Last Updated on December 3, 2025 by Bilal Hasdemir

The fact that nearly 1 in 8 men will get prostate cancer in their lifetime highlights how significant this health issue is in the United States. Early detection plays a crucial role, with a 5-year survival rate of almost 98%, demonstrating the importance of early diagnosis and treatment. When considering treatment options, the prostate cancer best treatment success rates are highest when the disease is caught early, maximizing the chances of a cure and long-term survival.
Key Takeaways
- Early detection greatly boosts the 5-year survival rate for prostate cancer patients.
- The best treatments depend on the cancer’s stage and how severe it is.
- A nearly 98 percent 5-year survival rate is possible with early detection and treatment.
- Effective plans often mix different therapies based on the patient’s needs.
- Getting diagnosed early is critical for better treatment results and survival.
Understanding Prostate Cancer: Types, Stages, and Risk Levels
Prostate cancer comes in different forms, from low-risk to aggressive. Knowing the type, stage, and risk level is key for the right treatment. This helps doctors choose the best plan for each patient.
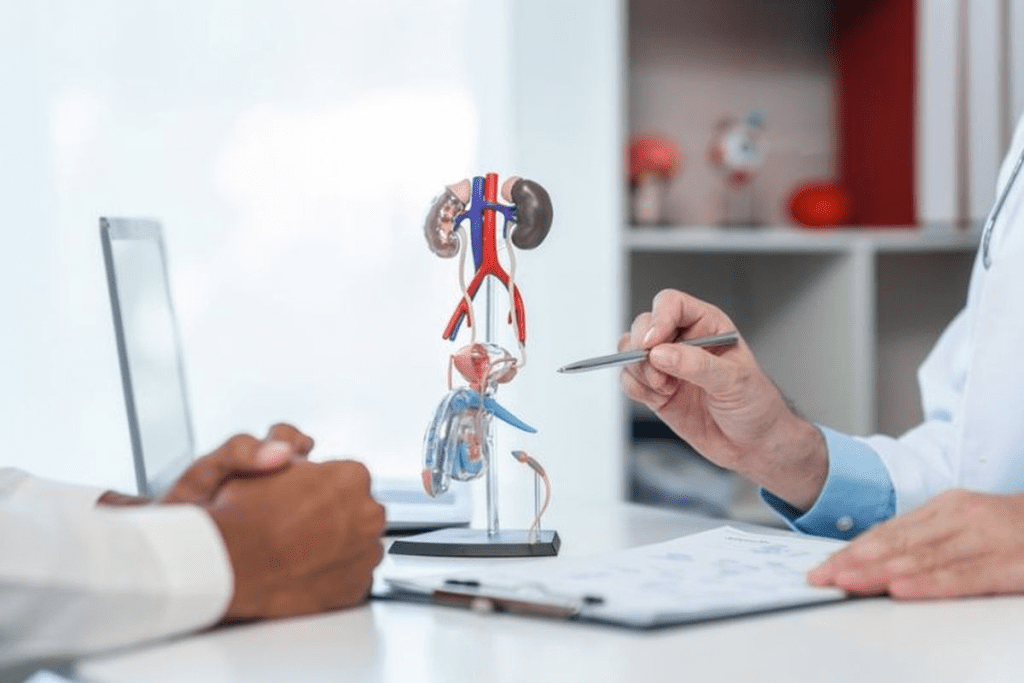
Defining Prostate Cancer and Its Prevalence
Prostate cancer is a tumor in the prostate gland, a gland below the bladder in men. It’s a common cancer in men, often in the U.S. The American Cancer Society says it’s the second leading cause of cancer death in men.
Prevalence of Prostate Cancer: The risk of prostate cancer changes with age, race, and family history. Men over 65, those with a family history, and African American men face higher risks.
| Risk Factor | Description | Impact on Risk Level |
| Age | Risk increases with age, after 65 | High |
| Family History | Having a father or brother with prostate cancer | Moderate to High |
| Race | African American men are at higher risk | High |
Common Risk Factors and Early Detection
Early detection is key for treating prostate cancer. Risk factors include age, family history, and race. Men with a family history should get screened early.
“The earlier prostate cancer is detected, the better the chances for successful treatment and survival.” –
American Cancer Society
Early detection methods include the PSA test and DRE. Knowing these methods helps men make informed health choices.
The stage of prostate cancer shows how far it has spread. This, along with the cancer’s grade and the patient’s health, helps decide the treatment. It’s important for doctors to know this to choose the right treatment.
How Success is Measured in Prostate Cancer Treatment
Measuring success in prostate cancer treatment looks at survival rates and quality of life. This approach helps us see how well treatments work. It’s key to understanding the best ways to fight cancer.
5-Year Survival Rates as a Benchmark
The 5-year survival rate is a key measure. It shows the percentage of patients alive 5 years after diagnosis. The American Cancer Society says survival rates for prostate cancer have gone up a lot.
A high 5-year survival rate means treatment is working well. But, survival rates can change based on cancer stage and grade.
Beyond Survival: Quality of Life Considerations
Survival rates are important, but so is quality of life. Treatments for prostate cancer can cause side effects like incontinence and erectile dysfunction. These can affect how well a patient lives.
Success in treating prostate cancer also means keeping patients active and happy. Doctors aim to control cancer while keeping side effects low.
Biochemical Recurrence and PSA Monitoring
Biochemical recurrence is when PSA levels go up after treatment. This is a big factor in treatment success. PSA monitoring helps catch recurrence early.
How often PSA tests are done depends on treatment and risk factors. For some, regular tests are key to catching recurrence and adjusting treatment.
Knowing about PSA monitoring and biochemical recurrence is key to managing prostate cancer. It helps ensure the best results for patients.
Surgical Approaches: Radical Prostatectomy
Radical prostatectomy is a key treatment for prostate cancer. It removes the prostate gland and can cure many patients. It’s mainly used for early-stage prostate cancer.
Types of Prostatectomy Procedures
There are different ways to do radical prostatectomy. Each method has its own benefits and things to consider. The choice depends on the cancer’s stage, the patient’s health, and the surgeon’s skill.
Open vs. Robotic-Assisted Techniques
Radical prostatectomy can be done in two ways: open surgery or robotic-assisted surgery. Robotic-assisted surgery is more popular. It’s known for its precision, less blood loss, and quicker recovery.
A study showed robotic-assisted surgery has fewer complications and shorter hospital stays. Here’s a comparison of the two methods:
| Characteristics | Open Radical Prostatectomy | Robotic-Assisted Radical Prostatectomy |
| Surgical Precision | High | Very High |
| Blood Loss | Moderate to High | Low |
| Recovery Time | Longer | Shorter |
An expert says robotic-assisted surgery has changed urology. It gives patients a precise and less invasive way to treat prostate cancer. This shows how prostate cancer surgery is getting better.
“Robotic prostatectomy has become a standard of care for many patients with localized prostate cancer, promising fewer side effects and a quicker recovery.”
The surgery cure rate for radical prostatectomy depends on several things. These include the cancer’s stage and the patient’s health. Early-stage cancer has a better chance of being cured with this surgery.
Radiation Therapy Options and Success Rates
Radiation therapy is a key treatment for prostate cancer. It offers different options based on each patient’s needs. This treatment has improved a lot, helping many patients live better lives.
External Beam Radiation Therapy (EBRT)
External Beam Radiation Therapy (EBRT) is a non-invasive treatment. It uses beams from outside the body to kill cancer cells. It works well for localized prostate cancer.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) is a more advanced EBRT. It shapes the radiation beams to fit the tumor. This method helps protect healthy tissues, reducing side effects and improving results.
Brachytherapy (Internal Radiation)
Brachytherapy involves placing small radioactive seeds in or near the prostate. It delivers radiation directly to the tumor, sparing healthy tissues. It can be used alone or with EBRT, based on the cancer’s risk and stage.
The success rates of radiation therapy, like EBRT and brachytherapy, are high. Studies show these treatments can control localized prostate cancer well. Many patients have few side effects. The choice between EBRT and brachytherapy depends on the cancer’s stage, grade, and the patient’s health.
Key considerations for radiation therapy include side effects like urinary issues, bowel problems, and fatigue. But, new technology and better planning have lowered these risks. Patient-specific factors are important in choosing the best radiation therapy.
Active Surveillance: When Watching is the Best Treatment
Active surveillance changes how we think about treating prostate cancer. It means watching the cancer closely with regular tests and check-ups. This way, men with low-risk cancer can avoid the side effects of aggressive treatments.
Candidates for Active Surveillance
Not every man with prostate cancer can use active surveillance. It’s best for those with low-risk prostate cancer. This means a low Gleason score, low PSA levels, and a small tumor. Doctors look at the patient’s health and cancer details to decide if active surveillance is right.
Monitoring Protocols and Triggers for Intervention
Active surveillance requires regular PSA tests, digital rectal exams (DREs), and biopsies. These tests happen every 6 to 12 months. If the PSA levels go up, the Gleason score changes, or the cancer grows, it’s time to consider more treatment.
Quality of Life During Active Surveillance
Active surveillance helps keep quality of life high. It avoids the side effects of aggressive treatments like incontinence and impotence. Men on active surveillance can live active lives, knowing they’re being closely watched.
Choosing active surveillance means men with low-risk cancer can manage their disease carefully. They can keep their quality of life high and avoid unnecessary treatment.
Hormone Therapy and Androgen Deprivation
Hormone therapy is a key treatment for prostate cancer. It works because prostate cancer cells need male hormones, or androgens, to grow. Testosterone is a major hormone involved.
By lowering androgen levels or blocking their effect, hormone therapy can slow cancer growth. It’s helpful for advanced cancer or when surgery or radiation isn’t an option.
How Hormone Therapy Works Against Prostate Cancer
Hormone therapy reduces androgen production or blocks their action on cancer cells. It can be done through surgery or medical treatments.
Androgen deprivation therapy (ADT) lowers androgen levels. ADT uses medications like GnRH agonists and antagonists to reduce testosterone production.
Abiraterone and Next-Generation Hormone Treatments
Abiraterone acetate is a new hormone treatment for advanced prostate cancer. It blocks the CYP17 enzyme, which makes androgens in the testes and cancer cells.
Studies show abiraterone can extend life for men with advanced prostate cancer. It’s a valuable treatment option for this stage.
Hormone Therapy Benefit vs. Side Effects
Hormone therapy controls prostate cancer but has side effects. Common issues include hot flashes, fatigue, weight gain, and low libido. Serious side effects can include osteoporosis and heart disease.
It’s important to consider both the benefits and side effects of hormone therapy. For many, the cancer control is worth the risks.
| Treatment Aspect | Hormone Therapy | Other Treatments |
| Mechanism of Action | Reduces androgen levels or blocks their action | Varies (surgery, radiation, chemotherapy) |
| Common Side Effects | Hot flashes, fatigue, weight gain, decreased libido | Varies (e.g., urinary issues with surgery, fatigue with radiation) |
| Use in Advanced Disease | Commonly used | Limited use for some treatments (e.g., surgery not typically used for advanced disease) |
Prostate Cancer Best Treatment Success: Combination Approaches
Prostate cancer treatment has evolved with combination therapies. These have shown high success rates. Healthcare providers can tailor treatments to meet individual patient needs, leading to better outcomes.
Hormone-Radiation Combination Therapy
Hormone-radiation combination therapy is a big step forward in treating prostate cancer. It combines hormone therapy to lower testosterone levels with radiation therapy to kill cancer cells. This combo has been shown to improve survival rates and lower cancer recurrence risk.
Clinical trials have proven the effectiveness of this therapy. It’s best for patients with intermediate to high-risk prostate cancer. This approach helps control tumors better and reduces metastatic disease.
Multimodal Treatment for High-Risk Disease
For high-risk prostate cancer, multimodal treatment is used. This combines surgery, radiation, and hormone therapy. Treatments are tailored to the patient’s risk and health.
Multimodal treatment improves cancer control and survival rates. It addresses cancer from all sides, leading to better outcomes and quality of life for patients.
Case Studies of Successful Combination Therapies
Many case studies show the success of combination therapies in prostate cancer treatment. For example, a patient with high-risk cancer might get hormone therapy before radiation. This can significantly reduce the tumor and improve survival.
These examples show how combination therapies can change prostate cancer treatment. They allow for personalized plans that meet each patient’s unique needs.
- Combination therapy offers improved treatment outcomes for prostate cancer patients.
- Hormone-radiation combination therapy is effective for intermediate to high-risk disease.
- Multimodal treatment approaches provide complete care for high-risk prostate cancer.
Comparing Prostatectomy vs. Radiation: Which is More Successful?
Prostatectomy and radiation therapy are both good ways to treat prostate cancer. Each has its own good and bad points. The right choice depends on the cancer’s stage, risk, and the patient’s health and wishes.
Success Rates by Cancer Stage and Risk Level
Research shows both treatments work well for prostate cancer. Success rates change with the cancer’s stage and risk. For example, a study in the Journal of Clinical Oncology found similar 5-year survival rates for low-risk cancer with both treatments.
- Low-risk prostate cancer: Both treatments have high success rates, with surgery sometimes being a bit better.
- Intermediate-risk prostate cancer: Radiation with hormone therapy is as good as surgery.
- High-risk prostate cancer: Radiation and hormone therapy together are often suggested.
Side Effect Profiles and Quality of Life
The side effects of prostatectomy and radiation can really affect a patient’s life. Knowing these side effects is key to making a good choice.
Prostatectomy Side Effects:
- Urinary incontinence
- Erectile dysfunction
Radiation Therapy Side Effects:
- Urinary frequency and urgency
- Bowel irritation
- Erectile dysfunction (less common than with surgery)
Patient Experiences and Satisfaction
People’s experiences with prostatectomy and radiation vary a lot. This depends on how the treatment affects their life and if they’re happy with their choice.
“I chose surgery because I wanted to remove the cancer entirely. The recovery was tough, but I’m glad I made that choice.” – A prostate cancer survivor
A study looked at what patients said about their treatments. It found both had tough parts, but many were very happy with their choice. This shows how important it is to choose what’s best for you.
Advanced and Metastatic Prostate Cancer Treatments
Managing advanced prostate cancer involves various therapies. These include radiopharmaceuticals and immunotherapy. They aim to tackle the challenges of metastatic prostate cancer. This improves patient outcomes and quality of life.
Radiopharmaceuticals and Targeted Therapies
Radiopharmaceuticals are a key treatment for metastatic prostate cancer, mainly for bone metastases. They combine radiation therapy with targeted delivery. This reduces side effects and boosts effectiveness.
- Radium-223 is a radiopharmaceutical that helps treat bone metastases. It improves survival and eases symptoms.
- New targeted therapies are being developed. They offer hope for future treatments.
Immunotherapy Approaches
Immunotherapy is a groundbreaking method for treating advanced prostate cancer. It uses the body’s immune system to fight cancer more effectively.
Treating Bone Metastases
Bone metastases are a common issue in advanced prostate cancer. They cause a lot of pain. Treatments like radiopharmaceuticals and bisphosphonates help manage pain and prevent bone damage.
- Radium-223 and other radiopharmaceuticals target bone metastases directly.
- Bisphosphonates and denosumab strengthen bones and prevent fractures.
These advanced treatments show the progress in managing metastatic prostate cancer. They offer new hope and better quality of life for patients.
Personalized Treatment: Finding Your Best Option
Prostate cancer treatment has changed a lot. Now, it focuses on personalized medicine. This means doctors use genetic testing and biomarkers to create treatment plans that fit each patient.
The Role of Genetic Testing and Biomarkers
Genetic testing and biomarkers are key in treating prostate cancer. They help find out what genetic changes are in the cancer cells. This information helps doctors choose the right treatment.
Biomarkers are special molecules in the body that show if there’s a problem. In prostate cancer, things like PSA levels and tests for BRCA1 and BRCA2 help doctors decide how to treat you.
Age, Health Status, and Treatment Selection
Your age and health are important when picking a treatment for prostate cancer. Older or sicker patients might get treatments that are less harsh. Younger, healthier patients might get more aggressive treatments.
It’s important to think about how treatments might affect your life. For example, some treatments might help you keep your urinary and sexual function. Even if they’re not the most effective against cancer.
Questions to Ask Your Doctor
- What are my treatment options based on my genetic profile and overall health?
- How will my age and health status influence my treatment plan?
- What are the possible side effects of the treatments I’m considering, and how can they be managed?
- Are there any new clinical trials or treatments that might be right for me?
Talking to your doctor about these things can help you make a good choice. This way, you get a treatment plan that really works for you.
Conclusion: The Future of Prostate Cancer Treatment
The world of prostate cancer treatment is changing fast. New medical tech and a better understanding of the disease are leading the way. Patients will soon have more effective and personalized treatments.
New breakthroughs in radiation, surgery, and hormone therapy have made a big difference. Genetic testing and biomarkers are helping doctors tailor treatments. This means better care for each patient.
The future looks bright for prostate cancer treatment. Research into new therapies and immunotherapy is underway. These advances will give patients more options, improving their lives and chances of survival.
The medical community is dedicated to improving care for prostate cancer patients. They are working hard to offer the best treatments available.
FAQ
What is the most successful treatment for prostate cancer?
The best treatment for prostate cancer varies. It depends on the cancer’s stage and risk, and the patient’s health. Options include surgery, radiation, active surveillance, hormone therapy, and combining treatments.
How is prostate cancer staged, and how does it affect treatment decisions?
Prostate cancer is staged based on the tumor’s size, lymph node involvement, and metastasis. The stage guides the treatment choice. Early-stage cancer might get surgery or radiation. Advanced cancer often gets hormone therapy or systemic treatments.
What is the role of PSA monitoring in tracking treatment effectiveness?
PSA monitoring tracks treatment success. A drop in PSA levels means good results. But, a rise might signal cancer return or growth.
What are the benefits and risks of robotic-assisted prostatectomy?
Robotic-assisted prostatectomy has benefits like less blood loss and quicker recovery. But, it also risks urinary incontinence and erectile dysfunction.
How does brachytherapy work, and what are its success rates?
Brachytherapy places radioactive seeds in the prostate. It’s very effective for early-stage cancer. Success rates are similar to surgery and external beam radiation.
What is active surveillance, and who is a candidate for it?
Active surveillance is for low-risk prostate cancer. It involves regular checks and biopsies. It’s for those with low-risk cancer, older patients, or those with health issues.
How does hormone therapy work against prostate cancer?
Hormone therapy lowers male hormones that feed cancer growth. It’s often used with other treatments to boost their effect.
What is the benefit of combination therapy in treating prostate cancer?
Combination therapy, like hormone-radiation therapy, targets cancer from different angles. It’s used for high-risk or advanced cancer to improve outcomes.
How do I choose between prostatectomy and radiation therapy?
Choosing between prostatectomy and radiation depends on cancer stage and risk, and patient health. Both have similar success rates but differ in side effects and quality of life.
What are the treatment options for advanced and metastatic prostate cancer?
Advanced prostate cancer treatments include hormone therapy, chemotherapy, radiopharmaceuticals, and immunotherapy. The goal is to control cancer, manage symptoms, and improve life quality.
How does genetic testing and biomarkers inform personalized treatment?
Genetic testing and biomarkers reveal cancer specifics like mutations or protein expression. This info helps tailor treatments, improving outcomes and reducing side effects.
What is the role of age and health status in treatment selection?
Age and health status are key in choosing treatments. They affect tolerance to treatments. Older patients or those with health issues may need more conservative or palliative approaches.
References
Santarelli, V., et al. (2025). Latest advancements and future directions in prostate cancer therapy: Partial prostatectomy and focal treatments as alternatives to radical surgery. Cancers, 17(18), Article 4631.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12468631
Chakrabarti, D. (2025). The contemporary management of prostate cancer: Balancing active treatment and quality of life. Cancer Treatment Reviews, 107, 102391.
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/caac.70020
Bigarella, M. P., et al. (2025). Multidisciplinary management of nonmetastatic locally advanced prostate cancer. Journal of Urology, 214(3), 523-532.
https://www.sciencedirect.com/science/article/pii/S2950247025000167
Yong, R. L., & Zacharia, B. E. (2024). A review of prostate cancer focal therapies in general practice. Australian Journal of General Practice, 53(9), 610-616.
https://www1.racgp.org.au/ajgp/2025/september/a-review-of-prostate-cancer-focal-therapies-in-gen