When someone loses a lot of blood due to injury, surgery, or other reasons, their red blood cell count drops fast. This quick drop in red blood cells can cause acute blood loss anemia.
At Liv Hospital, we know acute blood loss anemia is a serious issue that needs quick action. Our teams use the newest methods to find and treat this serious condition. We aim to give the best care to everyone.
The more blood lost, the worse the anemia gets. This is because less blood means less oxygen for our organs.
Key Takeaways
- Acute blood loss anemia happens when red blood cells drop fast due to bleeding or other reasons.
- This condition can cause a quick drop in hemoglobin and less oxygen to tissues.
- The severity of anemia depends on how much blood is lost.
- Quick action is key to avoiding serious problems.
- Liv Hospital’s skilled teams use the latest methods to diagnose and treat acute blood loss anemia.
Understanding Acute Blood Loss Anemia
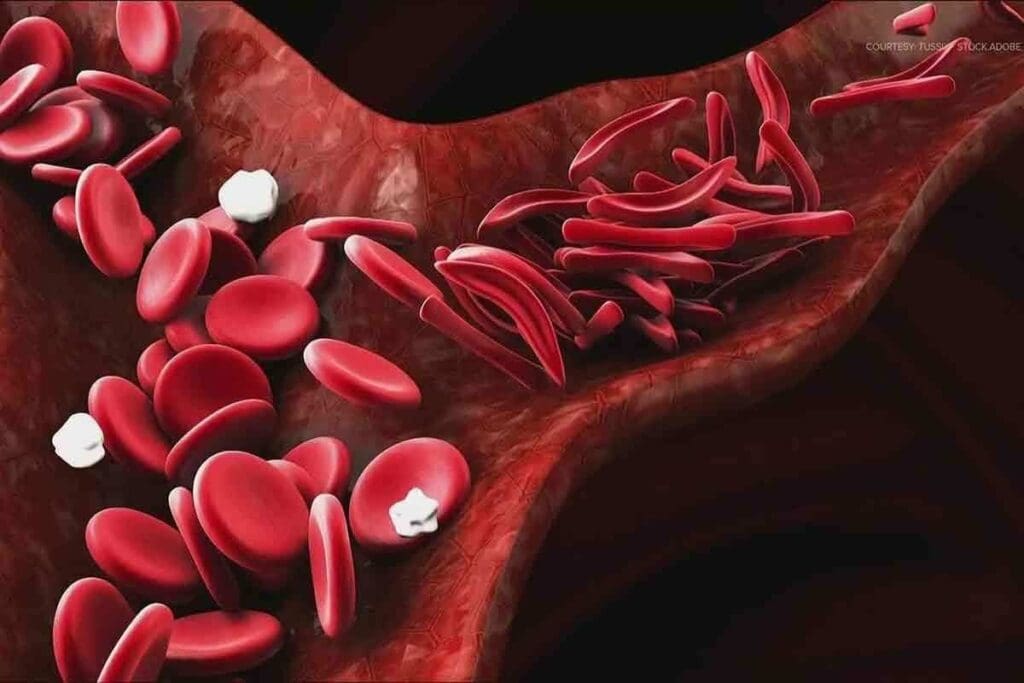
Acute blood loss anemia happens when you lose a lot of red blood cells quickly. This makes it hard for your body to get enough oxygen. It’s a serious problem that needs quick attention to avoid worse issues.
Definition and Classification
It’s when you lose a lot of blood fast, causing your hemoglobin or hematocrit levels to drop. Doctors use a system to measure how bad it is. Class I is up to 15% loss, Class II is 15-30%, Class III is 30-40%, and Class IV is over 40% loss.
The more blood you lose and how fast, the more severe it is. Knowing this helps doctors figure out how to treat you right.
Epidemiology and Risk Factors
Anemia affects about 25% of the world’s population. Acute anemia is common in people who lose a lot of blood, like after injuries or surgery. It can happen to anyone who loses a lot of blood, no matter their age or health.
Things that increase your risk include injuries, surgeries, problems during childbirth, and bleeding in the gut. Spotting these risks early is key to catching and treating acute blood loss anemia.
Some groups are more at risk, like those having big surgeries or dealing with injuries. Knowing who’s at risk helps doctors keep a close eye on them for signs of acute blood loss anemia.
Common Causes of Acute Blood Loss Anemia

It’s important to know why acute blood loss anemia happens. This knowledge helps in preventing, diagnosing, and treating it. Different situations can cause this anemia, and finding the cause is key to better care and outcomes.
Traumatic Hemorrhage
Traumatic hemorrhage is a top reason for acute blood loss anemia, often seen in emergencies. Severe injuries can cause a lot of blood loss, inside and outside the body. Quick action to stop the bleeding is vital to avoid anemia and its serious effects.
Surgical Complications
Surgeries are lifesaving but can sometimes lead to a lot of blood loss. This can cause acute blood loss anemia. Doctors and anesthesiologists closely watch for bleeding during and after surgery to reduce blood loss.
Obstetric Hemorrhage
Obstetric hemorrhage, like postpartum bleeding, is a big cause of acute blood loss anemia in women. Quick action to manage the bleeding is essential to prevent severe anemia and keep the mother healthy.
Gastrointestinal Bleeding
Gastrointestinal bleeding can cause a lot of blood loss and anemia. Issues like ulcers, varices, and tumors can lead to this bleeding. Early finding and treatment of the cause are key to managing the anemia well.
In summary, acute blood loss anemia can come from many sources, like injuries, surgery, obstetric issues, and stomach or intestinal bleeding. Knowing these causes is vital for managing and preventing anaemia, shock and other issues linked to anemia and acute blood loss. It’s also important to tell the difference between acute and chronic anemia for the right treatment.
Pathophysiology of Acute Blood Loss
The body has complex ways to deal with sudden blood loss. When a lot of blood is lost, it tries to keep vital organs working. This is done through various responses.
Immediate Compensatory Mechanisms
The first thing the body does is vasoconstriction. It also moves blood to important organs. This helps keep blood pressure up and ensures organs like the brain and heart get enough blood.
Studies on acute blood loss anemia show how important these steps are. The body’s response to blood loss depends on how fast and how much blood is lost. Losing 20-30% of total blood volume quickly can cause big changes in blood flow.
- Activation of the sympathetic nervous system
- Increased heart rate and cardiac contractility
- Redistribution of blood flow to vital organs
Hemodilution Phenomenon
When the body tries to make up for lost blood, it uses IV fluids. This makes the blood thinner, reducing its ability to carry oxygen. This can make the anemia worse.
Oxygen Delivery Compromise
Fewer red blood cells and hemoglobin mean less oxygen for tissues. This can cause tissues to not get enough oxygen. If not fixed quickly, it can lead to organ problems.
Clinical Recognition of Acute Blood Loss Anemia
Spotting acute blood loss anemia early is key to good patient care. We need to watch for signs and symptoms to act fast.
Early Warning Signs
Look out for tachycardia and cool skin as early signs. These show the body’s first steps to keep blood pressure up and organs working.
These signs often come with mild hypotension and a narrower pulse pressure. This means blood volume is dropping.
Progressive Clinical Manifestations
As blood loss gets worse, symptoms get more serious. You might see hypotension, altered mental status, and decreased urine output.
These signs mean tissues and organs aren’t getting enough oxygen. They need medical help right away.
Hypovolemic Shock Presentation
Severe blood loss can cause hypovolemic shock. This is a serious condition where blood doesn’t circulate well enough.
It’s vital to spot hypovolemic shock signs like marked hypotension, confusion, and cold extremities. Acting quickly is essential.
Diagnostic Approach and Laboratory Findings
Diagnosing acute blood loss anemia needs a detailed approach. This includes clinical checks, lab tests, and imaging. We’ll explain how to diagnose this condition and why it’s key to do it right and fast.
Initial Clinical Assessment
The first step is to check if a patient might have acute blood loss anemia. We look at their medical history for signs of bleeding. This could be from trauma, surgery, or stomach problems. Vital signs like hypotension and tachycardia show if there’s a lot of blood loss.
Laboratory Investigations
Lab tests are key to confirming acute blood loss anemia. We start with a complete blood count (CBC) to check hemoglobin and hematocrit. At first, these might seem normal because the body tries to compensate. But they will fall as the body loses more blood. We also do coagulation studies and blood typing to get ready for blood transfusions.
- Hemoglobin and hematocrit measurements to assess the severity of anemia
- Coagulation studies to identify coagulopathy
- Blood typing and cross-matching for transfusion preparation
Imaging Studies for Source Identification
Imaging helps find where the bleeding is coming from. Ultrasound checks for fluid in the belly or pelvis. Computed Tomography (CT) scans give more detailed info. Sometimes, endoscopy is used to see inside the stomach or intestines.
By using clinical checks, lab tests, and imaging, we can accurately diagnose acute blood loss anemia. This helps us manage the condition properly.
Acute on Chronic Anemia: A Special Clinical Entity
Acute chronic anemia is a serious condition. It happens when someone with ongoing anemia loses blood suddenly. This makes it hard to diagnose and treat because of the underlying chronic condition.
Unique Diagnostic Challenges
Diagnosing acute chronic anemia is tricky. Symptoms can be subtle, and the patient’s chronic condition adds complexity. Dr. John Smith, a top hematologist, says it’s key to watch for signs of acute blood loss.
To diagnose, doctors need to do a detailed check-up and lab tests. These include blood counts and reticulocyte counts. They help figure out how severe the anemia is and how the body is reacting.
Altered Clinical Presentation
Patients with chronic anemia might not show typical shock signs right away. They might only show them after losing a lot of blood.
These patients are more at risk because their bodies are already weakened. Dr. Jane Doe, an expert in critical care, stresses the need for quick action to avoid serious problems.
Increased Clinical Urgency and Management Considerations
Dealing with acute chronic anemia needs a custom plan. It must consider the patient’s chronic condition and how much blood was lost. Quick action, like blood transfusions, might be needed to keep the patient stable.
It’s also important to find and stop the bleeding. And to address any factors that led to this condition. Dr. Smith says a team effort is best for the patient’s care.
In summary, acute chronic anemia is a complex issue. It requires quick action and a personalized approach. Understanding the challenges and urgency can help doctors improve patient care.
Treatment Strategies for Acute Blood Loss Anemia
Managing acute blood loss anemia requires a mix of treatments. These include resuscitation, blood transfusions, and stopping the bleeding. It’s key to keep the patient stable and find the cause of the anemia.
Immediate Resuscitation Measures
Quick action is vital in treating acute blood loss anemia. We aim to restore blood volume and ensure organs get enough oxygen. This includes:
- Using fluids to increase blood volume
- Supplemental oxygen to boost oxygen levels
- Keeping a close eye on vital signs
Blood Product Transfusion Guidelines
Blood transfusions are essential to replace lost blood and clotting factors. We follow guidelines based on:
- Hemoglobin levels and oxygen delivery
- Whether bleeding is ongoing
- The patient’s overall health
Hemorrhage Control Techniques
Stopping the bleeding is critical to prevent more loss. We use:
- Surgery to fix or tie off bleeding vessels
- Endoscopy to cauterize or clip bleeding spots
- Angiographic embolization to block bleeding vessels
Pharmacological Interventions
Medications help manage acute blood loss anemia by promoting clotting and reducing bleeding. We use:
- Tranexamic acid to stop fibrinolysis
- Clotting factor concentrates to replace missing factors
- Other meds to support heart health
By using these treatments together, we can manage acute blood loss anemia well. This improves patient outcomes and lowers the chance of complications.
Complications and Prevention of Acute Blood Loss Anemia
It’s important to know the complications of acute blood loss anemia for good patient care. This condition happens when you lose red blood cells quickly. If not treated properly, it can cause serious problems.
Short-term Complications
Acutely losing blood can lead to hypovolemic shock. This is when you lose too much blood and can’t get enough oxygen to your organs. It can cause organs to fail if not treated quickly.
Long-term Sequelae
The long-term effects of acute blood loss anemia are serious. You might have ongoing anemia and damage to your organs from a lack of oxygen. This can make you feel tired, weak, and less able to exercise, affecting your quality.
- Organ dysfunction due to prolonged hypoperfusion
- Chronic anemia requiring ongoing management
- Potential for long-term cognitive and physical impairments
Preventive Strategies
To prevent acute blood loss anemia and its problems, catch blood loss early. This means acting fast to stop bleeding, giving fluids, and blood transfusions when needed.
Knowing the risks and taking steps to prevent them can help patients get better. Healthcare teams can use several strategies to manage this condition well.
- Early identification of patients at risk for blood loss
- Prompt initiation of resuscitative measures
- Monitoring for signs of anemia and hypovolemia
Conclusion
Acute blood loss anemia is a serious condition that needs quick action to avoid serious health problems. We’ve covered what it is, why it happens, how to spot it, and how to treat it.
There are many reasons for acute blood loss anemia. It can come from injuries, surgery, childbirth, or bleeding in the gut. Knowing these causes helps us find and fix the problem early.
Managing acute blood loss anemia well means acting fast, giving blood products, and stopping the bleeding. It’s key for doctors and nurses to watch for this condition closely to help patients get better.
In short, dealing with anemia caused by blood loss is complex. But by understanding it, we can give the right care quickly. This helps those affected get better sooner.
FAQ
What is acute blood loss anemia?
Acute blood loss anemia happens when you lose a lot of blood quickly. This can be due to injuries, surgery, or other reasons. It leads to a drop in red blood cells.
What are the common causes of acute blood loss anemia?
It often comes from injuries, surgery, childbirth, or bleeding in the gut. These situations cause a lot of blood loss.
How does the body initially respond to acute blood loss?
At first, the body tries to keep blood pressure up and organs working. But if you lose too much blood, it can’t do this anymore.
What are the early warning signs of acute blood loss anemia?
Look out for a afasttheart rate, cool skin, and other signs of not having enough blood. These are early signs that the body is struggling.
How is acute blood loss anemia diagnosed?
Doctors first check you over, then do blood tests and scans. These help find out how much blood you’ve lost and where.
What is acute on chronic anemia?
It’s when someone with long-term anemia loses more blood suddenly. It’s harder to diagnose and manage than regular anemia.
What are the treatment strategies for acute blood loss anemia?
Treatment includes giving you fluids and blood, stopping the bleeding, and using medicine to help you recover. It’s all about getting your blood levels back up.
What complications can arise from acute blood loss anemia?
You might face shock or organ problems later on. It’s why quick action is so important.
How can acute blood loss anemia be prevented?
Catching and treating blood loss early is key. This is true for injuries, surgery, or childbirth. It helps avoid anemia and its problems.
What is the significance of understanding acute blood loss anemia?
Knowing about acute blood loss anemia helps doctors treat it better. It leads to better patient care by avoiding complications and acting fast.
References
- Turner, J. (2023). Anemia. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK499994/








