to patients.
- There are many treatment options for backbone fractures.
- Knowing the recovery process is key for patients.
- Getting expert care and advice is essential for a good recovery.
What Is a Broken Back?

A broken back is when the vertebrae in your spine fracture. This is a serious injury that can greatly affect your health and life.
Definition and Anatomy of the Spine
The spine, or backbone, is made up of vertebrae, discs, and ligaments. These parts work together to support, move, and protect your body. The vertebrae are key, helping to absorb shock and distribute weight.
The spine has five main parts: cervical, thoracic, lumbar, sacrum, and coccyx. The lumbar region is often where fractures happen because it carries a lot of weight.
Types of Vertebral Fractures
There are several types of vertebral fractures, each with its own cause and effect. The main ones are:
- Compression fractures: These happen when a vertebra collapses, often because of osteoporosis or injury.
- Burst fractures: These are more severe, where the vertebra breaks into pieces, possibly harming nearby nerves.
- Osteoporotic fractures: These occur when bones weaken due to osteoporosis, making them more likely to break.
Knowing about these different fractures is key to figuring out the right treatment. Each fracture type needs a specific approach to heal and recover.
Common Causes of Backbone Fractures
It’s important to know why backbone fractures happen. These fractures can really affect a person’s life. We’ll look at what causes them, so you can understand the risks and how to avoid them.
Traumatic Injuries
Traumatic injuries often lead to backbone fractures. These injuries can come from:
- Motor vehicle accidents
- Falls from heights
- Sports injuries
- Violent incidents
The force from these incidents can break vertebrae. How bad the fracture is depends on the trauma’s intensity.
Osteoporosis-Related Fractures
Osteoporosis weakens bones, making them more likely to break. It can cause:
- Compression fractures
- Vertebral collapse
These fractures often happen to older adults or those with bone loss. It’s key to catch and treat osteoporosis early to prevent fractures.
Pathological Fractures
Pathological fractures happen when a disease weakens bones. Conditions like:
| Disease | Description |
| Cancer | Tumors can metastasize to the spine, weakening vertebrae. |
| Osteomyelitis | Infection of the bone can compromise its integrity. |
| Paget’s Disease | A condition that disrupts normal bone remodeling. |
These fractures show why it’s vital to manage health issues to avoid fractures.
Knowing the causes of backbone fractures helps us take steps to prevent them. We stress the need for preventive actions and timely medical care for backbone health.
If You Break Your Back, What Happens?
Breaking your back can start a chain of reactions in your body. When a vertebra breaks, you might feel pain, have neurological symptoms, and worry about your spine’s stability.
Immediate Physiological Response
The first thing you might feel is pain and swelling. Your body might also go into shock, have muscle spasms, and move less. Pain management is key in the early stages to help you heal.
Some quick reactions include:
- Pain and discomfort at the fracture site
- Muscle spasms to stabilize the area
- Inflammation and swelling
- Potential neurological symptoms due to nerve compression
Potential Nerve Involvement
A broken back can affect your nerves, leading to symptoms like numbness and weakness. In rare cases, it could even cause paralysis. How severe the nerve damage is depends on the fracture’s location and severity.
“The spinal cord is a critical component of the central nervous system, and any injury to it can have significant consequences. Prompt medical evaluation is essential to assess and address any nerve damage.”
Spinal Stability Concerns
Spinal stability is a big worry with a vertebral fracture. The spine’s structure is at risk, which could lead to more problems if not handled correctly. Spinal stability is key to supporting your body and helping you move.
Spinal stability worries include:
- Risk of further injury or fracture
- Potential for spinal deformity
- Need for immobilization and stabilization
Knowing about the body’s quick reactions, nerve issues, and spinal stability is important for managing and recovering from a broken back. We’ll look at these topics more in the next sections.
Recognizing the Symptoms of a Broken Back
It’s key to spot the signs of a broken back early for the best treatment. The symptoms can be sudden and severe or develop slowly.
Immediate Signs and Symptoms
The first signs of a broken lower back include sharp back pain, tenderness, and stiffness. You might find it hard to move or do everyday tasks because of reduced spinal mobility.
- Severe back pain that gets worse with movement
- Tenderness or stiffness in the back
- Visible deformity or abnormal curvature of the spine
- Difficulty walking or maintaining balance
Neurological Symptoms
A broken back can sometimes cause nerve problems. This can lead to:
- Numbness, tingling, or weakness in the limbs
- Loss of bladder or bowel control
- Difficulty with coordination and balance
- Radiating pain or sensations down the arms or legs
Neurological symptoms mean the injury might be serious. You need to see a doctor right away.
When to Seek Emergency Care
If you notice any of these, get emergency help:
- Severe pain or sudden symptoms
- Loss of mobility or trouble walking
- Loss of bladder or bowel control
- Numbness or tingling in the limbs
As a medical expert noted,
“Quick action on vertebral fractures can greatly improve recovery and lower long-term risks.”
Knowing the symptoms of a broken back is critical for quick treatment. If you’re showing these signs, get medical help fast.
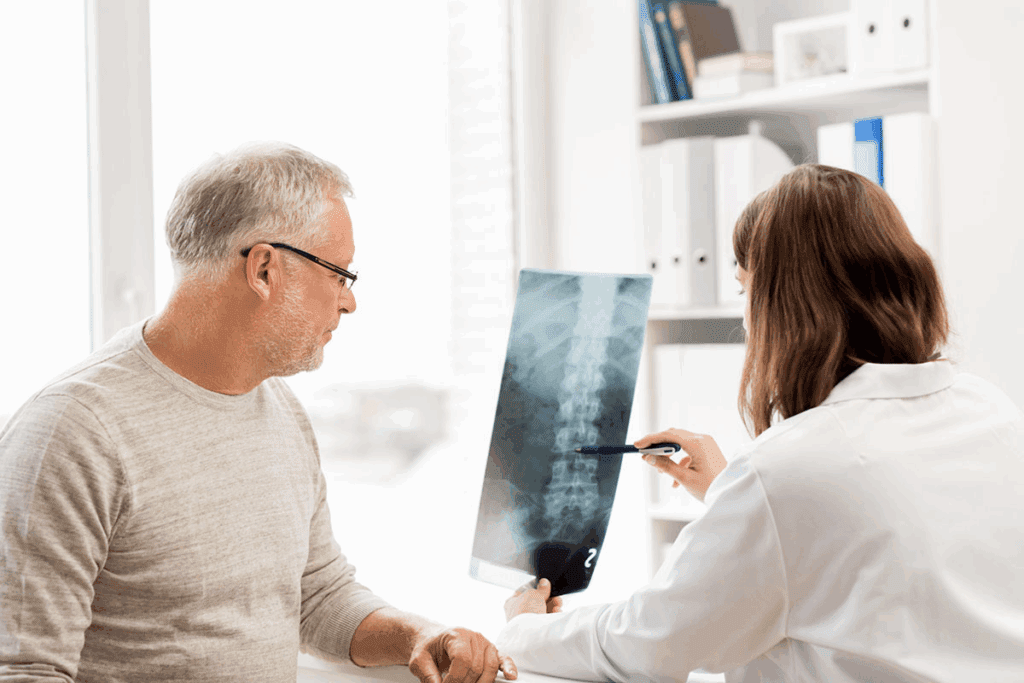
Diagnosis Process for Vertebral Fractures
Diagnosing a broken back involves several steps. We use both clinical checks and advanced imaging. When a patient shows signs of a vertebral fracture, we start a detailed diagnostic process. This helps us understand the injury’s extent and decide on treatment.
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check-up. We look at the patient’s symptoms, how the injury happened, and any past health issues. A physical exam helps us check for pain, tenderness, and nerve function.
Imaging Techniques
Imaging studies are key to confirming a fracture and its severity. We use:
- X-rays: First look at the spine for fractures or deformities.
- Computed Tomography (CT) scans: Show detailed spine images, helping us see how severe the fracture is and if there are fragments or displacement.
- Magnetic Resonance Imaging (MRI): Checks for soft tissue injuries, like ligament or spinal cord damage.
Classification of Fracture Severity
After diagnosing a fracture, we classify its severity. This helps us choose the right treatment. We look at the fracture’s characteristics, like how much the vertebral body has collapsed, any kyphosis, and if the posterior elements are involved.
| Fracture Type | Description | Treatment Approach |
| Stable Compression Fracture | Mild to moderate collapse of the vertebral body without significant kyphosis or posterior element involvement. | Conservative management with bracing and pain management. |
| Unstable Burst Fracture | Significant collapse or fragmentation of the vertebral body, potentially with kyphosis or posterior element fracture. | Surgical intervention may be necessary to stabilize the spine and prevent neurological compromise. |
| Flexion-Distraction Injury | Fracture through the posterior elements, potentially with ligamentous injury. | Treatment depends on the severity and stability, ranging from conservative management to surgical stabilization. |
Getting a correct diagnosis and classification of vertebral fractures is vital. It helps us choose the best treatment, ensuring the best outcomes for patients.
Comprehensive Backbone Fracture Treatment Options
Treating vertebral fractures requires a detailed plan. This plan looks at the fracture’s severity, the patient’s health, and any nerve symptoms. Each treatment is customized to meet the patient’s needs for the best results.
Emergency Management
For acute vertebral fractures, quick action is key. This might include keeping the spine stable, giving pain relief, and sometimes surgery to fix the spine or ease nerve pressure.
Key components of emergency management include:
- Initial assessment and stabilization
- Pain management
- Immobilization
- Surgical intervention when necessary
Treatment Decision Factors
Many things affect how to treat backbone fractures. These include the fracture’s type and how bad it is, any nerve problems, the patient’s age and health, and any other health issues.
| Factor | Considerations |
| Fracture Type and Severity | Stable vs. unstable fractures, compression fractures, burst fractures |
| Neurological Symptoms | Presence of numbness, tingling, weakness, or paralysis |
| Patient’s Age and Health | Comorbidities, bone density, overall physical condition |
Treatment Team Approach
Backbone fracture treatment often needs a team of experts. This team might include orthopedic and neurosurgeons, physical therapists, pain specialists, and rehab experts. Working together, they make sure the patient gets the best care.
By tailoring treatment to each patient’s needs, healthcare teams can help people with vertebral fractures recover well.
Non-Surgical Treatment Approaches
Many patients choose nonsurgical treatments first for vertebral fractures. These methods help the bone heal naturally. They also manage symptoms and prevent more injuries.
Rest and Activity Modification
Rest is key in treating vertebral fractures without surgery. We advise against heavy lifting, bending, or hard activities. These actions can make the condition worse. By changing daily tasks, patients can lower the chance of more harm and help their bones heal.
Bracing and Support Options
Bracing is another way to support the spine without surgery. Orthotic braces help by reducing pain and aiding in healing. They do this by limiting how much the spine moves. The right brace depends on where and how bad the fracture is.
Pain Management Strategies
Managing pain well is important for patients with vertebral fractures. We use medicines, physical therapy, and other methods like acupuncture or chiropractic care. These help control pain and improve life quality.
By using rest, bracing, and pain control, we can treat many vertebral fractures without surgery. This lets patients recover and get back to their usual lives.
How to Fix a Broken Back: Surgical Interventions
When other treatments don’t work, surgery is often the next step for a broken back. Surgery can make the spine stable, reduce pain, and help you move better.
Minimally Invasive Procedures
Modern surgery for back fractures is less invasive. Techniques like vertebroplasty and kyphoplasty fill the broken vertebra with bone cement. This makes it stable and less painful. These surgeries are done under local anesthesia and have quicker recovery times than open surgery.
Spinal Fusion Surgery
Spinal fusion surgery is more complex. It joins two or more vertebrae together using bone grafts and metal rods and screws. It’s used for serious fractures or when the spine is unstable. Though it takes longer to recover, it can offer lasting stability and pain relief.
Post-Surgical Care
After spinal surgery, proper care is key to a good recovery. This includes following a rehab program, managing pain, and seeing your doctor regularly. It’s also important to avoid heavy lifting and bending to prevent more harm.
Knowing about surgical options helps patients make better choices. Whether it’s a less invasive procedure or spinal fusion, the aim is the same. It’s to fix the spine, ease pain, and improve life quality.
Broken Back Healing Time and Recovery Expectations
Recovering from a broken back takes time, from a few weeks to months. The broken back healing time depends on the fracture type and severity. It also depends on your age and health.
Recovery Timeline by Fracture Type
Different fractures heal at different rates. For example:
- Compression fractures, often seen in osteoporosis, can heal in 8-12 weeks with proper care.
- Burst fractures, being more severe, need 3 to 6 months to recover.
- Fracture-dislocations, the most severe, may need surgery and take over 6 months to heal.
Factors Affecting Healing
Several things can impact your recovery from a broken back. These include:
- Age: Older people might heal more slowly because of lower bone density and health issues.
- Nature of the fracture: More complex fractures take longer to heal.
- Treatment approach: Surgery can speed up recovery but also has risks and recovery times.
- Overall health: Conditions like osteoporosis or diabetes can slow healing.
- Adherence to treatment: Sticking to your treatment plan is key for the best recovery.
Knowing these factors and the expected broken back healing time helps plan for recovery. It ensures the best outcomes for patients and healthcare providers.
Physical Therapy and Rehabilitation for Broken Back Recovery
Physical therapy is key for getting back strength and movement after a broken back. We know that healing from a broken back needs a full plan. Physical therapy is a big part of that.
Initial Rehabilitation Phase
The first part of rehab is about handling pain and starting to move gently. We help patients create a special exercise plan that fits their needs and limits.
In this stage, pain management is top priority. Breathing exercises and relaxation methods help reduce pain.
Progressive Strengthening
As patients get better, we focus on progressive strengthening exercises. These help build muscle strength and make the spine more stable. We use things like resistance bands and core strengthening programs.
Return to Daily Activities
Next, patients start to do their daily tasks again. This step uses adaptive equipment and techniques to help them recover safely and get back to normal.
Adaptive Equipment and Techniques
Tools like walkers, canes, and ergonomic furniture help a lot. We also teach the right way to lift and bend to avoid more harm.
We watch how patients are doing and change their treatment as needed. This ensures they get the best recovery possible.
Preventing Complications During Fractured Back Recovery Time
The recovery after a spinal fracture is key. It’s important to prevent complications. Patients face risks that can affect treatment success and life quality.
Managing Pain and Discomfort
Managing pain well is vital during recovery. A mix of medicine, physical therapy, and other methods like acupuncture or relaxation is suggested. It’s essential to work closely with your healthcare provider to find the right balance and avoid side effects.
- Follow the prescribed medication regimen carefully.
- Engage in gentle exercises as recommended by your physical therapist.
- Consider alternative pain management techniques.
Avoiding Secondary Injuries
It’s important to prevent further injury during recovery. Making lifestyle changes and knowing your body’s limits is key. It’s important to avoid heavy lifting, bending, or twisting, as these can make things worse.
- Use proper lifting techniques or avoid lifting heavy objects altogether.
- Modify your home environment to reduce fall risks.
- Wear supportive devices as recommended by your healthcare provider.
Addressing Nerve Damage
Nerve damage is a risk with vertebral fractures. Watching for signs like numbness, tingling, or weakness is important. If you notice these symptoms, seek medical attention promptly.
Psychological Aspects of Recovery
The mental side of recovering from a broken back is significant. Patients might feel anxious, depressed, or frustrated. Seeking support from mental health professionals, family, and friends can help.
Recovering from a vertebral fracture is tough, both physically and mentally. By managing pain, avoiding further injuries, and dealing with nerve damage, patients can improve their recovery.
Conclusion
Recovering from a broken back needs a full plan that includes the right treatment at the right time. We’ve looked into the details of vertebral fractures, like what causes them, how to tell they’re happening, and how to treat them.
Getting the right treatment for a broken back is key to getting better. This can be through non-surgical or surgical methods. A good plan can really help improve how well you recover. We’ve talked about ways to manage pain, help healing, and get back to normal.
We aim to give top-notch help and support to those dealing with vertebral fractures. Knowing the right care and rehab is important. It helps people feel more confident as they go through recovery. We’re here to support you every step of the way.
By using the tips and advice in this article, you can learn how to treat and recover from a broken back. With the right treatment, you can get back to living a full life.
FAQ
What is a broken back?
A broken back, also known as a vertebral fracture, happens when a vertebra in the spine breaks. This can be due to trauma, osteoporosis, or other conditions that weaken bones.
How long does it take to heal a broken back?
Healing time for a broken back varies. It depends on the fracture’s severity, your health, and treatment success. It can take weeks to months for a vertebral fracture to heal.
What are the symptoms of a broken back?
Symptoms include severe back pain, limited mobility, and numbness or tingling in limbs. In severe cases, you might lose bladder or bowel control. Seek medical help if you have these symptoms.
How is a broken back diagnosed?
Diagnosis involves a physical exam, medical history, and imaging like X-rays, CT scans, or MRI. These tests show the fracture’s severity and guide treatment.
What are the treatment options for a broken back?
Treatments range from nonsurgical methods like rest and bracing to surgery. The choice depends on the fracture’s severity and your health.
Can a broken back be treated without surgery?
Yes, many fractures can be treated without surgery. Rest, bracing, and pain management work for stable or less severe fractures.
What is the role of physical therapy in recovering from a broken back?
Physical therapy is key in recovery. It improves mobility, strength, and function. A physical therapist creates a personalized program to aid recovery and prevent future injuries.
How can I prevent complications during recovery from a broken back?
Manage pain well, avoid secondary injuries, and watch for nerve damage signs. Also, address the psychological aspects of recovery to cope with challenges.
What is the recovery timeline for a broken back?
Recovery time varies based on fracture severity and health. It can take weeks to months, with some needing ongoing support.
How do I know if I have a stable or unstable vertebral fracture?
A stable fracture won’t worsen or cause further injury. An unstable fracture might progress or cause complications. A healthcare professional can determine stability through imaging and evaluations.
References
- Eastell, R., Rosen, C. J., Black, D. M., et al. (2019). Pharmacological management of osteoporosis in postmenopausal women: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 104(5), 1595-1622. https://academic.oup.com/jcem/article/104/5/1595/5352476
- McGirt, M. J., Parker, S. L., Wolinsky, J. P., et al. (2009). Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: a meta-analysis. The Journal of Bone & Joint Surgery, 91(6), 1410-1419.
https://journals.lww.com/jbjsjournal/Fulltext/2009/06000/Vertebroplasty_and_Kyphoplasty_for_the_Treatment.20.aspx






