Last Updated on November 13, 2025 by
Childhood leukemia often shows up with sudden changes in blood counts. These changes are key to catching the disease early, and understanding how is leukemia diagnosed plays an important role. At top places like livhospital.com, we know that odd lab results can mean anemia, thrombocytopenia, or leukocytosis.
When a child’s blood test shows something off, it’s time to see a doctor. The bone marrow makes new blood cells, but in leukemia, it makes bad white blood cells instead. This is how leukemia is diagnosed.
Key Takeaways
- Childhood leukemia is diagnosed through abnormal lab results, mainly in CBC tests.
- Signs like anemia, thrombocytopenia, and leukocytosis can point to leukemia.
- Spotting it early is key to better treatment in kids.
- Seeing the family doctor is usually the first step.
- Blood tests are vital for finding blood cell problems.
Understanding Childhood Leukemia
It’s key to know about childhood leukemia to catch it early and treat it well. This cancer affects the blood and bone marrow. It’s the most common cancer in kids, making up nearly one in three cases.
Types of Childhood Leukemia
Childhood leukemia comes in several types, with Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML) being the most common. ALL makes up about 80% of cases, while AML is around 15-20%. There are also rarer types like Chronic Myeloid Leukemia (CML) and Juvenile Myelomonocytic Leukemia (JMML).
Each leukemia type has its own traits and treatment needs. For example, ALL is often treated with chemotherapy and has a good outlook if caught early. AML, though, needs more intense treatment, like chemotherapy and sometimes a bone marrow transplant.
Prevalence and Risk Factors
Childhood leukemia hits some groups harder and is linked to certain risks. The rate of leukemia varies worldwide, with some countries seeing more cases. Known risks include genetic factors, radiation, and some toxins.
Parents might worry about leukemia risks in their kids. While some risks are unavoidable, knowing the signs can help catch it early. Look out for signs like constant tiredness, pale skin, frequent infections, and easy bruising or bleeding.
Our pediatric oncologists stress the need for early detection and full care. Knowing about childhood leukemia types and how common they are helps parents deal with diagnosis and treatment.
Complete Blood Count Abnormalities
Diagnosing childhood leukemia starts with a Complete Blood Count (CBC) test. This test checks the numbers and types of white blood cells, red blood cells, and platelets. It’s key to spotting leukemia early.
Children with leukemia often show odd CBC results. These can include anemia, low platelets, and unusual white blood cell counts. These signs point to the disease.
Anemia: Low Hemoglobin in 83% of Cases
Anemia is common in kids with leukemia, affecting 83% of them. Low hemoglobin levels cause fatigue, weakness, and shortness of breath. A study found anemia is a big sign of leukemia in kids, needing quick action.
“Anemia is a critical component of the initial presentation of leukemia in children, highlighting the need for prompt diagnosis and treatment.”
Thrombocytopenia: Low Platelets in 80% of Cases
Thrombocytopenia, or low platelets, is seen in 80% of leukemia cases in kids. It raises the risk of bleeding and bruising. Monitoring platelet counts is key to managing the disease.
White Blood Cell Variations: From Leukopenia to Extreme Leukocytosis
White blood cell counts vary in childhood leukemia. Some kids have low counts, while others have high counts, with 46% having extreme highs. These variations affect the immune system and health.
It’s vital to understand these CBC oddities for diagnosing and treating childhood leukemia. Spotting anemia, thrombocytopenia, and white blood cell changes helps doctors start the right treatment.
Pancytopenia: A Critical Warning Sign
Pancytopenia is when all three blood cell types are low. It’s a big warning sign that needs quick medical help. This is very important in kids with leukemia, as it shows a serious problem.
Recognizing Reduction in All Three Cell Lines
Pancytopenia means fewer red, white blood cells, and platelets. This can cause tiredness, more infections, and easy bleeding. Spotting these signs early is key to acting fast.
To find pancytopenia, doctors do a CBC test. This test checks the levels of different blood cells. A big drop in all three types means looking deeper, often finding leukemia.
Clinical Significance and Emergency Management
Pancytopenia is very serious, often linked to childhood leukemia. Quick action is needed, including going to the hospital and getting blood transfusions.
Knowing how to spot leukemia early is vital. Seeing pancytopenia as a warning sign is a big part of this. Quick diagnosis and treatment can greatly help kids with leukemia.
In short, pancytopenia is more than a condition; it’s a serious warning. Understanding its importance and acting quickly can greatly help kids with leukemia.
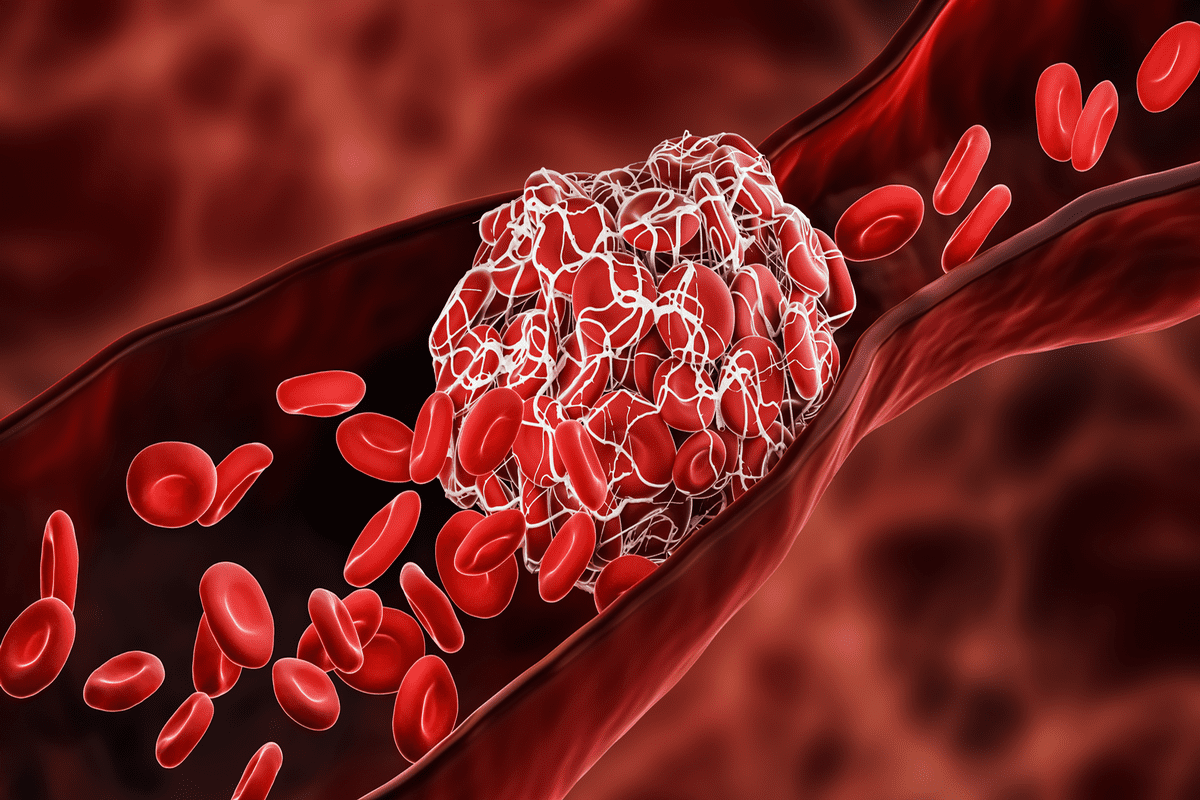
Peripheral Blood Smear Findings
Diagnosing leukemia often involves a key tool: the peripheral blood smear. This test looks at a blood sample under a microscope. It helps find abnormal cells that might show leukemia.
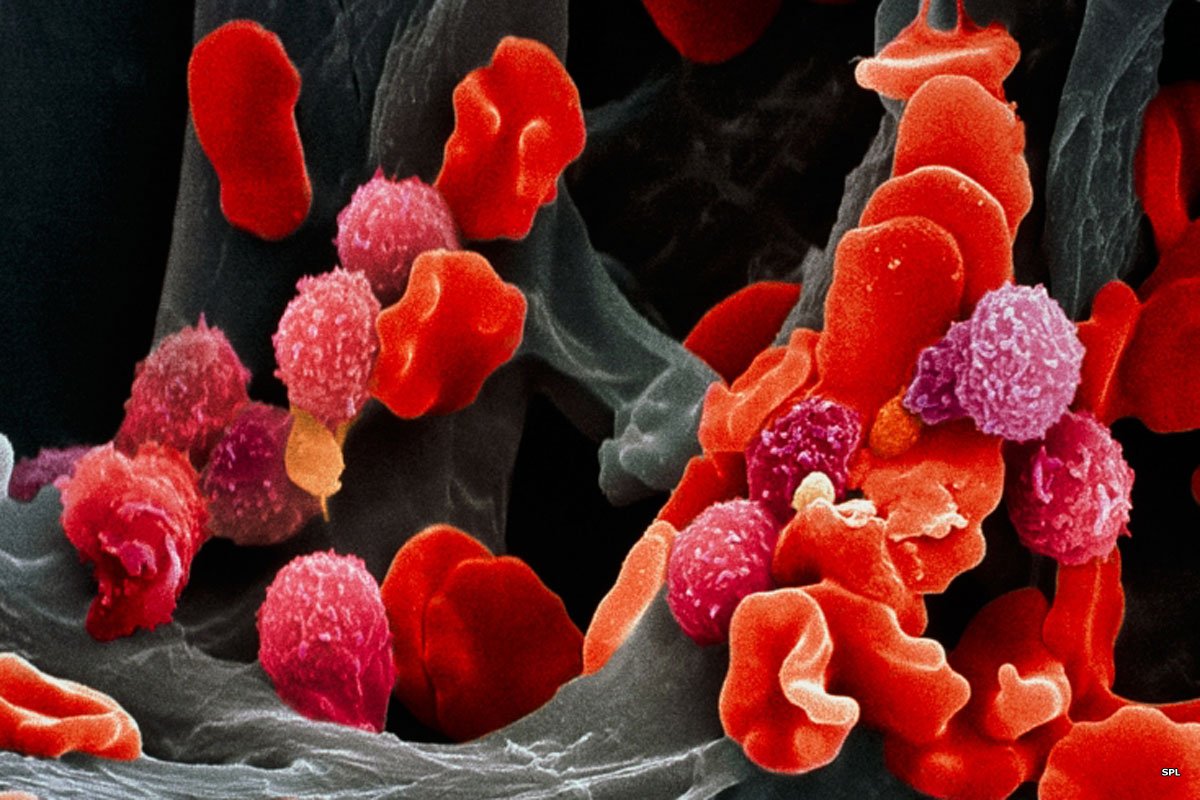
Blast Cells: The Hallmark of Leukemia
Blast cells in the blood smear are a big sign of leukemia. These cells are young and shouldn’t be in healthy blood. Finding them is a key clue, but not all leukemia shows up this way.
Some blast cell features include:
- They are bigger than normal white blood cells
- They have a big nucleus and small cytoplasm
- They have visible nucleoli
Morphological Changes in Blood Cells
Leukemia also changes how blood cells look. These changes can affect red and white blood cells and platelets. For example, red blood cells might look irregular or be different sizes.
Some changes include:
- Red blood cells can vary in size
- They can have different shapes
- White blood cells might have odd granules
These changes in the blood smear can suggest leukemia. But it’s important to remember that the smear is just one part of finding a diagnosis.

Doctors use the blood smear to look for leukemia. They can then start figuring out what to do next. The smear’s findings, along with other tests, help make a correct diagnosis and treatment plan.
How Is Leukemia Diagnosed: The Complete Process
The journey to diagnose leukemia often begins with a routine blood test. This test shows signs of trouble. Then, a series of tests confirms if the disease is present.
Initial Blood Work Suspicion
The first step is a Complete Blood Count (CBC). This test checks the blood’s components, like red and white blood cells, and platelets. If the counts are off, it might mean leukemia.
Abnormal CBC results lead to more tests. Finding blast cells in the blood is a big clue for more tests.
Confirmatory Testing
After a CBC hints at leukemia, more tests are needed. These tests help confirm the diagnosis. They include:
- Peripheral Blood Smear: A close look at blood cells for oddities.
- Immunophenotyping: Identifies the leukemia type by checking cancer cell proteins.
- Cytogenetic Testing: Looks at cell genetics for leukemia signs.
Bone Marrow Aspiration and Biopsy
A bone marrow aspiration and biopsy are key. It takes a bone marrow sample for study. This test shows the leukemia type, how far it’s spread, and cancer cell details.
The diagnostic process may take time. But it’s vital for a correct diagnosis and treatment plan. Knowing the steps helps patients and families understand the journey.
Cytogenetic and Molecular Abnormalities
Diagnosing leukemia has gotten better with the discovery of specific genetic changes. These changes help us understand how the disease grows and find the best treatment.
Common Chromosomal Abnormalities
Cytogenetic testing finds changes in chromosomes, like translocations and aneuploidy, which are common in leukemia. For example, the Philadelphia chromosome is a known abnormality in some leukemias. It happens when chromosomes 9 and 22 swap places. The National Center for Biotechnology Information says these genetic changes are very important for predicting how the disease will progress.
Other changes include having more or fewer than 46 chromosomes in a cell. These can make the leukemia more aggressive or harder to treat.
Prognostic Implications of Genetic Findings
The genetic findings from cytogenetic testing are very important for predicting the disease’s course. Some changes mean a better outlook, while others suggest a higher risk of relapse or treatment failure. Knowing this helps doctors create treatment plans that fit each child’s needs.
We use this knowledge to make treatment choices that are right for each child. This way, we can help improve their chances of a better outcome and lower the risk of complications.
Laboratory Differences Between ALL and AML
It’s important to know the differences between ALL and AML for the right treatment. Lab tests help tell these two leukemias apart. This is key to making a good treatment plan.
Distinguishing Features in Blood Work
Blood tests are the first step in finding leukemia. ALL and AML show different signs in blood tests. ALL has many lymphoblasts, while AML has myeloblasts. The CBC might show anemia or low platelets in both, but the cell types differ.
Some key blood work differences are:
- ALL has lymphoblasts, AML has myeloblasts
- White blood cell counts and differentials vary
- Red blood cell and platelet counts differ
Immunophenotyping Results
Immunophenotyping is a key test for finding the leukemia type. This test is vital for telling ALL and AML apart. ALL cells have lymphoid markers like CD19 and CD10. AML cells have myeloid markers like CD33 and CD13.
Immunophenotyping also shows:
- Leukemia cell maturity
- Specific antigens for ALL or AML
- Prognostic factors based on the test
Cytochemical Staining Patterns
Cytochemical staining helps tell ALL and AML apart, too. This technique highlights enzymes or structures in cells. For example, AML cells often have myeloperoxidase (MPO) enzyme, which is usually not found in ALL cells.
Cytochemical staining patterns give important clues about leukemia cell lineage and differentiation. This helps in diagnosing and classifying leukemia.
In summary, knowing the lab differences between ALL and AML is vital for diagnosis and treatment. Understanding these differences helps doctors create better treatment plans for patients.
Interpreting Lab Results for Parents and Caregivers
As a parent or caregiver, it’s key to understand your child’s lab results. This knowledge helps you make informed decisions about their care. When your child is diagnosed with leukemia, many lab tests are done. These tests help diagnose, plan treatment, and track progress. It can be tough to understand these results, but with help, you can get through it.
Understanding Your Child’s Blood Test Reports
Blood test reports show metrics like white blood cell count, hemoglobin levels, and platelet count. Knowing these metrics is important to understanding your child’s health. For example, an abnormal white blood cell count might mean leukemia. Your child’s oncologist will explain these results in the context of their health.
It’s key to learn about the different parts of a blood test report. This knowledge helps you ask better questions and understand your child’s treatment plan.
Questions to Ask Your Child’s Oncologist
When you get lab results, you might have questions. Don’t be afraid to ask your child’s oncologist for help. Here are some questions to think about:
- What do the lab results say about my child’s current health?
- How do these results affect the treatment plan?
- Are there any big changes in the lab results we should know about?
- What lab results should we expect during and after treatment?
Monitoring Progress Through Lab Values
Lab values are key to tracking your child’s progress during treatment. Regular blood tests let the healthcare team see if treatment is working. Tracking these results helps you understand your child’s journey and meet their needs better.
By working with your child’s oncologist and understanding lab results, you can actively support their care and recovery.
Advanced Diagnostic Techniques
Advanced diagnostic techniques have changed how we diagnose leukemia. They offer precise and personalized treatment options. These new technologies have greatly improved our ability to diagnose and monitor leukemia. This leads to more effective treatments.
Flow Cytometry
Flow cytometry is a key tool in diagnosing leukemia. It analyzes the proteins on leukemia cells’ surfaces. This helps identify the type of leukemia, like ALL or AML. Knowing this is vital for choosing the right treatment.
The process labels cells with fluorescent antibodies. These antibodies bind to specific proteins. Then, the labelled cells go through a flow cytometer. It measures their fluorescence and other traits. This helps spot abnormal cells and understand their characteristics.
Next-Generation Sequencing
Next-generation sequencing (NGS) is a fast way to sequence DNA or RNA. In leukemia diagnosis, genetic mutations that cause the disease. This info helps predict how well a patient will do and guides treatment.
NGS can spot many genetic changes, like mutations and deletions. By looking at leukemia cells’ genes, doctors can find therapy targets. They can also watch for mutations that make treatment less effective.
Minimal Residual Disease Testing
Minimal residual disease (MRD) testing finds small leukemia cells left after treatment. It uses flow cytometry or molecular methods like PCR. MRD testing shows if treatment is working well.
Having MRD means a higher risk of relapse. Without MRD, the outlook is better. MRD testing helps decide if more treatment is needed or if it can be reduced.
In summary, advanced techniques like flow cytometry, next-generation sequencing, and MRD testing have changed leukemia diagnosis and treatment. They give detailed info on leukemia cells. This helps doctors create personalized treatment plans and check how well treatments are working.
- Flow cytometry helps identify specific types of leukemia and their immunophenotypic characteristics.
- Next-generation sequencing detects genetic mutations and alterations driving the disease.
- Minimal residual disease testing monitors the presence of small numbers of leukemia cells after treatment.
Conclusion: From Lab Results to Treatment Planning
Understanding lab results is key in diagnosing and treating childhood leukemia. We’ve talked about different tests like complete blood count and bone marrow aspiration. These help find problems in blood cells.
Healthcare providers use these findings to plan treatments. Parents and caregivers can also understand the process better. While you can’t test for leukemia at home, knowing the signs can lead to early medical help.
Leukemia diagnosis has come a long way. Research keeps improving treatment results. Families can get support and resources, like those from the Tap Society, by staying informed and working with healthcare providers.
FAQ’s:
How is childhood leukemia diagnosed?
Doctors use a few methods to find childhood leukemia. They look at the child’s health history and do tests. These include a Complete Blood Count (CBC), a blood smear, and bone marrow tests.
What are the common lab abnormalities in childhood leukemia?
Kids with leukemia often have low blood counts. This can be seen in a CBC and blood smear. It shows signs of anemia, low platelets, and too many white blood cells.
What is the role of CBC in diagnosing leukemia?
The CBC is key in finding leukemia. It spots problems like anemia and too many white blood cells. These signs point to leukemia.
How do you test for leukemia at home?
You can’t test for leukemia at home. Only a doctor can do the tests needed for a diagnosis.
What are the symptoms of childhood leukemia?
Kids with leukemia might bruise easily or have low fevers. They might also have swollen lymph nodes.
How do cytogenetic and molecular abnormalities impact treatment and outcome?
These abnormalities help doctors know what type of leukemia it is. They also help predict how well it will respond to treatment. This affects the treatment plan and how well the child will do.
What is the difference between ALL and AML in laboratory tests?
Tests can tell if it’s ALL or AML. Blood work, special tests, and staining patterns help make this distinction.
How can parents and caregivers interpret lab results?
Parents and caregivers can talk to the child’s doctor about lab results. They can ask questions and keep track of how the child is doing.
What are the advanced diagnostic techniques used in leukemia diagnosis?
New tests like flow cytometry and next-generation sequencing help diagnose leukemia. They also check for any remaining cancer cells.
How is pancytopenia recognized and managed?
Pancytopenia is found through a CBC. It’s treated right away because it’s a serious condition.
What is the significance of peripheral blood smear findings in leukemia diagnosis?
Blood smear findings are very important. They show if there are cancer cells in the blood. This helps doctors diagnose leukemia.
References
- Medical News Today. (2024). Leukemia survival rates by age: Is it curable? https://www.medicalnewstoday.com/articles/322990