Acute coronary syndrome (ACS) is a serious condition where blood flow to the heart suddenly drops. This can cause heart attacks and unstable angina. Learn acute coronary heart disease definition, pathophysiology, and management strategies effectively.
ACS covers a range of urgent heart problems. These include STEMI, NSTEMI, and unstable angina. Knowing what ACS is and how it works is key to treating it well.
At Liv Hospital, we focus on top-notch care for ACS. We use the latest methods to help our patients get the best results.
The term acute coronary syndrome covers a range of heart problems. It’s a serious issue that needs quick action.
ACS includes conditions like STEMI, NSTEMI, and unstable angina. Knowing what ACS is helps doctors treat patients fast and right.
ACS has different levels of heart blockage. This leads to various symptoms. At one end, there’s unstable angina, with no heart damage. At the other, STEMI and NSTEMI show heart damage due to blockage.
Telling STEMI, NSTEMI, and unstable angina apart is key. STEMI shows a complete block on the ECG. NSTEMI and unstable angina have similar symptoms but differ in heart damage signs.
ACS is serious because it can lead to big health problems if not treated right away. Knowing the differences helps doctors make better choices for patients. Quick and correct treatment can save lives and prevent serious issues.
It’s key to know about Acute Coronary Syndrome (ACS) to tackle its big health issue worldwide. ACS includes different heart problems like STEMI, NSTEMI, and unstable angina.
ACS is a big problem for health and death around the world. Millions of people get ACS every year. Studies show ACS has a big effect on health care and the economy.
In the U.S., ACS causes a lot of deaths. This shows we need better ways to prevent and treat it.
ACS costs a lot, affecting health care and the economy. These costs include medical bills, lost work time, and care for family members. It’s important to find ways to manage ACS costs.
Health care systems worldwide struggle with ACS. They need to work better to help patients and save money.
ACS hits different people in different ways. Age, gender, and money status play big roles. For example, older people and those with health issues are at higher risk.
Knowing these differences helps us make better plans for prevention and treatment. By focusing on specific groups, we can do better and close care gaps.
Acute coronary syndrome (ACS) happens when coronary arteries get blocked. This blockage leads to heart muscle not getting enough blood. Knowing how this happens helps doctors treat it better.
Atherosclerosis is key in ACS. It’s when plaques grow in coronary arteries. These plaques have lipids, inflammatory cells, and fibrous elements.
These plaques can narrow the artery over time. Factors like hypertension, dyslipidemia, diabetes mellitus, and smoking make them worse.
Plaque rupture and erosion are major causes of ACS. When a plaque bursts, it exposes a lipid core to blood. This leads to a blood clot that can block the artery.
The risk of rupture depends on the plaque’s makeup and its thin fibrous cap. High lipid content, inflammation, and mechanical stress make plaques unstable.
After a plaque bursts, blood clots block the artery. The clot, made of platelets and fibrin, can be big or small. A big clot can cause a ST-elevation myocardial infarction (STEMI). A small clot might cause non-ST-elevation myocardial infarction (NSTEMI) or unstable angina.
When blood flow to the heart stops, the ischemic cascade starts. This includes:
Knowing how ACS works is key to better care. It helps doctors quickly fix the problem and reduce heart damage.
ACS develops from many factors, both changeable and unchangeable. Knowing these factors is key to preventing and managing ACS.
Several changeable risk factors play a big role in ACS. These include:
By changing lifestyles and getting medical help, we can lower ACS risk.
Some risk factors can’t be changed, but knowing them is vital for managing risk.
Knowing these unchangeable risk factors helps in creating personalized prevention and monitoring plans.
It’s key to spot the signs of Acute Coronary Syndrome (ACS) quickly. This is because ACS can range from unstable angina to heart attack. Each needs fast and right care.
Classic angina symptoms are chest pain or discomfort. People often say it feels like pressure or squeezing. This pain can spread to arms, back, neck, jaw, or belly.
Symptoms of ACS include chest pain or discomfort, pain that spreads to other parts of the body, nausea, shortness of breath, and sudden, heavy sweating. These symptoms happen when you exert yourself or get stressed. They usually go away when you rest or take nitroglycerin.
Not everyone shows the usual signs. Some might feel tired, have trouble breathing, or feel their heart beating fast without chest pain. Atypical symptoms are more common in certain groups, like women, older adults, and people with diabetes. Spotting these signs is key to not delaying treatment.
Some groups might show different symptoms or have unique risk factors. For example, women might feel sharp pain in their back, neck, or jaw. Older adults might feel confused, dizzy, or faint. People with diabetes might not feel pain or might have different symptoms because of nerve damage.
Acting fast can help save lives in ACS cases. It’s vital to spot symptoms, whether they’re typical or not, to get help quickly. This can greatly reduce serious problems and death rates.
We use many tools to diagnose ACS accurately and quickly. The diagnosis involves clinical signs, ECG findings, cardiac biomarkers, and sometimes advanced imaging. This approach ensures we get the diagnosis right.
First, we take a detailed medical history and do a physical exam. We look for symptoms like chest pain, shortness of breath, and signs of heart problems. Risk stratification is key to decide what to do next.
We also check for risk factors like high blood pressure, diabetes, and smoking. The type, length, and intensity of chest pain are very important.
The ECG is vital in diagnosing ACS. We look for signs of heart damage, like ST-segment changes or T-wave inversion. ST-elevation myocardial infarction (STEMI) is when there’s ST elevation in two or more leads, showing a blocked artery.
Reading ECGs needs careful thought, as signs can be subtle or mixed with other issues. Sometimes, we need to do serial ECGs to see changes.
Cardiac biomarkers, like troponin, are key in diagnosing heart attacks. High troponin levels mean heart damage, even if the ECG looks normal. We also check other tests, like blood counts and kidney function, to see how the patient is overall.
Other biomarkers, like CK-MB, can help too. But troponin is best because it’s very accurate for heart damage.
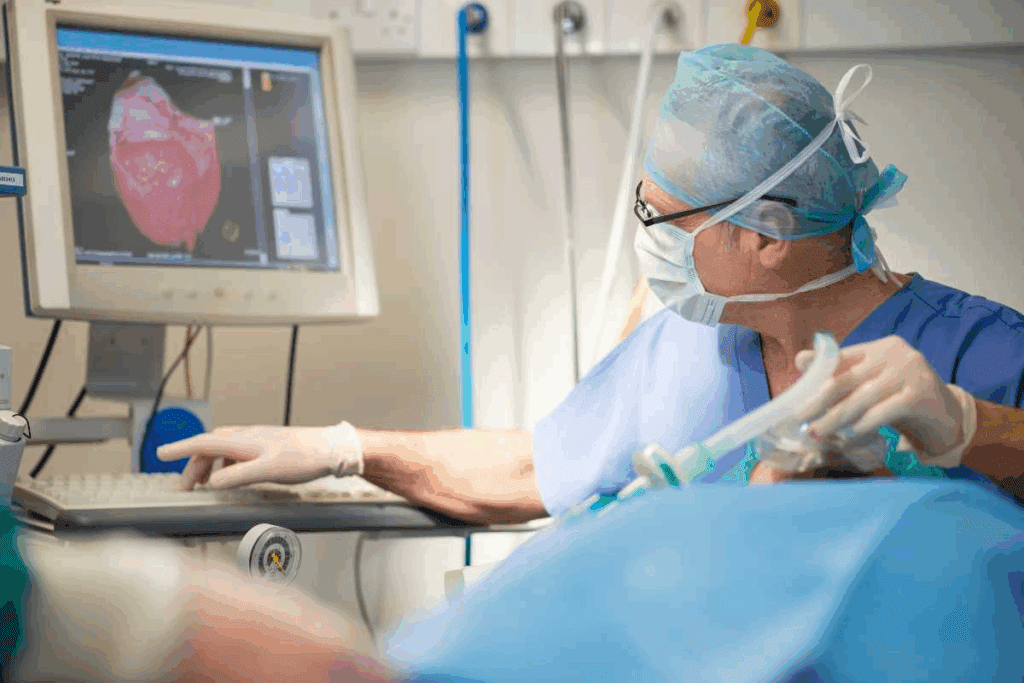
For some patients, we use advanced imaging to check for ACS. Echocardiography looks at heart function, while coronary CT angiography (CCTA) shows artery details. Cardiac MRI checks how well the heart is working and if it’s damaged.
These tests are great for unclear cases or to see how much damage there is. They help us make better treatment plans and improve patient care.
The key to managing ACS is using proven protocols. These include quick actions, medicines, and ways to fix blocked arteries. By sticking to these guidelines, doctors can give patients the best care fast, leading to better results.
When someone with suspected ACS comes in, they need fast help. Doctors give oxygen, aspirin, and nitroglycerin as needed. They also start heart monitoring and take ECGs. Quickly finding and treating ACS cuts down on serious problems and boosts survival chances.
Managing ACS with medicines means using antiplatelets, anticoagulants, beta-blockers, and more. These drugs help lessen heart damage and stop future heart problems. The right medicines depend on the patient’s situation and what doctors recommend. Customizing treatment for each patient is key to the best results.
Fixing blocked arteries is a big part of treating ACS. Doctors might use PCI or CABG. The choice depends on how bad the blockage is, the patient’s health, and the type of blockage. Quickly fixing the blockage can save lives and prevent more heart issues.
Time is very important in treating ACS. Quick action can mean the difference between life and death. It’s important to have systems in place for fast ACS care. This includes quick pre-hospital and emergency room care, and fast access to heart specialists. Working together as a team is essential for giving patients the care they need fast.
Secondary prevention is key to reducing the risk of future cardiovascular events in ACS patients. Effective long-term management involves a multifaceted approach. This includes medication adherence, cardiac rehabilitation, lifestyle modifications, and risk factor management.
Medication adherence is critical for managing ACS long-term. We advise patients to follow their prescribed medication regimen. This usually includes antiplatelet agents, beta-blockers, ACE inhibitors or ARBs, and statins.
Regular follow-up care with healthcare providers is essential. It helps monitor medication adherence and adjust treatment plans as needed. It also manages any side effects.
Table: Common Medications Used in ACS Management
| Medication Class | Examples | Purpose |
| Antiplatelet Agents | Aspirin, Clopidogrel | Prevent platelet aggregation |
| Beta-blockers | Metoprolol, Atenolol | Reduce myocardial oxygen demand |
| ACE Inhibitors or ARBs | Lisinopril, Losartan | Lower blood pressure, reduce strain on the heart |
| Statins | Atorvastatin, Simvastatin | Lower cholesterol levels |
Cardiac rehabilitation is a program that includes exercise, education, and stress counseling. It helps patients recover from ACS events. It also improves their health and reduces the risk of future cardiovascular events.
Lifestyle modifications are vital in preventing ACS. We encourage patients to adopt a heart-healthy lifestyle. This includes a balanced diet, regular physical activity, smoking cessation, and maintaining a healthy weight.
Key Lifestyle Modifications:
Managing and controlling risk factors is essential for preventing ACS recurrence. This includes monitoring and managing conditions like hypertension, hyperlipidemia, and diabetes. We work closely with patients to develop personalized plans to manage these risk factors effectively.
By focusing on secondary prevention and long-term management, we can significantly improve outcomes for ACS patients. Our approach addresses the multifaceted needs of these patients. It enhances their quality of life and reduces the risk of future cardiovascular events.
Understanding ACS and using proven care methods are key to better patient results. New research and education keep improving how we treat ACS. This leads to better care and outcomes for patients.
The future of ACS care depends on more education and sharing knowledge through trusted journals. Healthcare workers need to keep up with new ACS research. This way, they can give the best care and help patients more.
Looking ahead, we must focus on using evidence-based practices. We also need to work together and put patients first. By doing this, we can keep reducing the impact of ACS and help more patients worldwide.
Acute Coronary Syndrome (ACS) is a group of heart conditions. They happen when blood flow to the heart suddenly drops. This includes STEMI, NSTEMI, and unstable angina.
STEMI means a coronary artery is completely blocked. NSTEMI has a partial blockage and some heart muscle damage. Unstable angina has reduced blood flow but no major heart muscle damage.
Risk factors you can change include high blood pressure, high cholesterol, diabetes, smoking, and being overweight. Factors you can’t change include age, family history, and genetics.
Doctors use a few methods to diagnose ACS. They look at your symptoms, do an electrocardiogram (ECG), check for biomarkers, and might use imaging like echocardiography or coronary angiography.
Treatment for ACS includes quick actions like thrombolysis or PCI. Doctors also use medicines like antiplatelets, anticoagulants, and beta-blockers. Lifestyle changes and cardiac rehab are also important.
Secondary prevention helps prevent future heart problems. It includes sticking to your treatment plan, making lifestyle changes, and managing risk factors.
ACS costs a lot for healthcare systems. This includes emergency care, hospital stays, procedures, and ongoing care.
Some groups are at higher risk for ACS. This includes older adults, men, and those with a family history.
Cardiac rehab is key for better outcomes. It offers a structured program of exercise and education. This helps patients recover and live healthier.
Preventing ACS means managing risk factors. This can be done through lifestyle changes and, if needed, medicines. This reduces the chance of getting ACS.
National Center for Biotechnology Information. (2025). What Is Acute Coronary Heart Disease Understanding ACS. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10381786/).
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us