
At Liv Hospital, we are dedicated to providing top-quality cardiac care and full support for international patients. Understanding the connection between acute coronary artery thrombus and heart attacks is vital for quick and effective treatment.
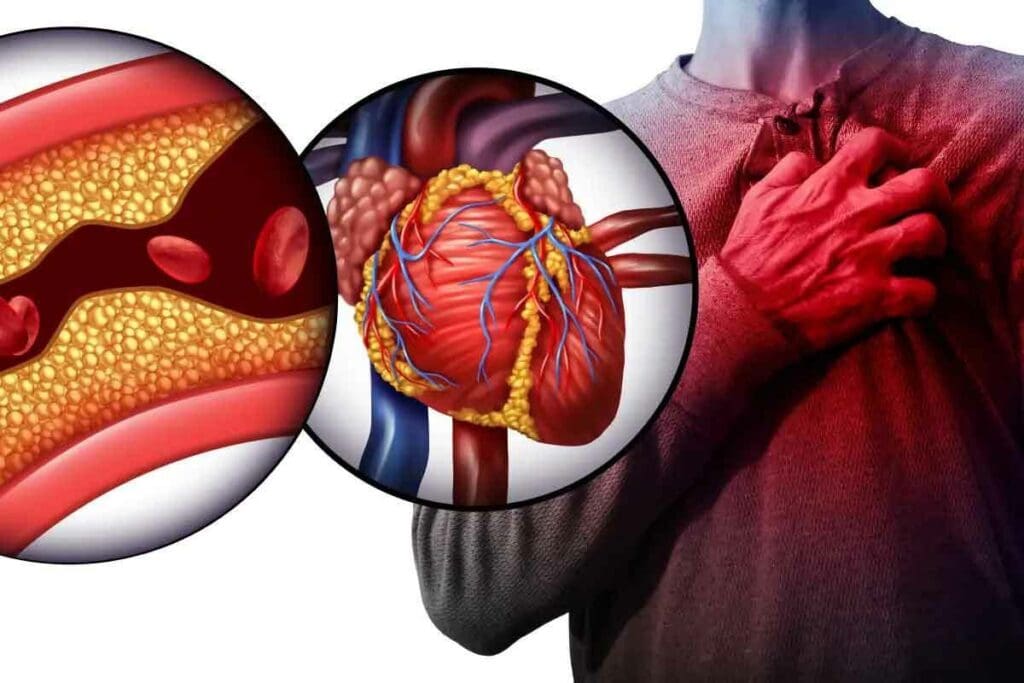
Acute coronary syndrome (ACS) occurs when blood flow to the heart suddenly decreases, often due to an acute coronary artery thrombus—a blood clot that blocks a coronary artery. This blockage can lead to a heart attack if not treated immediately.
At Liv Hospital, our cardiology team is fully equipped to diagnose and manage acute coronary artery thrombus using advanced techniques and evidence-based care. We focus on delivering timely, effective treatment to save lives and ensure the best outcomes for our patients.
Key Takeaways
- Coronary thrombosis is a critical factor in heart attacks.
- Understanding this condition is vital for effective treatment.
- Liv Hospital provides world-class cardiac care and international patient support.
- Timely treatment is key to saving lives.
- Advanced treatment approaches greatly improve patient outcomes.
The Nature of Acute Coronary Artery Thrombus
A blood clot in the coronary arteries is called acute coronary artery thrombus. It’s a serious issue that can harm your heart. We’ll look into what it is and how it affects people worldwide.
Definition and Medical Terminology
Acute coronary artery thrombosis means a sudden blockage in a coronary artery by a blood clot. This is a medical emergency because it can cause a heart attack. The terms used to describe it are complex, like thrombus, coronary occlusion, and myocardial ischemia.
Understanding these terms is key for doctors and patients. It helps them grasp the seriousness of acute coronary artery thrombus.
The term “acute” means it happens quickly, often in hours or minutes. “Thrombus” is the blood clot inside a blood vessel. In coronary artery thrombosis, this clot blocks blood flow to the heart muscle. This can damage or kill heart tissue because of lack of oxygen.
Prevalence and Global Impact
Coronary artery thrombosis is a big health problem worldwide. It’s a major cause of illness and death, says the World Health Organization (WHO). In the United States, it affects millions, with many experiencing acute coronary syndromes, including thrombosis.
The impact of acute coronary artery thrombus goes beyond death rates. It also affects healthcare costs, productivity, and family well-being. Quick and effective treatment is needed to reduce damage and improve results. We must understand the widespread effects of coronary artery thrombosis to fight it better.
Coronary Artery Anatomy and Function

The coronary circulation is key to keeping the heart healthy. It’s a network of arteries, veins, and capillaries. They supply blood to the heart’s muscle layer.
Structure of Coronary Circulation
The coronary circulation mainly includes the left and right coronary arteries. These start from the aortic root. They branch into smaller vessels like the left anterior descending artery and the circumflex artery. These vessels carry oxygenated blood to the heart’s different areas.
Important parts of the coronary circulation are:
- The left main coronary artery, splitting into the left anterior descending and circumflex arteries.
- The right coronary artery, which feeds the right atrium, parts of the right ventricle, and sometimes the left ventricle.
- Capillaries, where oxygen, nutrients, and waste are exchanged.
Vital Role in Cardiac Health
The coronary circulation is vital for heart health. It brings oxygen and nutrients to the heart muscle. Any blockage, like a thrombus, can cause reduced blood flow or even heart tissue death, known as a heart attack.
The role of coronary circulation is seen in several ways:
- It supplies oxygen and nutrients to the heart muscle.
- It removes waste from the heart tissue.
- It controls blood flow based on the heart’s needs.
Keeping the coronary circulation healthy is essential. It helps prevent heart diseases and ensures the heart stays well.
Pathophysiology of Acute Coronary Artery Thrombus
The pathophysiology of acute coronary artery thrombus starts with atherosclerosis development. Atherosclerosis is when plaque builds up in the arteries. This can cause many heart diseases.
Atherosclerosis Development
Atherosclerosis plays a big role in coronary thrombosis. It starts with lipids and inflammatory cells building up in the artery walls. This leads to plaque formation.
Factors like high blood pressure, high cholesterol, and smoking make atherosclerosis worse. These factors hurt the artery lining, making it easier for harmful cells to stick and move into the artery.
Plaque Rupture Mechanisms
Plaque rupture is a key event in acute coronary artery thrombus. When a plaque bursts, the fatty core inside is exposed. This starts the thrombotic cascade.
The likelihood of a plaque rupturing depends on its makeup and inflammation level. Plaques with thin caps and lots of fat are more likely to burst.
Thrombotic Cascade
The thrombotic cascade is a complex series of events. When a plaque bursts, platelets stick to the exposed area. They get activated and send out signals.
These signals make more platelets stick and activate, starting the coagulation cascade. This leads to a fibrin clot forming. The clot can block the artery, causing heart problems.
Understanding the thrombotic cascade is key to finding ways to stop and treat coronary thrombosis.
From Thrombus to Heart Attack: The Causal Relationship
Acute coronary artery thrombus formation is a key moment in heart attack pathogenesis. It leads to ischemia and can cause infarction. When a thrombus blocks a coronary artery, it stops blood flow to the heart muscle. This triggers a series of events that can lead to a heart attack.
Myocardial Ischemia Process
Myocardial ischemia happens when the heart doesn’t get enough blood. This is often due to a blockage in the coronary arteries, caused by a thrombus. The process involves several steps:
- Reduced blood flow due to coronary artery occlusion
- Insufficient oxygen delivery to the heart muscle
- Impaired cardiac function due to lack of nutrients
- Potential for arrhythmias or other complications
The severity and length of ischemia determine heart muscle damage. Prolonged ischemia can lead to myocardial infarction, or a heart attack.
Progression to Infarction
The transition from ischemia to infarction involves complex changes. When a coronary artery is blocked, the heart muscle downstream becomes ischemic. If the blockage stays, the ischemic muscle may die, leading to infarction.
The infarction process includes several stages:
- Initial ischemia due to reduced blood flow
- Cellular injury and necrosis
- Inflammation and repair processes
- Potential scarring and long-term cardiac remodeling
Understanding the link between coronary thrombosis, myocardial ischemia, and infarction is key for effective treatments. Early recognition and quick action can reduce heart attack damage and improve outcomes.
Risk Factors Contributing to Coronary Thrombosis
Coronary thrombosis happens for many reasons, both things we can change and things we can’t. Knowing these factors helps us prevent and manage coronary thrombosis.
Modifiable Risk Factors
Things we can change or control are called modifiable risk factors. These include:
- Smoking: Smoking harms the blood vessel lining, making blockages more likely.
- High Blood Pressure: High blood pressure damages coronary arteries, raising thrombosis risk.
- High Cholesterol: Too much LDL cholesterol causes artery plaque, leading to thrombosis.
- Diabetes: Diabetes increases coronary thrombosis risk by affecting blood vessels and the heart.
By changing our lifestyle and using medicine when needed, we can lower our risk of coronary thrombosis.
Non-Modifiable Risk Factors
Things we can’t change are called non-modifiable risk factors. These include:
- Family History: A family history of heart disease or thrombosis raises your risk.
- Age: Risk grows with age, more so after 45 for men and 55 for women.
- Gender: Men face higher risk, but women’s risk increases after menopause.
Even though we can’t change these factors, knowing them helps us plan better prevention and watch for risks.
By focusing on things we can change and understanding what we can’t, we can lower coronary thrombosis rates and its serious effects.
Recognizing the Signs and Symptoms
It’s key to know the signs of coronary thrombosis to get help fast. We need to spot how it can show up to act quickly.
Classic Presentation Patterns
The usual signs of coronary thrombosis include chest pain or discomfort. This feels like a squeeze or pressure. It might spread to the arms, back, neck, jaw, or stomach.
Other symptoms are shortness of breath, nausea, lightheadedness, or cold sweats. These happen when the heart muscle doesn’t get enough oxygen-rich blood, causing ischemia.
If you’re feeling these symptoms, get medical help right away. Spotting these signs early can greatly help your treatment.
Atypical and Silent Presentations
Not everyone shows the usual signs of coronary thrombosis. Some might have atypical presentations, with symptoms that are not typical or less clear. For instance, some might feel pain in the upper abdomen, get tired easily, or have palpitations without chest pain.
Also, some cases can be silent, with no symptoms at all. This is more common in people with diabetes or those who’ve had a heart attack before. Nerve damage can make it hard to feel pain.
Spotting these less common signs is tough but very important. Doctors need to think of coronary thrombosis, even if the symptoms don’t seem typical.
By knowing both the usual and unusual signs of coronary thrombosis, we can catch it sooner. This can save lives.
Diagnostic Approaches and Testing
To diagnose acute coronary thrombosis, doctors use a detailed plan. This plan includes emergency checks, cardiac biomarkers, and imaging tests. We’ll look at these steps to see how they help find coronary thrombosis.
Initial Emergency Assessment
The first step in diagnosing acute coronary thrombosis is very important. It involves quickly checking the patient’s symptoms, medical history, and physical exam. Electrocardiography (ECG) is a key tool here to spot signs of heart problems.
Doctors look for symptoms like chest pain, shortness of breath, and sweating. But, some patients might not show these signs, like diabetics or the elderly.
Cardiac Biomarkers
Cardiac biomarkers are proteins in the blood when heart cells are damaged. Troponin and creatine kinase-MB (CK-MB) are the most used biomarkers. High levels of these biomarkers mean heart damage, often from coronary thrombosis.
- Troponin: Very specific for heart damage, troponin stays high for days after a heart event.
- CK-MB: Less specific than troponin, but CK-MB is useful for diagnosing heart attacks, when troponin isn’t clear.
Imaging and Specialized Tests
Imaging tests are key in diagnosing coronary thrombosis. They show if there’s disease or thrombosis in the coronary arteries. The main imaging tests are:
- Coronary Angiography: The best test for coronary artery disease, it shows the arteries and any blockages.
- Echocardiography: Uses sound waves to check the heart and find problems like ischemia or infarction.
- Cardiac MRI: Gives detailed heart images, helping to see how much damage there is and what might have caused it.
By using these tests together, doctors can accurately diagnose coronary thrombosis. The tests chosen depend on the patient’s symptoms, risk factors, and what resources are available.
Emergency Management of Acute Coronary Thrombosis
Handling acute coronary thrombosis requires a detailed plan to quickly open blocked arteries. This approach is key to reducing heart damage and better patient results.
First Response Protocols
When someone shows signs of acute coronary thrombosis, acting fast is vital. First responders must quickly check the patient’s vital signs and ECG. This helps figure out how bad the blockage is. They then need to get the patient to the cardiac catheterization lab fast.
First responders also give aspirin and other drugs to stop more clots. They watch the patient closely for any signs of getting worse or new problems.
Thrombolytic Therapy Options
Thrombolytic therapy is a key part of treating acute coronary thrombosis. It uses drugs to break up the clot in the artery. This lets blood flow back to the heart muscle.
Choosing the right drug and when to use it is very important. Drugs like alteplase and streptokinase are often used. But, doctors must think carefully before starting this treatment, looking at the patient’s health and any risks.
Interventional Procedures
Interventional procedures are also important in treating acute coronary thrombosis. Primary percutaneous coronary intervention (PCI) is the best choice for some patients. It directly fixes the blocked artery and gets blood flowing again.
During PCI, a stent is placed in the artery to keep it open. This helps the heart muscle get the blood it needs. This method is very good at saving lives and improving health in these patients.
Quick and right action is very important for patients with acute coronary thrombosis. By using first response steps, thrombolytic therapy, and interventional procedures, doctors can give the best care and results.
Pharmacological Treatment Strategies
Managing coronary thrombosis requires a detailed plan. Medications play a key role in stopping new clots from forming. Our goal is to help the heart heal and avoid future heart problems.
Antiplatelet and Anticoagulant Therapies
Antiplatelet and anticoagulant treatments are vital for coronary thrombosis. Antiplatelet agents like aspirin and P2Y12 inhibitors stop platelets from sticking together. This prevents new clots and stops existing ones from growing.
Anticoagulants such as heparin and DOACs like rivaroxaban also help. They block the clotting process. The right choice depends on the patient’s situation and needs.
Supportive Medications
Other drugs support the treatment of coronary thrombosis. Beta-blockers lower heart rate and work less hard. Statins help keep plaques stable and reduce inflammation.
ACE inhibitors and angiotensin receptor blockers (ARBs) control high blood pressure. They help the heart work better and improve patient outcomes. These drugs are part of a complete treatment plan for heart health.
By using these treatments together, we can manage coronary thrombosis well. This reduces the chance of complications and improves patients’ lives.
Surgical Interventions for Severe Cases
Surgery is key for treating severe coronary thrombosis. It’s used when other treatments don’t work or aren’t possible. Surgery helps restore heart health.
Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting, or CABG, is a common surgery for severe heart disease. It uses grafts to bypass blocked arteries. These grafts come from the leg or chest.
This surgery boosts blood flow to the heart. It also lowers the risk of heart attacks. A study on NCBI shows CABG improves survival and reduces the need for more surgeries.
| Benefits of CABG | Considerations |
| Improved blood flow to the heart | Surgical risks and complications |
| Reduced risk of myocardial infarction | Recovery time and rehabilitation |
| Long-term survival benefits | Potential need for future interventions |
Emerging Surgical Approaches
New surgical methods are being developed for coronary thrombosis. These include less invasive surgeries and hybrid procedures. They combine surgery and percutaneous interventions.
Minimally Invasive Surgery Uses smaller cuts and less damage. This means faster recovery times.
Hybrid Revascularization: Mixes CABG with PCI. It’s a complete treatment for complex cases.
These new methods are promising. They might help those who can’t have traditional CABG or PCI.
Recovery and Prognosis After Coronary Thrombosis
Recovering from coronary thrombosis needs a focus on both short-term and long-term care. This ensures the best health outcomes for patients. The recovery path is complex, requiring a detailed plan for immediate and long-term health.
Short-term Recovery Process
The first stage of recovery is key and often happens in a hospital. Immediate care strategies include keeping the patient stable, managing pain, and stopping more clots. It’s vital to:
- Take all medicines as directed, like antiplatelet and anticoagulant drugs.
- Rest and avoid too much activity to protect the heart.
- Watch for any signs of complications or worsening health.
Long-term Outcomes and Survival Rates
The long-term outlook for patients with coronary thrombosis depends on several things. These include heart damage, overall health, and sticking to treatment plans. Long-term management aims to prevent future heart problems and improve survival. Important steps include:
- Making lifestyle changes like eating right, exercising, and quitting smoking.
- Continuing medical treatment for conditions like high blood pressure and high cholesterol.
- Seeing doctors regularly to check on heart health.
| Factor | Impact on Prognosis |
| Extent of Cardiac Damage | Big damage can lead to worse outcomes. |
| Adherence to Treatment | Following treatment closely is linked to better survival. |
| Lifestyle Modifications | Good changes can greatly improve long-term health. |
Knowing what affects recovery and prognosis helps patients and doctors work together. By focusing on both short-term and long-term care, we can boost survival rates and quality of life for those recovering from coronary thrombosis.
Conclusion: Advances in Understanding and Managing Coronary Thrombosis
We’ve seen big steps forward in dealing with coronary thrombosis, a serious heart issue. Better diagnosis and treatment have helped patients a lot. This has made a big difference in their health.
At Liv Hospital, we’re all about top-notch heart care. We use the newest medical tech and treatments. Our team works hard to give patients the best care, from start to finish.
Thanks to a better understanding of coronary thrombosis, we have new ways to manage it. This includes medicines and procedures. By keeping up with these new methods, we help our patients live better lives.
We’re always looking to improve how we handle coronary thrombosis. Our goal is to give our patients the best care and support.
FAQ
What is acute coronary artery thrombus?
Acute coronary artery thrombus is when a blood clot forms in a coronary artery. These arteries carry blood to the heart. This can cause a heart attack by blocking blood flow.
What is coronary thrombosis?
Coronary thrombosis is when a blood clot forms in a coronary artery. It’s a serious issue that can lead to a heart attack by stopping blood flow to the heart.
Is coronary thrombosis a heart attack?
Coronary thrombosis can cause a heart attack. But they’re not the same thing. A heart attack happens when the heart muscle is damaged from a lack of blood flow. This often comes from a coronary thrombosis.
What are the risk factors for coronary thrombosis?
Risk factors include things you can change, like smoking and high blood pressure. High cholesterol, diabetes, and obesity are also risks. Age, family history, and genetics are things you can’t change.
What are the symptoms of coronary thrombosis?
Symptoms include chest pain or discomfort and shortness of breath. You might also feel nausea, fatigue, or pain in the arms, back, neck, jaw, or stomach. Some people don’t show symptoms at all.
How is coronary thrombosis diagnosed?
Doctors first do an emergency assessment. They check for cardiac biomarkers and use imaging like ECG, echocardiogram, and coronary angiography.
What is the treatment for coronary thrombosis?
Treatment includes emergency care with thrombolytic therapy or procedures like angioplasty and stenting. Doctors also use antiplatelet and anticoagulant drugs, along with supportive medications.
Can coronary thrombosis be prevented?
Some risk factors can’t be changed. But managing things you can change can lower your risk. This includes lifestyle changes and medical treatment.
What is the prognosis after coronary thrombosis?
The outcome depends on how severe it is and how quickly and well it’s treated. It also depends on any other health conditions. With good care, many people can recover and live active lives.
What surgical interventions are available for coronary thrombosis?
For severe cases, surgery like coronary artery bypass grafting (CABG) is an option. New surgical methods are also being developed to help restore blood flow to the heart.
How does Liv Hospital manage coronary thrombosis?
Liv Hospital offers full care for coronary thrombosis. This includes emergency treatment, medication, and surgery. We also provide support and guidance during recovery.
References:
- Turner, J., Parsi, M., & Badireddy, M. (2023). Anemia. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499994/





