Last Updated on November 25, 2025 by Ugurkan Demir

Learn about a narrowing of arteries that leads to heart strain and reduced flow.
Coronary heart disease (CHD) is a big worry for many people around the world. It often happens when arteries narrow because of plaque buildup, known as atherosclerosis. This makes it hard for blood to reach the heart, raising the chance of heart problems.
As we get older, the risk of CHD goes up. But age isn’t the only factor. What we do and our genes also play big roles. Knowing what causes coronary heart disease risk factors helps us prevent and manage it better.
It’s key to understand atherosclerosis to grasp CHD’s causes and its effects on the heart. Atherosclerosis is when plaque builds up in artery walls, causing them to narrow or block. Factors like high cholesterol, high blood pressure, and smoking play a role in this.
The buildup of low-density lipoprotein (LDL) cholesterol starts the plaque formation in arteries. This cholesterol can oxidize, leading to inflammation and attracting white blood cells. These cells, now foam cells, gather and form plaque, narrowing the arteries and reducing blood flow.
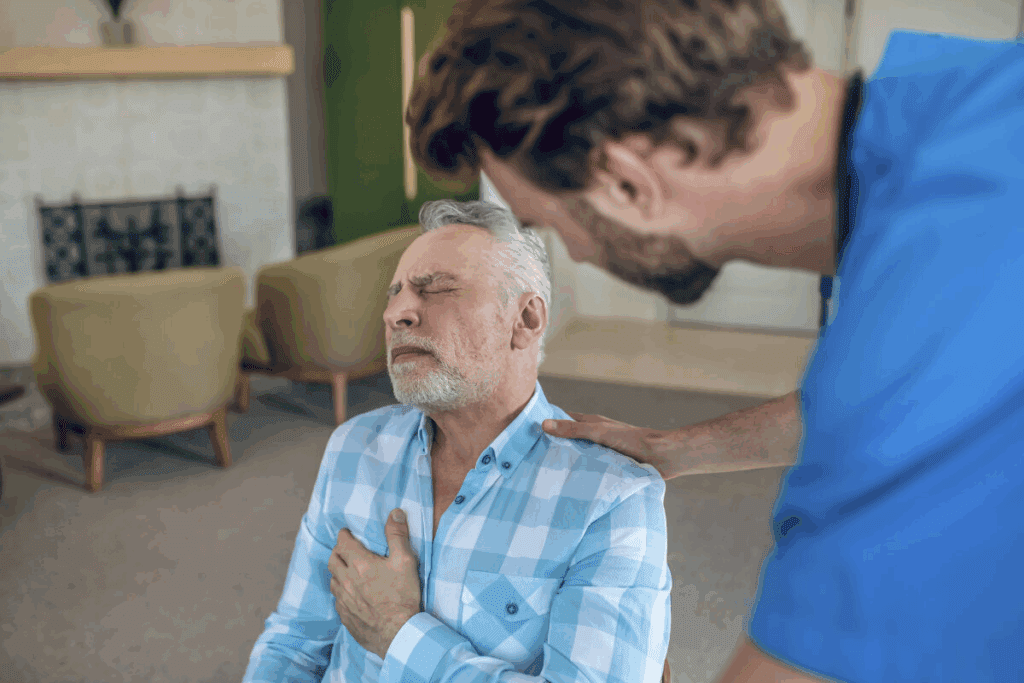
When arteries narrow due to plaque, the heart must work harder to push blood through. This extra effort can cause heart strain, leading to symptoms like chest pain, shortness of breath, or fatigue. If not treated, this strain can lead to heart failure.
It’s important to recognize early signs of artery narrowing. Common symptoms include:
These signs suggest the heart isn’t getting enough blood. If you experience any, seek medical help right away.
| Risk Factor | Description | Impact on Heart Health |
| High Cholesterol | Elevated levels of LDL cholesterol | Increases plaque formation and arterial narrowing |
| Hypertension | High blood pressure | Damages arterial walls, increasing CHD risk |
| Smoking | Tobacco use | Accelerates atherosclerosis and increases CHD risk |

High cholesterol is a big risk for heart disease, mainly because it causes plaque buildup in arteries. Knowing about the different types of cholesterol helps us manage heart health better.
Cholesterol moves through the blood with the help of lipoproteins, which are made of lipids and proteins. There are two main types: LDL and HDL. LDL cholesterol, or “bad” cholesterol, can cause plaque in arteries, raising heart disease risk. HDL cholesterol, or “good” cholesterol, helps clear out extra cholesterol, lowering heart disease risk.
The buildup of LDL cholesterol in arterial walls starts the plaque formation process. This can cause inflammation and attract immune cells, making plaques grow. As plaques get bigger, they can harden and narrow arteries, cutting off blood to the heart and raising CHD risk.
Keeping cholesterol levels in check is key to avoiding heart disease. The American Heart Association suggests these cholesterol levels:
| Cholesterol Type | Optimal Level |
| LDL Cholesterol | Less than 100 mg/dL |
| HDL Cholesterol | 60 mg/dL or higher |
| Total Cholesterol | Less than 200 mg/dL |
By managing cholesterol levels, we can greatly lower the chance of getting coronary heart disease.
Hypertension is a key factor in coronary heart disease (CHD). It damages arteries, raising the risk of CHD. We’ll look at how high blood pressure harms arteries and increases CHD risk.
High blood pressure puts too much pressure on artery walls. This causes them to thicken and harden, known as arteriosclerosis. This makes arteries less able to control blood flow, leading to plaque buildup.
High blood pressure also damages the inner lining of blood vessels, called endothelial dysfunction. This creates inflammation, speeding up atherosclerosis.
Any blood pressure increase raises CHD risk. But, certain levels are more dangerous. A systolic blood pressure of 130 mmHg or higher, or a diastolic of 80 mmHg or higher, is risky.
Even “normal” blood pressures can affect people differently. This depends on age, health, and genetics.
Managing high blood pressure involves lifestyle changes and sometimes medicine. Eating a heart-healthy diet, exercising regularly, and keeping a healthy weight are key. Also, limit alcohol and manage stress.
It’s important to regularly check blood pressure. Working with healthcare providers to create a personalized plan is essential.
Tobacco use harms arterial health, speeding up atherosclerosis and leading to coronary heart disease (CHD). It damages the inner lining of blood vessels, making them more prone to blockages.
Tobacco smoke has thousands of harmful chemicals for the heart. These chemicals can:
Chemicals in tobacco smoke also cause blood clots. This increases the risk of heart attack and stroke. These factors narrow arteries fast, raising the risk of CHD for smokers.
Secondhand smoke is a big risk for CHD. Non-smokers exposed to secondhand smoke face a higher heart disease risk. Secondhand smoke harms the heart, leading to:
Quitting smoking is key to lowering CHD risk. The body starts to heal right after quitting. Here’s what happens:
| Time | Recovery Milestone |
| 20 minutes | Heart rate and blood pressure drop |
| 12 hours | Carbon monoxide level in blood returns to normal |
| 24 hours | Risk of heart attack starts to decrease |
| 1 year | Risk of CHD is cut in half |
| 5 years | Risk of stroke is similar to that of a non-smoker |
| 15 years | Risk of CHD is similar to that of a non-smoker |
Quitting smoking is tough but worth it. With support, people can beat tobacco addiction and lower CHD risk.
It’s important to understand how diabetes affects blood vessels to prevent heart disease. Diabetes mellitus is a condition where blood sugar levels are too high. This can harm blood vessels and raise the risk of heart disease.
Insulin resistance is a step towards type 2 diabetes and harms blood vessels. When cells resist insulin, the pancreas makes more insulin. This can make arteries narrow, raising blood pressure and heart work.
Key effects of insulin resistance on arterial function include:
Type 1 and type 2 diabetes both raise heart disease risk but in different ways. Type 1 diabetes destroys insulin-making cells, causing high blood sugar. Type 2 diabetes, linked to insulin resistance, is more common and also increases heart disease risk.
| Diabetes Type | Primary Cause | CHD Risk Factors |
| Type 1 | Autoimmune destruction of beta cells | High blood sugar, possible ketoacidosis |
| Type 2 | Insulin resistance and impaired insulin secretion | Insulin resistance, bad cholesterol, high blood pressure |
Keeping blood sugar in check is key to avoiding vascular damage and heart disease. Lifestyle changes like diet and exercise are important. Medication may also be needed.
Effective glycemic control strategies:
Excess weight is linked to coronary heart disease (CHD). Obesity plays a big role in narrowing arteries. It’s important to know how obesity harms heart health and leads to CHD.
Visceral fat is bad for the heart. It releases harmful substances that damage blood vessel linings. This makes arteries narrow and stiff, raising CHD risk.
People with more visceral fat face higher risks of insulin resistance and type 2 diabetes. These conditions increase CHD risk. So, losing weight is key to heart health.
Waist size is a good way to check CHD risk. A bigger waist means more visceral fat, which is bad for the heart. Studies show waist size is a better CHD risk indicator than BMI.
| Waist Circumference | CHD Risk Level | |
| < 31.5 inches (Men) | < 30.5 inches (Women) | Low |
| 31.5 – 37 inches (Men) | 30.5 – 35 inches (Women) | Moderate |
| > 37 inches (Men) | > 35 inches (Women) | High |
Keeping a healthy weight is vital for artery health. Changing diet, exercising more, and making lifestyle changes can help. These steps are key to a healthy weight.
Some good strategies include:
By using these methods, people can control their weight and improve heart health.
Regular physical activity is key for healthy arteries and less heart disease risk. A sedentary lifestyle harms heart health. We’ll look at how lack of exercise affects arteries and how to fight it.
Exercise is vital for heart health. The American Heart Association says you need 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity weekly. Adding muscle-strengthening activities two or more times a week boosts heart protection.
Beginners should start with short, easy workouts and slowly increase them. Even a little exercise helps lower heart disease risk.
Exercise makes arteries more flexible, which is good for blood flow and pressure. It releases nitric oxide, which relaxes blood vessels. This makes them more elastic.
Exercise also cuts down inflammation and improves cholesterol levels. These changes help arteries stay healthy and reduce heart strain.
Adding more activity to your day is easy. Try taking the stairs, walking to work, or doing chores. Also, plan time for exercise, like a lunchtime walk or evening bike ride.
| Activity | Duration | Frequency |
| Brisk Walking | 30 minutes | 5 days a week |
| Cycling | 45 minutes | 3 days a week |
| Swimming | 30 minutes | 2 days a week |
By making these changes and focusing on exercise, you can lower heart disease risk and keep arteries healthy.
What we eat is key to keeping our hearts healthy and preventing atherosclerosis. The foods we choose can either speed up or slow down artery narrowing. Looking into how diet affects coronary heart disease shows that some foods can greatly impact our heart health.
Trans fats in processed and fried foods raise “bad” cholesterol and lower “good” cholesterol. They can cause plaque buildup in arteries, speeding up atherosclerosis. It’s important to eat more natural, unprocessed foods to avoid these harmful fats.
“The American Heart Association suggests eating no more than 5-6% of total daily calories as saturated fat,” says health guidelines. They also advise to keep trans fat intake as low as possible. This highlights the need to watch what fats we eat.
Too much sodium can lead to high blood pressure, a big risk for CHD. High sugar and refined carb intake can cause insulin resistance and diabetes, raising heart disease risk. Lowering these substances is key to protecting our hearts.
Eating a heart-healthy diet is vital for preventing CHD. Diets rich in fruits, veggies, whole grains, and lean proteins help fight heart disease. The Mediterranean diet, focusing on these foods, offers many heart benefits.
Foods high in omega-3s, like salmon and walnuts, also support heart health. They reduce inflammation and improve blood fats. A balanced diet, along with exercise and healthy lifestyle choices, is essential for preventing CHD.
Chronic stress is a big problem in today’s world, affecting millions. It harms our heart health, leading to coronary heart disease (CHD). We’ll look at how stress affects our arteries, find out what causes it, and talk about ways to manage it.
Chronic stress sets off a chain of body responses that can damage blood vessels. Stress hormones like cortisol and adrenaline make our heart beat faster and blood pressure go up. This can cause long-term damage to our arteries.
The endothelium, a thin layer of cells in our blood vessels, is very important. Damage to it can lead to problems with blood flow and increase inflammation. This can narrow our arteries and raise the risk of CHD.
There are many things that can cause chronic stress, like work pressure, money worries, and personal issues. Knowing what stresses us helps us find ways to deal with it. Common stressors include:
Knowing what stresses us is the first step to managing it.
It’s important to manage chronic stress to keep our heart healthy. There are proven ways to do this:
Using these methods can help protect our arteries from stress damage.
Genetic factors and family history play a big role in CHD risk. Coronary heart disease is a complex condition. It comes from genetics and environment working together.
Genetic predisposition can increase the chance of getting CHD. Knowing about genetic factors and family history helps us understand risk better. This way, we can take steps to prevent it.
Research has found genetic markers linked to atherosclerosis, a key part of CHD. These markers are in genes related to lipid metabolism, inflammation, and vascular function.
For example, genetic changes in the LDL receptor can cause familial hypercholesterolemia. This is a condition with very high LDL cholesterol levels. Table 1 lists some important genetic markers for atherosclerosis.
| Genetic Marker | Associated Risk | Mechanism |
| LDLR variants | Familial hypercholesterolemia | Impaired LDL clearance |
| APOE variants | Altered lipid metabolism | Influences LDL and HDL levels |
| CXCL12 variants | Increased atherosclerotic plaque formation | Enhances inflammatory cell recruitment |
Looking at family history is key in CHD risk evaluation. A detailed family history can show who is at higher risk due to genetics.
Healthcare providers should use tools to gather family history. They should focus on first-degree relatives who had heart events early in life.
Preventive steps are vital for those at risk of CHD due to genetics. These include eating heart-healthy, exercising regularly, and quitting smoking.
In some cases, medicine may be needed to control risk factors like high cholesterol or high blood pressure. Early intervention can greatly lower CHD risk in those genetically predisposed.
Understanding genetics and family history helps us give personalized care. This care addresses each person’s unique needs. It helps reduce CHD risk.
It’s important to know who gets coronary heart disease to help more people. We look at who is most at risk and why. This helps us make better health plans.
Coronary heart disease is a big killer worldwide. It causes over 7 million deaths each year. In the U.S., someone dies from it every minute. It’s the cause of one in four deaths.
Global CHD Statistics:
| Region | CHD Mortality Rate |
| Global | 12.7% of total deaths |
| U.S. | 1 in 4 deaths |
| Europe | 20% higher than global average |
Who gets CHD changes with age and gender. Men over 45 and women over 55 face higher risks. Men are more likely to get it, but the gap closes with age. Some ethnic groups are more at risk due to their genes.
Demographic Variations in CHD Risk:
Having many risk factors makes CHD more likely. High cholesterol, high blood pressure, smoking, and diabetes all play a part. Knowing how these add up helps us prevent CHD better.
Cumulative Risk Factors for CHD:
| Number of Risk Factors | Relative Risk of CHD |
| 0-1 | Low |
| 2-3 | Moderate |
| 4 or more | High |
Preventing coronary heart disease (CHD) needs a mix of strategies. We must tackle the different risk factors and causes. This way, we can create effective prevention plans that include lifestyle changes, managing risk factors, and medical help when needed.
Our study shows how key it is to control high blood pressure and keep cholesterol levels right. A healthy lifestyle, like regular exercise, a balanced diet, and managing stress, can greatly lower CHD risk.
Preventing CHD well means looking at all risk factors, like high blood pressure, high cholesterol, and diabetes. Working with doctors and being proactive about heart health can help lower CHD rates. This approach boosts overall health.
By using these strategies every day, people can fight against artery narrowing and lower CHD risk. It’s vital to have a detailed prevention plan. This plan should cover lifestyle, genetics, and environmental factors that lead to CHD.
Atherosclerosis is when plaque builds up in arteries, narrowing them. This blocks blood flow to organs like the heart. It makes the heart work harder, leading to strain.
Risk factors for CHD include high cholesterol, high blood pressure, and smoking. Diabetes, obesity, lack of exercise, and poor diet also play a role. Stress and genetics can increase risk too.
High LDL (“bad”) cholesterol can cause plaque in arteries. This narrows them and limits blood flow to the heart. It raises the risk of CHD.
High blood pressure damages arteries by causing inflammation and scarring. This makes them more likely to narrow or block, increasing CHD risk.
Smoking harms the heart and blood vessels. It speeds up atherosclerosis and damages blood vessel linings. It also reduces blood flow to the heart, raising CHD risk.
Diabetes can damage blood vessels and nerves. It can also cause blood sugar swings that harm the heart. Poorly managed diabetes increases CHD risk.
Obesity, mainly around the belly, raises CHD risk. It promotes inflammation and insulin resistance. These changes damage the heart and blood vessels.
Exercise improves artery flexibility and lowers blood pressure. It also enhances lipid profiles and boosts heart health. Regular activity helps prevent CHD.
Foods high in saturated fats, trans fats, sodium, and refined carbs increase CHD risk. Eating fruits, veggies, whole grains, and lean proteins can protect against CHD.
Yes, chronic stress can harm the heart by causing high blood pressure and inflammation. It damages the vascular system.
Genetics can affect lipid metabolism and blood pressure. They can increase CHD risk. Knowing your family history is important for prevention.
CHD risk varies worldwide and among different groups. Age, gender, ethnicity, and risk factors like smoking and high blood pressure play a role.
Knowing the causes of CHD is key to prevention and management. It helps individuals address risk factors and lower their chance of getting the disease.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!