Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 1 in every 285 children with cancer get radiation therapy as part of their treatment. It’s understandable that parents have significant concerns regarding the safety of this treatment. It’s key to talk about it.Understand the safety protocols used to protect children during treatment and get A sentence for radiation to explain it simply to others.
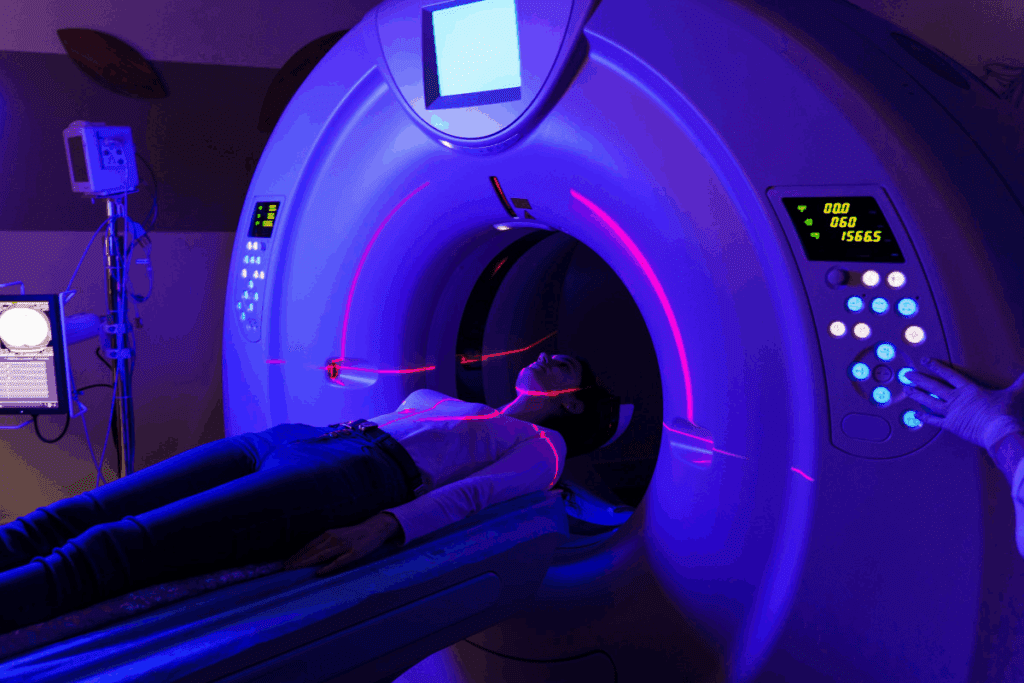
Radiation therapy kills cancer cells with high-energy radiation. It’s a good treatment, but safety worries are real, more so for kids. Our team in pediatric radiation oncology works hard to give the best care to our young patients.
Key Takeaways
- Radiation therapy is used to treat various types of cancer in children.
- The safety of radiation therapy for kids is a significant concern for parents.
- Pediatric radiation oncology requires specialized care and expertise.
- Advanced technology has improved the safety and efficacy of radiation therapy.
- We provide complete support for international patients seeking treatment for their children.
Understanding Radiation Therapy in Pediatric Care
For parents of kids with cancer, knowing about radiation therapy is key. We aim to offer clear support during tough times.
What Is Radiation Therapy?
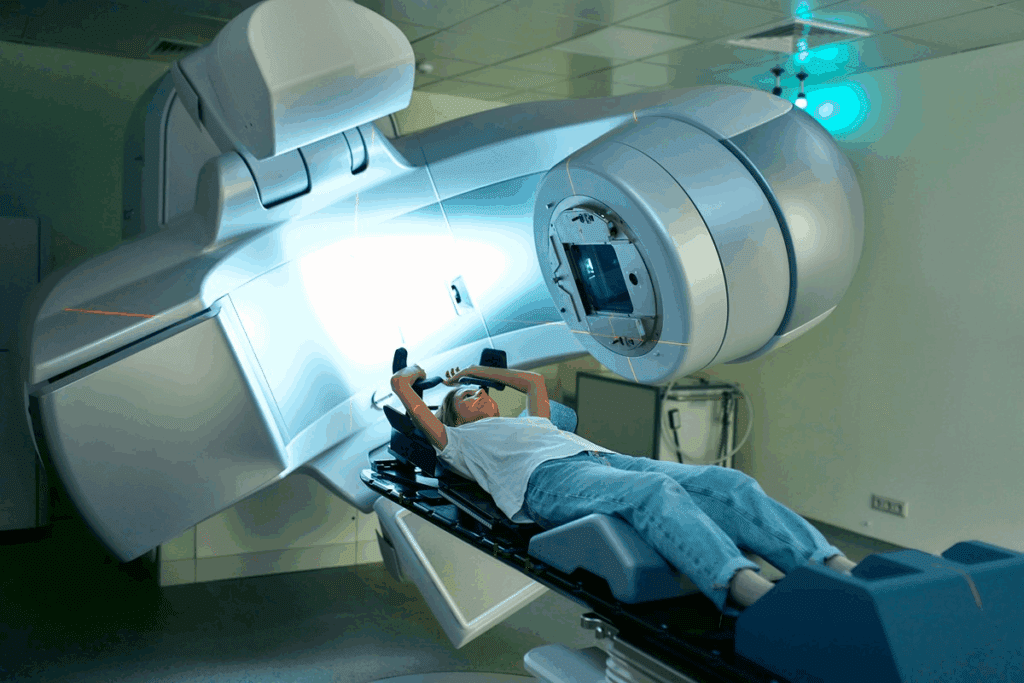
Radiation therapy uses high-energy particles or waves to kill cancer cells. It focuses on the area with cancer.
Radiation therapy can be external or internal. External therapy uses a machine outside the body. Internal therapy puts radioactive material inside or near the tumor.
How Does Radiation Therapy Work?
Radiation therapy damages cancer cells’ DNA, stopping them from growing. Over time, these cells die, and the tumor shrinks.
The aim is to hit the tumor with the right amount of radiation. This way, it doesn’t harm nearby healthy tissues. Thanks to new tech, radiation therapy is now safer and more precise.
Types of Radiation Used in Treatment
Therapy uses gamma rays, X-rays, and electron beams. Gamma rays come from radioactive materials and are used in some internal treatments.
The type of radiation depends on the cancer type, location, and the child’s health. Our team helps families choose the best treatment plan.
The Role of Radiation Therapy in Treating Childhood Cancer
Radiation therapy is key in fighting childhood cancer. It aims to kill cancer cells, boosting survival chances and improving life quality for kids.
Common Childhood Cancers Treated with Radiation
It’s often used for brain and spinal cord tumors in kids. It also works well against neuroblastoma, Wilms tumor, and some leukemias. The choice to use it depends on the cancer type, stage, and the child’s health.
We often pair it with chemotherapy for better results. This makes radiation therapy a vital part of treating kids with cancer.
When Is Radiation Therapy Recommended?
It’s recommended when cancer is in one place and can be hit without harming nearby healthy tissues. It’s also considered when surgery is not an option or would cause too much harm.
Our team decides the best treatment plan for each child. We look at their age, cancer type and stage, and any past treatments.
Success Rates in Pediatric Patients
The success of radiation therapy in kids depends on the cancer type and stage. It’s very effective for some childhood cancers.
| Type of Cancer | Success Rate with Radiation Therapy |
| Brain Tumors | 70-80% |
| Neuroblastoma | 50-70% |
| Wilms Tumor | 80-90% |
These numbers show how important radiation therapy is for kids with cancer. We keep working to make treatments even better for our young patients.
Safety Considerations for Radiation Therapy
Radiation therapy for kids is a careful balance between being effective and safe. We make sure kids are safe by planning carefully and following strict rules.
Guidelines for Safe Radiation Exposure
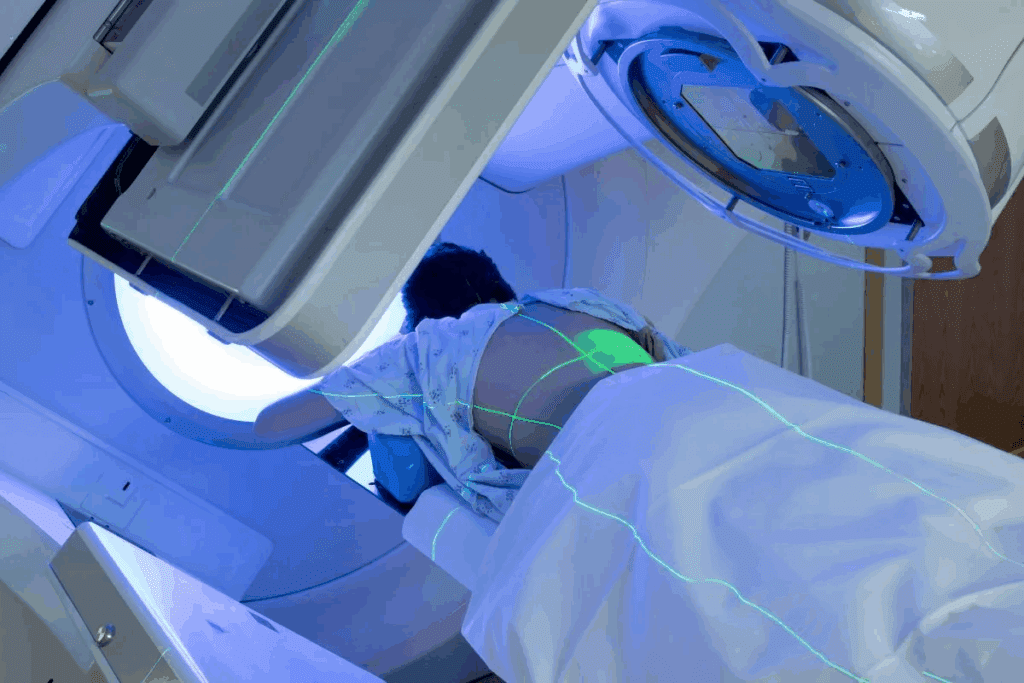
We follow strict guidelines to keep radiation exposure low. This means we target the tumor precisely and avoid healthy tissues. Advanced radiation therapy techniques like IMRT and proton therapy help a lot.
We also think about the child’s age and size. These things can affect how they react to radiation. So, we create personalized treatment plans for each child.
| Radiation Therapy Technique | Description | Benefits for Pediatric Patients |
| Intensity-Modulated Radiation Therapy (IMRT) | Delivers precise doses of radiation to the tumor site | Minimizes exposure to surrounding healthy tissues |
| Proton Therapy | Uses protons instead of X-rays to kill cancer cells | Reduces risk of secondary cancers and damage to critical structures |
Risks and Side Effects for Children
Radiation therapy can cause side effects in kids, like tiredness, nausea, and skin issues. We help families manage these side effects well.
- Fatigue: Rest and relaxation are encouraged.
- Nausea: Medications are available to control nausea.
- Skin Reactions: Gentle skin care practices are recommended.
Long-Term Health Effects
Children may face growth problems and a higher risk of secondary cancers after radiation therapy. We keep a close eye on them to catch any issues early.
Our research helps us improve how we care for kids with radiation therapy. This way, we can make their treatment better and safer.
Comparing Radiation Therapy with Other Treatments
Childhood cancer treatment options include radiation therapy, chemotherapy, and targeted therapy. It’s important to know the differences and benefits of each. This helps decide the best treatment for a child.
Chemotherapy vs. Radiation Therapy
Chemotherapy and radiation therapy are key cancer treatments. Chemotherapy uses drugs to fight cancer cells all over the body. Radiation therapy, on the other hand, targets cancer cells in a specific area with high-energy rays.
The choice between these treatments depends on the cancer type, stage, and the child’s health. Sometimes, both treatments are used together for better results.
Targeted Therapy and Its Applications
Targeted therapy is a newer cancer treatment. It uses drugs to target specific cancer cell traits, sparing healthy cells. This method is effective for some childhood cancers.
Targeted therapy can be used alone or with other treatments like chemotherapy or radiation. The choice depends on the cancer’s genetic makeup.
Combined Treatment Approaches
Using different treatments together, like radiation, chemotherapy, and targeted therapy, is common in childhood cancer care. Combined treatment approaches can improve survival rates and lower recurrence risks.
We work with a team to find the best treatment plan for each child. We consider the cancer type, stage, age, and overall health.
It’s understandable that parents have significant concerns regarding the safety of this treatment.
Communicating Options to Parents
We talk to parents about many things, like the type of radiation and treatment schedule. We also discuss possible side effects and other treatment options. This open dialogue makes parents more confident in their choices for their child.
- Detailed explanations of the treatment process
- Discussion of possible risks and benefits
- Info on other treatment choices
- Support resources for families during treatment
Supporting Children During Treatment
Helping kids during radiation therapy is more than just the treatment. It’s about giving emotional support and addressing their worries. Our team works together to make a supportive space for the whole family.
By teaming up with families, we aim to reduce stress and anxiety from radiation therapy. Our goal is to make the treatment as easy as possible. This way, we help our young patients get the best results.
Innovations in Radiation Technology for Pediatrics
New advancements in radiation therapy offer hope to children with cancer. The field of pediatric oncology is making big strides. These advancements make treatments more precise and safer.
Advances in Radiation Delivery Methods
New methods for delivering radiation are being developed. Proton therapy is a standout for treating some pediatric cancers. It targets tumors more accurately, protecting healthy tissues.
Intensity-Modulated Radiation Therapy (IMRT) is another big leap. It allows for beams of different intensities from various angles. This method helps focus the radiation on the tumor, saving more healthy tissue.
Minimizing Exposure with New Technologies
New tech aims to cut down on radiation for kids. Image-guided radiation therapy (IGRT) is a key innovation. It uses real-time imaging to ensure radiation is delivered exactly right. This cuts down on damage to healthy tissues.
- Advanced imaging techniques improve tumor targeting.
- Real-time monitoring during treatment enhances precision.
- Reduced radiation exposure minimizes long-term side effects.
Ongoing Research and Future Directions
Research in pediatric radiation oncology is ongoing. It aims to better treatment outcomes. Studies are looking into stereotactic body radiation therapy (SBRT) and total body irradiation (TBI) for kids. They’re also studying tumor genetics and molecular traits for more tailored treatments.
- Investigating novel radiation delivery techniques.
- Enhancing patient-specific treatment planning.
- Improving long-term survival rates and quality of life.
As we keep improving radiation therapy, the future looks brighter for kids with cancer. Our goal is to give the best care to our young patients. We’re committed to advancing pediatric radiation oncology.
Psychological Support for Pediatric Patients
The journey through radiation therapy can be tough for kids. We know their emotional health is as vital as their physical health. So, we focus on their mental well-being.
Addressing Emotional Needs
Children facing radiation therapy often feel scared and unsure. We create a supportive space with counseling and emotional support. It’s tailored to their age and understanding.
We work with families to meet each child’s emotional needs. This might mean preparing them for therapy, helping with side effects, or keeping communication open.
Support Resources for Families
Radiation therapy impacts the whole family, not just the child. We offer many resources to help:
- Counseling services for kids and their families
- Support groups for sharing experiences and connecting with others
- Materials to help families understand the treatment and support their child
Our goal is to build a strong support system for families during this tough time.
Coping Strategies During Treatment
It’s key to find ways to cope with the stress of radiation therapy. We help kids and their families find strategies to manage anxiety.
| Coping Strategy | Description | Benefits |
| Relaxation Techniques | Methods like deep breathing, visualization, and progressive muscle relaxation | Reduces anxiety, promotes relaxation |
| Support Networks | Connecting with family, friends, and support groups | Enhances emotional support, reduces feelings of isolation |
| Education and Preparation | Understanding the treatment process and what to expect | Reduces fear, increases sense of control |
By using these strategies, kids and their families can face radiation therapy better. It makes the process less scary.
We’re dedicated to top-notch healthcare for kids with radiation therapy. We focus on their emotional needs and support their families. Our goal is to make their treatment journey as easy as possible.
Regulatory Oversight and Safety Standards
Keeping children safe during radiation therapy is our main goal. We follow strict rules and guidelines to protect them. This complex framework helps keep our young patients safe.
Agencies Involved in Radiation Safety
Several agencies watch over radiation safety in kids. The Nuclear Regulatory Commission (NRC) sets rules for safe radiation use. The International Commission on Radiological Protection (ICRP) gives guidelines for protection. The American Society for Radiation Oncology (ASTRO) also helps set best practices.
Standard Protocols for Pediatric Care
We have strict protocols for kids getting radiation therapy. These include careful planning and precise radiation delivery. We also monitor the patient closely and adjust doses based on age and size.
Using new technologies like IMRT and proton therapy helps us target tumors better. We make sure our equipment works right and our methods are current. This ensures the best care for our patients.
Accreditations and Certifications
Accreditations and certifications show we meet high standards. The Joint Commission and the American College of Radiology (ACR) offer these. They prove our dedication to top-notch care.
| Accrediting Body | Focus Area | Benefits |
| Overall Quality and Safety | Enhanced patient trust, improved care standards | |
| American College of Radiology (ACR) | Radiation Oncology Practices | Verified expertise, adherence to best practices |
| Nuclear Regulatory Commission (NRC) | Safe Use of Radioactive Materials | Compliance with federal regulations, safety assurance |
By following these rules and standards, we give our pediatric patients the best care. We reduce risks and make treatments more effective.
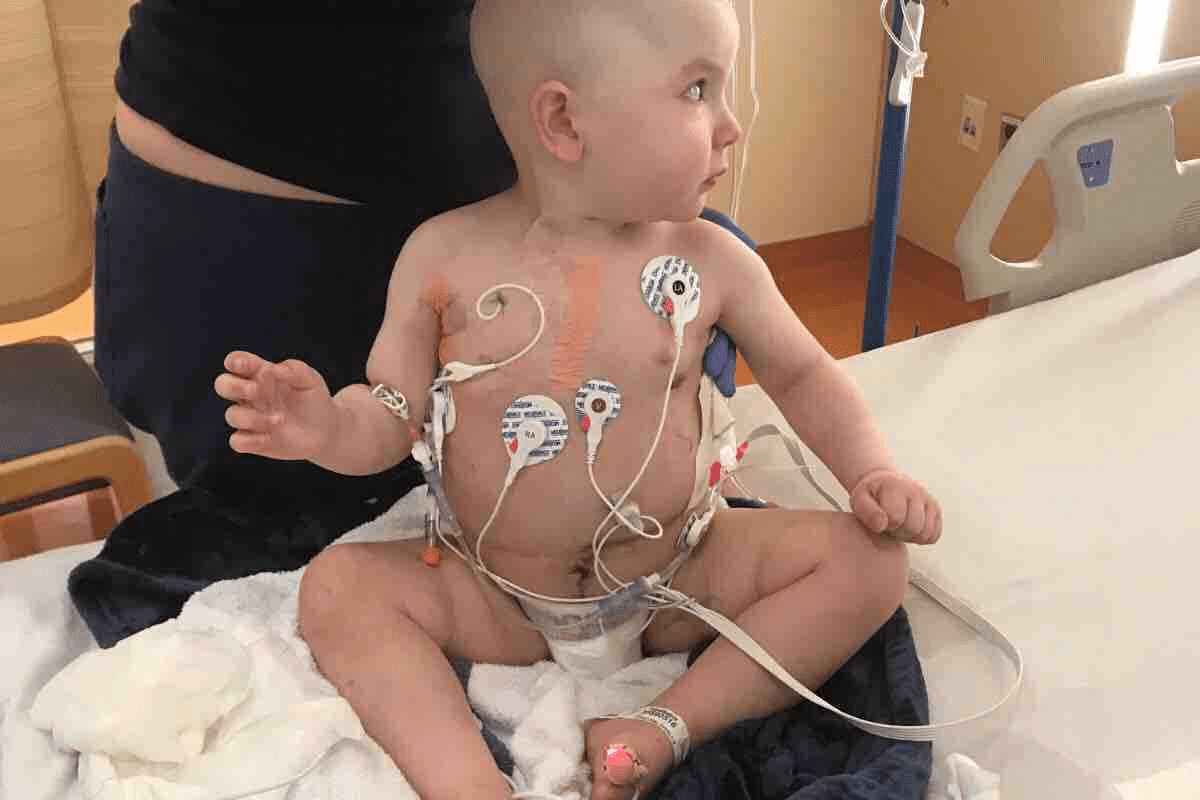
Real-Life Experiences: Stories from Families
Families who have gone through radiation therapy for their kids share valuable insights. They talk about the tough times, the victories, and what they learned. These stories help others who are on the same journey.
Success Stories
Many families have found that radiation therapy worked well for their children. For example, a young girl with a brain tumor was treated with radiation. Now, she’s doing great and loves to stay active.
These stories show how far radiation therapy has come. They also highlight the hard work of doctors and the need for early treatment.
The Challenges Families Face
Even though radiation therapy can be very effective, families face big challenges. They deal with the shock of the diagnosis and the side effects of treatment. It’s tough both physically and emotionally.
It’s important to have support from doctors, family, and friends. Many families find comfort in talking to others who understand what they’re going through. This creates a community of support and understanding.
Overcoming Fears and Embracing Hope
One big challenge is overcoming fears about radiation therapy. Talking openly with doctors and learning about the treatment helps a lot.
By sharing their stories, families who have been through radiation therapy give hope to others. Their experiences show that treatment can work and that kids and families can be strong.
We know that every child’s journey with radiation therapy is different. But by learning from others, families can find their way. They can do it with knowledge, support, and hope.
FAQs About Radiation Therapy for Kids
Radiation therapy is a common treatment for childhood cancers. Parents often have many questions about its safety and how well it works. We know it can be hard to understand, but knowing more can help you feel better.
Common Questions from Parents
Parents worry about the effects of radiation therapy on their child. They ask, “Will it hurt my child?” and “Are there long-term side effects?”
- How is radiation therapy administered?
- What are the possible risks and side effects?
- How can we support our child during treatment?
Expert Answers to Parental Concerns
Our team is here to help and support you. Radiation therapy is a precise treatment that targets cancer cells while minimizing exposure to surrounding healthy tissues. We use the latest technology to make treatment as effective as possible with fewer side effects.
Concerns about pain are common. Radiation therapy itself is not painful, but some children might feel tired or have skin irritation. We work with families to manage these side effects and offer the support they need.
Resources for More Information
For more information, there are trusted resources available. The American Cancer Society and the Children’s Oncology Group offer valuable information on radiation therapy and childhood cancer treatment.
- American Cancer Society:
- Children’s Oncology Group:
We encourage parents to contact these organizations and our team for any questions or concerns about radiation therapy for their child.
Conclusion: Weighing the Risks and Benefits
Radiation therapy is a complex treatment that needs careful thought, mainly in pediatric care. It’s important to understand its role in treating childhood cancer. This knowledge helps in making informed decisions.
Careful Consideration of Treatment Options
A team of specialists is key in pediatric radiation oncology. They work together to create a treatment plan that fits the child’s needs. This team approach helps parents understand the risks and benefits of radiation therapy. It allows them to make choices that are best for their child.
Informed Decision-Making
Parents must be well-informed when it comes to radiation therapy for kids. Knowing the treatment options and possible outcomes helps them work with their child’s healthcare team. A team of experts from different fields is essential in pediatric radiation oncology. They provide the best care for children.
FAQ
What is radiation therapy, and how does it work?
Radiation therapy is a treatment for cancer. It uses high-energy rays to kill or slow cancer cells. We use different types like gamma rays or X-rays to target tumors safely.
Is radiation therapy safe for children?
We are very careful with our young patients. Radiation therapy has some risks, but we follow strict rules to keep them low. Our team works with families to create a safe treatment plan.
What are the possible side effects of radiation therapy in children?
Side effects can vary. They might include feeling tired, skin changes, or hair loss. We also watch for long-term effects and try to prevent them.
How does radiation therapy compare to other cancer treatments?
We often use radiation therapy with other treatments like chemotherapy. Each treatment has its own benefits and risks. We help families choose the best option for their child.
Can children undergoing radiation therapy be around other kids and family members?
Usually, yes. But we give specific advice on how to keep others safe. We also offer support to help families deal with treatment’s emotional side.
How long does radiation therapy take to shrink a tumor?
It depends on the cancer type, tumor size, and radiation dose. We closely watch progress and adjust the treatment as needed.
What is the role of parental involvement in radiation therapy for children?
We believe parents should be involved. We explain treatment options and address concerns. We also offer emotional support during treatment.
Are there any new developments in radiation therapy for pediatric care?
Yes, we stay updated on new technology and treatments. Research and innovations are improving outcomes and reducing side effects for kids.
How can families cope with the emotional challenges of radiation therapy?
We offer counseling and support groups. We also provide tips on managing stress and anxiety. This helps families cope emotionally.
What regulatory oversight is in place for radiation therapy in children?
Radiation therapy is closely watched to ensure safety and effectiveness. We follow strict guidelines and protocols for pediatric care. This ensures our young patients get the best care.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32838088/