Chronic back pain can really get in the way of life. If you’ve tried many treatments but nothing works, nerve ablation might be the answer. It’s a small procedure that uses radiofrequency to turn off the pain nerves, giving you long-lasting relief.
At Liv Hospital, we know how tough chronic pain can be. We’re dedicated to finding new ways to help. Our team uses the latest tech to make sure ablation nerve procedures are safe and work well. This helps our patients get back to living their best lives.
It’s important to understand chronic back pain to find good treatments. This pain affects many people worldwide, causing a lot of disability and lowering their quality of life.
Chronic back pain comes from many sources. It can be from degenerative conditions, injuries, or lifestyle choices. Facet-mediated pain is a common cause. It happens when the facet joints in the spine get arthritic.
Common Causes Include:
Treating chronic back pain starts with simple steps. It moves to more complex treatments if needed.
| Treatment Stage | Interventions |
| Conservative Management | Physical therapy, medication, lifestyle modifications |
| Minimally Invasive Procedures | Nerve blocks, steroid injections |
| Advanced Interventions | Nerve ablation, spinal cord stimulation |
Knowing the causes and treatments helps doctors tailor care for each patient. This can lead to better pain management and a better life for those suffering from chronic back pain.

Ablation nerve treatment is a big step forward in treating chronic back pain. It’s a less invasive option compared to traditional surgeries. We’ll dive into what it is, how it works, and the different methods used.
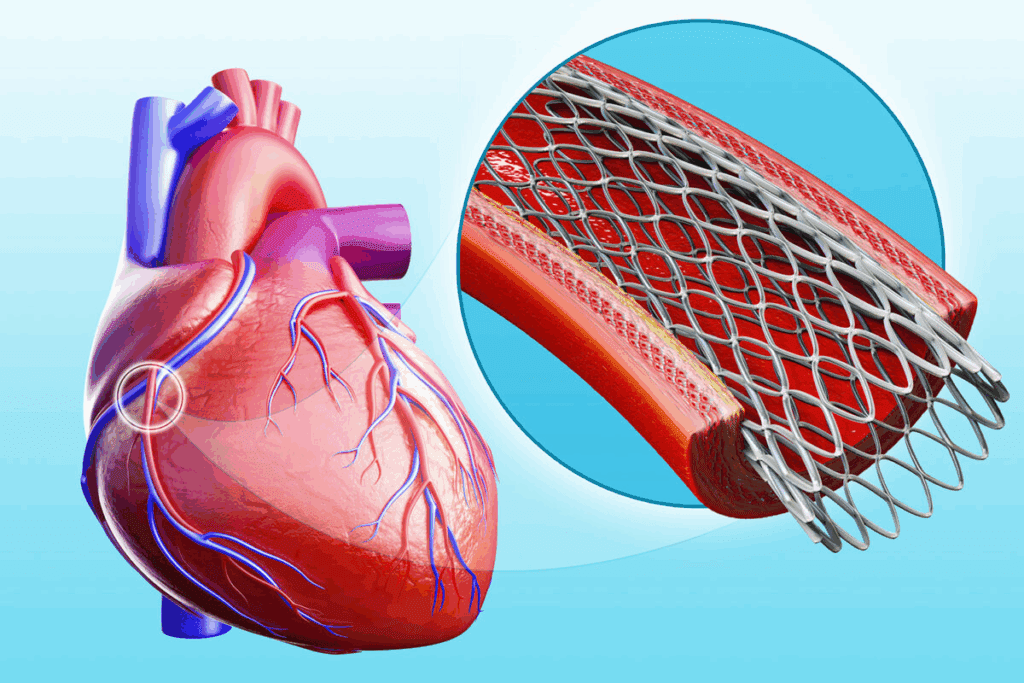
Ablation nerve treatment, or nerve ablation, is a minimally invasive procedure for chronic back pain. It uses thermal energy or other methods to stop specific nerves from sending pain signals to the brain. Studies show that basivertebral nerve ablation is a non-surgical, minimally invasive treatment for lower back pain.
The main idea behind nerve ablation is to interrupt the pain signal before it hits the brain. This reduces or stops the pain feeling. It does this by targeting the nerves that carry pain signals from the affected area.
There are several nerve ablation techniques, each with its own way of working:
Each method is chosen based on the patient’s condition and the type of pain they have.
Nerve ablation uses thermal energy to block pain signals. It’s a promising method for those with severe back pain. Radiofrequency ablation (RFA) is a key technique for managing chronic pain.
Thermal energy is heat used to damage nerve tissue. This stops pain signals from reaching the brain. When nerves are heated, they can’t send signals anymore, reducing pain.
A special device with radiofrequency waves is used. It heats the area around the needle tip, placed near the nerve. This heat damages the nerve, cutting off pain signals.
Nerve ablation and nerve cutting aim to stop pain signals. But they work in different ways.
Nerve ablation uses heat to harm the nerve. Nerve cutting, on the other hand, cuts the nerve surgically. Here’s a comparison:
| Characteristics | Nerve Ablation | Nerve Cutting |
| Method | Uses thermal energy to damage nerve tissue | Surgically severs the nerve |
| Invasiveness | Minimally invasive | More invasive, requires surgery |
| Reversibility | Effects can be considered somewhat reversible as nerve regeneration is possible | Generally considered irreversible |
| Recovery Time | Typically shorter recovery time | Longer recovery time due to surgical nature |
Knowing these differences helps patients and doctors choose the best treatment for back pain.
If you have back pain that won’t go away, nerve ablation might be an option. It’s a procedure that could help you find long-term relief from chronic back pain.
Nerve ablation works well for specific back pain types. Studies show it’s great for facet-mediated axial back pain in the neck and lower back. It’s recommended when other treatments haven’t helped.
Common Back Conditions Treated with Nerve Ablation:
These pains are usually in the back and get worse with movement. Nerve ablation can stop these pain signals from reaching your brain.
Not everyone with back pain is a good candidate for nerve ablation. We check each patient carefully to see if they’re a good fit for the procedure.
| Criteria | Description |
| Failure of Conservative Therapy | Patients who haven’t gotten better with treatments like physical therapy, medicine, or injections. |
| Diagnostic Confirmation | Positive diagnosis of facet-mediated pain through tests or diagnostic blocks. |
| Absence of Contraindications | Patients without conditions that could make the procedure risky, like bleeding disorders or infections. |
By choosing patients carefully, we can make sure nerve ablation works best. This helps those with chronic back pain find significant relief.
Before radiofrequency ablation, a nerve block test is key. It checks if the treatment will work for chronic back pain. This test finds out if the pain comes from the right area and if the treatment will help.
Diagnostic nerve blocks involve injecting a local anesthetic into or around nerves. The goal is to see if these nerves cause pain. By numbing the area, doctors can see if pain goes away.
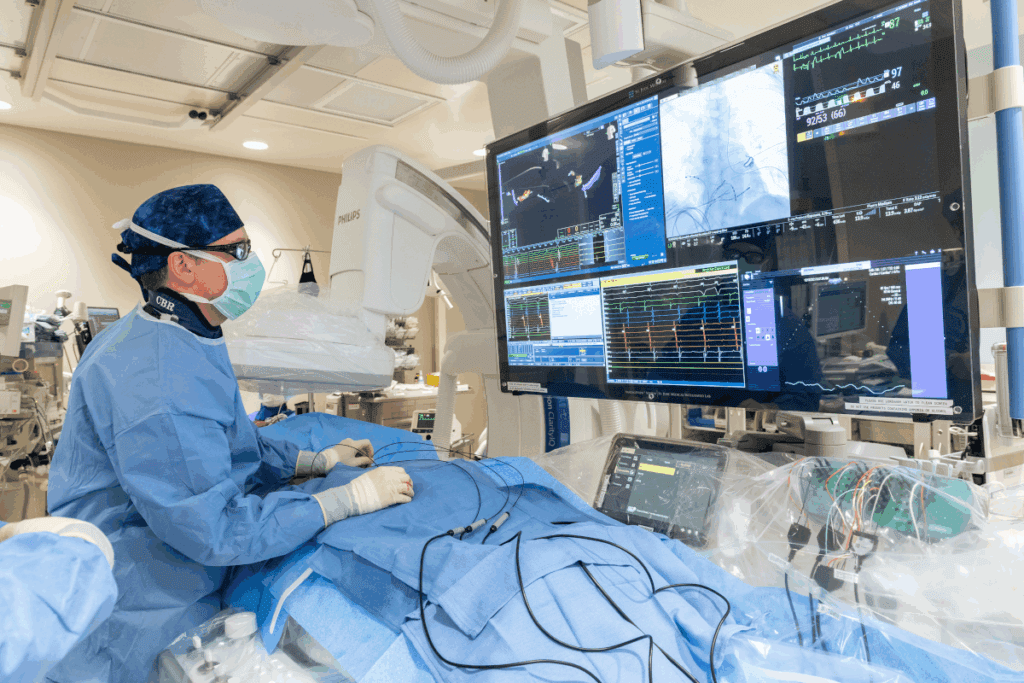
The test is done with imaging like fluoroscopy to place the anesthetic right. This is important for good results. Patients are watched after the injection to see how they feel.
When looking at nerve block test results, doctors check how much pain relief there is. If pain goes down a lot, it means the nerves are likely causing the pain. This shows radiofrequency ablation might work well.
If there’s little to no pain relief, it might mean the nerves aren’t the main problem. Or, other things could be causing the pain. Then, more tests might be needed to find the real cause or to look at other treatments.
Experts say using diagnostic blocks before radiofrequency ablation makes treatment better. It makes sure only those likely to get better from the treatment do it. This shows how important it is to do a good diagnostic check before deciding on ablation.
Getting a nerve ablation procedure for back pain is a big step towards feeling better. Knowing what to expect can make you feel more at ease. We make sure our patients know every step of the way.
Before we start, we do a lot of prep work. We look at your medical history to check for any risks. We also do a physical exam to see if the procedure is right for you.
We tell you what to do before the procedure, like avoiding certain medicines. We also talk about what to expect after it’s done to help with your recovery.
| Pre-Procedure Instruction | Purpose |
| Avoid blood thinners | Reduce risk of bleeding |
| Arrange for post-procedure transportation | Ensure safe travel home after the procedure |
| Stop certain medications as advised | Minimize possible interactions or problems |
To keep you comfortable, we use local anesthesia. It numbs the area where the needle goes. We use a small needle and imaging to guide it to the right spot.
This way, you won’t feel any pain during the procedure. We keep an eye on how you’re feeling and adjust the anesthesia if needed.
Getting the needle in the right spot is key for the procedure’s success. We use imaging like fluoroscopy or ultrasound to guide it. This makes sure we hit the target nerve.
Once the needle is in place, we use heat to stop the nerve from sending pain signals. This is how we help you find relief from back pain.
By following these steps, we make sure the procedure is safe and works well. Our goal is to help you feel better from chronic back pain.
The medial branch nerves are key in sending pain signals from the facet joints. Knowing how these nerves work is vital for managing pain through medial branch ablation.
Medial branch nerves branch off from the primary dorsal rami of spinal nerve roots. They help send pain signals from the facet joints. According to StatPearls, these nerves are essential for pain relief.
The anatomy of medial branch nerves varies along the spine. In the cervical area, their branching is specific. In the lumbar area, they follow a different path. Knowing these differences is key for precise ablation.
Facet joint pain often leads to chronic back pain. Medial branch nerves are key in sending this pain. By targeting these nerves, we can reduce facet joint pain.
Studies show medial branch ablation is effective for facet joint pain. Accurate diagnosis and precise targeting are key for success.
| Region | Anatomical Characteristics | Clinical Significance |
| Cervical | Specific branching patterns | Important for precise needle placement |
| Lumbar | Different course of medial branch nerves | Critical for effective ablation |
Understanding medial branch nerves and their link to facet joint pain helps healthcare providers. Medial branch ablation is a valuable treatment for chronic back pain.
Knowing what to expect after nerve ablation helps manage your hopes and gets the best results. We’ll walk you through the key recovery steps. You’ll learn about the immediate effects and when you can get back to normal.
Right after the procedure, you might feel some pain or soreness where the treatment was done. Medical News Today says this usually goes away in a few days. You might feel numbness or weakness in the treated area, but it’s usually temporary.
Some people might see mild swelling or bruising at the injection site. These signs are short-lived and can be eased with over-the-counter pain meds and cold packs.
How long it takes to get back to normal varies. It depends on your health and the procedure details. You should avoid hard work, heavy lifting, and bending for a few days after.
Always listen to your doctor’s advice. They can give you specific guidance based on your situation and procedure.
Understanding the recovery helps you prepare better. It ensures you get the most out of your nerve ablation treatment.
It’s important to know how well nerve ablation works for pain relief. This treatment has become popular for back pain because it can offer lasting relief.
Many studies have looked into nerve ablation for back pain. They found it can be a good treatment for some back pain types. For example, a study showed it helps with chronic back pain.
How well nerve ablation works can vary. But, many people find it helps a lot. It’s key to remember that results can differ based on health and the doctor’s skill.
People often wonder how long nerve ablation’s effects last. Relief can last from 6 months to over 2 years. Some studies say relief can last for years.
Nerve ablation isn’t a permanent fix because nerves can grow back. But, this can take years. During this time, many people see big improvements in their pain and life quality.
In summary, nerve ablation is a hopeful option for chronic back pain. It can offer lasting relief. But, it’s important to talk to a doctor to see if it’s right for you.
It’s important to know the risks and side effects of spinal ablation before deciding on it. This treatment, like any medical procedure, has its own set of risks. Patients need to be aware of these.
Spinal ablation is usually safe but can cause some side effects. These might include pain, swelling, or bruising at the site. Some might feel more pain before they start feeling better.
Most patients do well without major issues after spinal ablation. Knowing about these side effects can help with recovery and expectations.
| Common Side Effects | Frequency | Typical Duration |
| Temporary discomfort | Common | 1-3 days |
| Swelling or bruising | Common | 1-7 days |
| Temporary increase in pain | Less common | Until pain relief is achieved |
Though rare, serious problems can happen with spinal ablation. These include infections, nerve damage, or allergic reactions. It’s key to watch for these after the procedure.
Nerve damage is a serious but rare issue. It can lead to ongoing pain, numbness, or weakness. The risk is lower with careful technique and imaging during the procedure.
In summary, spinal ablation is mostly safe, but knowing the risks and side effects is vital. Being informed helps patients make the best choices for their health.
Looking into other options for back pain is key. Nerve cauterization works for some, but others might find better choices. It’s important to find what works best for each person.
There are many pain procedures that can replace nerve cauterization. Studies, like those in StatPearls, highlight pulsed radiofrequency and cryoablation as good alternatives.
Pulsed radiofrequency sends electrical pulses to nerves without causing much heat. This might offer relief with fewer risks than traditional methods.
Cryoablation uses cold to stop nerves from sending pain signals. It’s a good option for those who can’t have heat treatments.
Many prefer non-invasive treatments first or alongside others. These include:
It’s vital for patients to talk to their healthcare provider about these options. This way, they can choose the best treatment for their situation.
When looking at treatments for chronic back pain, nerve ablation stands out. It’s a minimally invasive method that disrupts pain signals to offer relief. This makes it a good option for many people.
We’ve looked into the details of nerve ablation, including its benefits and risks. Knowing about it helps patients decide if it’s right for them.
Choosing nerve ablation should be a careful decision. It’s best to talk to a healthcare professional first. This way, patients can move closer to lasting relief from back pain.
A nerve ablation procedure is a treatment for back pain. It uses heat or cold to damage nerves. This stops pain signals from reaching the brain, giving relief from chronic back pain.
Nerve ablation and nerve cutting both aim to stop pain signals. But they work differently. Nerve ablation uses heat or cold, while nerve cutting cuts the nerve surgically.
Chronic back pain can come from many sources. Facet joint arthritis, degenerative disc disease, and spinal stenosis are common. Nerve ablation often treats pain from facet joints.
A nerve block test numbs a suspected pain-causing nerve with local anesthetic. If pain goes away, it shows the nerve is the pain source. This makes the patient a good candidate for radiofrequency ablation.
Diagnostic nerve blocks confirm if a nerve is causing pain. They help decide if a patient is right for radiofrequency ablation.
After nerve ablation, you might feel soreness, numbness, or discomfort. Most people can get back to normal in a few days. Always follow your doctor’s post-procedure care instructions.
Pain relief from nerve ablation varies. It can last from 6 months to 2 years or more. Some people get long-lasting relief, while others might need more treatments.
Spinal ablation can cause temporary numbness, soreness, or discomfort. Serious but rare complications include infection, nerve damage, or allergic reactions.
Yes, there are other treatments for back pain. Options include steroid injections, spinal cord stimulation, and non-invasive methods like physical therapy, medication, or lifestyle changes.
Medial branch ablation targets nerves that send pain signals from facet joints. By damaging these nerves, it can help relieve facet-mediated pain.
The procedure uses imaging to guide a needle to the nerve. Local anesthesia numbs the area. Then, the nerve is ablated with heat or cold.
National Center for Biotechnology Information. (2025). What Is a Nerve Ablation for Back Pain. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7901125/
Janapala, R. N., Manchikanti, L., Sanapati, M. R., Thota, S., Abd-Elsayed, A., Kaye, A. D., & Hirsch, J. A. (2021). Efficacy of radiofrequency neurotomy in chronic low back pain: A systematic review and meta-analysis. Pain Medicine, (Published online). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8439627/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us