Last Updated on November 26, 2025 by Bilal Hasdemir
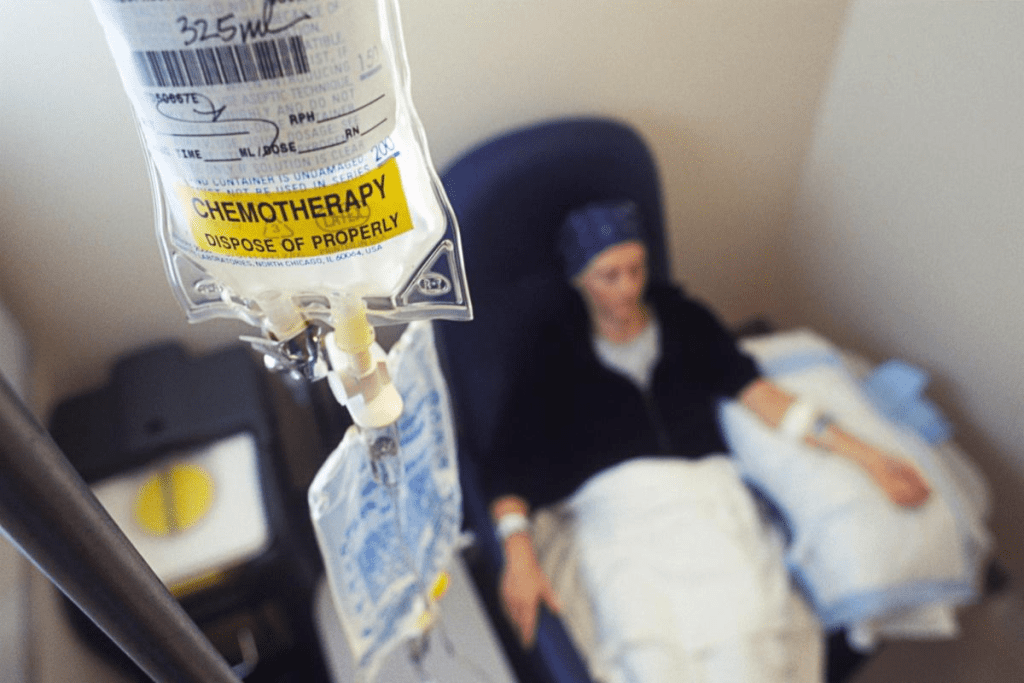
Many cancer patients get adjuvant chemotherapy after surgery. Studies show that when this treatment starts can greatly affect its success. Knowing the best time to start adjuvant chemotherapy is key to getting the most out of it and improving patient results.
Adjuvant chemotherapy is a vital treatment to lower cancer coming back. When it starts can change how long a patient lives. Research has found the best time to start this treatment, and these findings are important for doctors and patients.
Key Takeaways
- The timing of adjuvant chemotherapy can significantly impact treatment outcomes.
- Research is critical in finding the best start time for adjuvant chemotherapy.
- Knowing when to start adjuvant chemotherapy can help patients live longer.
- Adjuvant chemotherapy is a key treatment for many cancers.
- The best time to start adjuvant chemotherapy can differ for each patient.
Understanding Adjuvant Chemotherapy
After the main treatment for cancer, like surgery, adjuvant chemotherapy is key. It helps get rid of any cancer cells left behind. This extra treatment is important to lower the risk of cancer coming back and to help patients do better.
Definition and Purpose
Adjuvant chemotherapy is a treatment given after the main therapy to lower cancer risk. Its main goal is to find and kill tiny cancer cells left after the main treatment. This helps prevent cancer from coming back.
Key aspects of adjuvant chemotherapy include:
- Given after surgery or other main treatments
- Works to get rid of leftover cancer cells
- Helps lower the risk of cancer coming back
- Can also improve survival rates for some cancers
Types of Cancers Requiring Adjuvant Therapy
Adjuvant chemotherapy is used for many types of cancers. Here are a few examples:
| Cancer Type | Common Use of Adjuvant Chemotherapy |
| Breast Cancer | Often used for early-stage breast cancer, mainly when lymph nodes are involved |
| Colon Cancer | Recommended for stage III colon cancer and some stage II cases |
| Lung Cancer | Used in certain non-small cell lung cancer cases after surgery |
Difference Between Adjuvant and Neoadjuvant Chemotherapy
It’s important to know the difference between adjuvant and neoadjuvant chemotherapy. This helps understand how chemotherapy works in cancer treatment.
Adjuvant Chemotherapy: Given after the main treatment (like surgery) to lower cancer recurrence risk.
Neoadjuvant Chemotherapy: Given before the main treatment (usually surgery) to shrink tumors and make them easier to remove.
These treatments have different goals and times. Adjuvant chemotherapy focuses on getting rid of any cancer cells left after surgery. Neoadjuvant chemotherapy aims to make the main treatment more effective by shrinking tumors.
The Critical Role of Adjuvant Chemotherapy Timing
Knowing when to start adjuvant chemotherapy is key to its success. The timing greatly affects how well it works and the patient’s outcome.
Impact on Treatment Efficacy
The timing of adjuvant chemotherapy is very important. Studies show starting it early can lead to better results. It helps lower the chance of cancer coming back.
Starting early has been linked to better survival rates in cancers like breast, colon, and lung. A study in the Journal of Clinical Oncology found that starting within 6 weeks of surgery led to better outcomes.
Relationship Between Timing and Survival Rates
How soon adjuvant chemotherapy starts is closely tied to survival rates. Research indicates that starting too late can harm survival chances.
| Cancer Type | Optimal Timing | Impact on Survival Rates |
| Breast Cancer | Within 6 weeks post-surgery | Improved survival rates with early initiation |
| Colorectal Cancer | Within 8 weeks post-surgery | Reduced survival rates with delayed initiation |
Balancing Urgency and Patient Recovery

While starting early is important, we must also consider the patient’s recovery. Patients need time to heal before starting chemotherapy.
Patient recovery is a big factor in finding the right timing for adjuvant chemotherapy. Doctors must look at the patient’s health, nutrition, and strength before starting treatment.
Standard Guidelines for Adjuvant Chemotherapy Initiation
Guidelines from groups like ASCO and NCCN help doctors decide when to start adjuvant chemotherapy. These rules are made from lots of research and trials. They make sure patients get the best treatment.
ASCO Recommendations
The American Society of Clinical Oncology (ASCO) has detailed guidelines for adjuvant chemotherapy. They focus on the cancer type and stage, and the patient’s health.
NCCN Guidelines
The National Cancer Network (NCCN) also has guidelines for adjuvant chemotherapy. Their guidelines are known for being thorough and relevant to patients.
International Consensus Statements
There are also international statements on starting adjuvant chemotherapy. These come from global experts working together. They aim to make care the same everywhere.
These guidelines stress the need for a team approach to adjuvant chemotherapy. Doctors, surgeons, and others work together. This way, patients get the best care possible.
The “Optimal Window” for Starting Adjuvant Treatment
Research has focused on finding the best time to start adjuvant treatment after surgery. This is key to making treatment more effective.
Adjuvant chemotherapy is vital in cancer treatment. It aims to get rid of any cancer cells left after the main treatment. When to start this treatment is very important for its success.
The 6-Week Benchmark
The 6-week benchmark is often seen as the best time to start adjuvant chemotherapy. It’s when the body has recovered enough from surgery but before cancer can come back.
Waiting too long to start adjuvant chemotherapy can make it less effective. This can also affect how long a patient might live.
Evidence Supporting Early Initiation
Starting adjuvant chemotherapy early is supported by research. It’s believed that early treatment can stop cancer from spreading and improve survival chances.
Many studies have looked at when to start adjuvant chemotherapy and its impact on patients. They found that starting early can lead to better survival rates.
Maximum Time Thresholds
While the 6-week benchmark is common, the best time to start adjuvant chemotherapy can vary. This depends on the cancer type and the patient’s health.
Doctors need to know these time limits to decide when to start adjuvant chemotherapy. They must balance the need for early treatment with the need for recovery after surgery.
Post-Surgical Recovery Period Considerations
Getting better after surgery is key before starting adjuvant chemotherapy. This recovery time has many important parts. Doctors look at these to decide when to start adjuvant treatment.
Wound Healing Requirements
Wound healing is a big deal during recovery. Proper wound healing is important for health and getting ready for adjuvant chemotherapy. If wounds don’t heal right, treatment might be delayed. This could make adjuvant chemotherapy less effective.
Nutritional Status Assessment
Checking the patient’s nutritional status is also very important. Good nutrition helps the body heal from surgery and handle adjuvant chemotherapy. Doctors do nutritional checks to find any gaps and fix them.
Physical Strength Recovery
Getting back physical strength is also a big part. Patients need to be strong enough for adjuvant chemotherapy. This means not just getting back in shape but also managing tiredness and other symptoms.
These factors”wound healing, nutrition, and physical strength”decide when to start adjuvant chemotherapy. Doctors look at all these carefully. They make sure patients are ready for the next part of their treatment.
Factors Affecting Adjuvant Chemotherapy Timing

Knowing what affects when to start adjuvant chemotherapy is key. This decision involves many things about the patient, the tumor, and the treatment. It’s a complex process.
Cancer Type and Stage
The cancer’s type and stage are very important. Different cancers react differently to chemotherapy. The stage of the cancer also plays a big role in when to start treatment.
Table: Cancer Types and Their Sensitivity to Chemotherapy
| Cancer Type | Sensitivity to Chemotherapy | Typical Timing of Adjuvant Chemotherapy |
| Breast Cancer | Moderate to High | Within 6-8 weeks post-surgery |
| Colorectal Cancer | Moderate | Within 8 weeks post-surgery |
| Lung Cancer | High | Within 6 weeks post-surgery |
Surgical Complications
Surgical problems can change when to start adjuvant chemotherapy. Issues like infections or slow healing can delay treatment.
Patient Age and Comorbidities
Age and health problems are also important. Older patients or those with health issues might need chemotherapy adjusted.
- Older patients might not handle chemotherapy as well.
- Health problems can affect when and how to give chemotherapy.
Genetic and Molecular Factors
Genetic and molecular details of the tumor matter too. Some genetic changes might mean starting chemotherapy sooner.
- Tumors with certain genetic changes might need chemotherapy sooner.
- Testing the tumor can show who will benefit most from chemotherapy.
In summary, many things affect when to start adjuvant chemotherapy. These include the cancer, surgery issues, patient health, and genetic details. Understanding these helps make treatment timing better for patients.
Specific Timeframes: 6-Week vs. 8-Week Start Times
When it comes to adjuvant chemotherapy, timing is everything. Studies have looked into starting this treatment at 6 weeks or 8 weeks after surgery. This is to see which time is best for patient results.
Research on the 6-Week Threshold
Starting adjuvant chemotherapy within 6 weeks of surgery is a focus of research. The goal is to kill off any cancer cells early on. This approach has shown to increase survival chances for some cancer patients.
Outcomes with 8-Week Initiation
While 6 weeks is often seen as the best start time, some studies look at 8 weeks. They found that starting at 8 weeks might not hurt survival chances for all patients. But, this can depend on the cancer type and the patient’s health.
| Cancer Type | 6-Week Start Time | 8-Week Start Time |
| Breast Cancer | Improved survival rates | Comparable survival rates |
| Colorectal Cancer | Significant reduction in recurrence | Moderate reduction in recurrence |
| Lung Cancer | Enhanced treatment efficacy | Variable treatment efficacy |
Cancer-Specific Time Sensitivities
Each cancer type reacts differently to when adjuvant chemotherapy starts. Some cancers need treatment sooner, while others might wait a bit longer without losing effectiveness.
It’s key to understand these cancer-specific time sensitivities for personalized treatment plans. Doctors consider the cancer type, stage, and patient health to decide the best start time for adjuvant chemotherapy.
In summary, while 6 weeks is often advised, the best start time can change based on cancer type, stage, and individual patient factors. More research is needed to fully understand how different start times affect patient outcomes.
Cancer-Specific Adjuvant Chemotherapy Timing
The best time to start adjuvant chemotherapy depends on the cancer type. Knowing these differences helps create effective treatment plans. This is key to improving patient outcomes.
Breast Cancer
For breast cancer, chemotherapy is often given after surgery. It helps lower the chance of cancer coming back. Starting chemotherapy within 6 weeks after surgery can improve survival rates and reduce recurrence risk (Early Breast Cancer Trialists’ Collaborative Group, 2019). The choice of chemotherapy depends on the tumor size, grade, and receptor status.
A study in the Journal of Clinical Oncology found that waiting too long to start chemotherapy can harm patients. Waiting more than 12 weeks after surgery can lead to lower survival and disease-free survival rates in early-stage breast cancer (J Clin Oncol, 2018).
Colorectal Cancer
In colorectal cancer, chemotherapy starts within 8 weeks after surgery. The usual treatment includes fluoropyrimidine-based chemotherapy, often with oxaliplatin. Research shows that adjuvant chemotherapy improves survival and lowers recurrence risk in stage III colorectal cancer (André et al., 2015).
| Cancer Stage | Recommended Adjuvant Chemotherapy | Timing |
| Stage III | Fluoropyrimidine + Oxaliplatin | Within 8 weeks post-surgery |
| Stage II (high-risk) | Fluoropyrimidine | Within 8 weeks post-surgery |
Lung Cancer
For non-small cell lung cancer (NSCLC), chemotherapy is recommended after surgery. The best time to start is usually 6 to 8 weeks after surgery. A study in the Journal of Thoracic Oncology showed that adjuvant chemotherapy can improve survival in completely resected NSCLC (Cao et al., 2019).
Starting adjuvant chemotherapy on time is critical for various cancers. Understanding the specific timing for breast, colorectal, and lung cancers helps healthcare providers create better treatment plans. These plans are tailored to meet each patient’s needs.
Patient-Provider Communication About Adjuvant Chemotherapy Timing
Getting the timing right for adjuvant chemotherapy is a team effort. It’s all about talking things over between patients and their doctors. This way, patients know what’s going on and can help decide their treatment.
Discussing the Treatment Timeline
Talking about when treatment should start is key. Doctors need to explain when to start adjuvant chemotherapy. They look at the cancer type, stage, and the patient’s health. Starting treatment 6-8 weeks after surgery can help with some cancers.
- Key factors to discuss:
- The type and stage of cancer
- The patient’s overall health and recovery progress
- The possible benefits and risks of waiting
Addressing Patient Concerns
Patients often worry about their treatment, like when to start adjuvant chemotherapy. Doctors should talk openly and honestly. They should reassure and support patients.
By talking things through, doctors can ease worries and make patients happier. Giving clear info helps patients make good choices about their care.
Shared Decision-Making Process
Shared decision-making means working together to choose treatment. It’s about talking over the good and bad of options. And what the patient wants and values.
- Identify the key decisions to be made
- Discuss the good and bad of each option
- Think about what the patient wants and values
- Make a choice together
By working together, patients and doctors can create a treatment plan that fits the patient’s needs.
Multidisciplinary Approach to Adjuvant Therapy Scheduling
Getting adjuvant therapy to work best needs a team effort from different doctors. This team approach makes sure all parts of a patient’s care are thought about. It helps figure out the best time for adjuvant chemotherapy.
Role of the Tumor Board
A tumor board is key in planning adjuvant therapy. It’s made up of experts from many fields. They come together to:
- Find the best treatment plan.
- Make sure care is coordinated.
- Talk about tough cases.
Tumor boards help make better decisions. They bring together surgeons, medical oncologists, and radiation oncologists. This teamwork makes sure adjuvant chemotherapy starts when it’s most helpful for the patient.
Coordination Between Surgical and Medical Oncology
Working well together is key for adjuvant therapy planning. This means:
| Coordination Aspect | Description | Benefit |
| Pre-operative planning | Talking about surgery and chemotherapy plans before surgery. | Better recovery and fewer problems. |
| Post-operative assessment | Checking how the patient is doing after surgery. | Best time for adjuvant chemotherapy. |
| Ongoing communication | Keeping in touch between surgical and medical oncology teams. | Can change plans if needed. |
This teamwork makes sure the move from surgery to chemotherapy goes smoothly. It helps patients do better.
Patient Advocacy in Treatment Planning
Patient advocacy is very important in planning adjuvant therapy. Advocates make sure:
- Patients’ worries and wishes are heard.
- Patients get all the facts about their options.
- Care plans fit each patient’s needs.
Good patient advocacy leads to care that’s more personal and responsive. It makes the chemotherapy experience better for patients.
Special Populations and Adjuvant Chemotherapy Timing
Special groups, like the elderly and those with serious health issues, face unique challenges with adjuvant chemotherapy timing. They need personalized care to balance treatment benefits and risks.
Elderly Patients
Elderly people often have weaker bodies and are more likely to suffer from chemotherapy side effects. When deciding on chemotherapy timing, their health, any existing conditions, and how well they function are key. Studies suggest that while age doesn’t stop chemotherapy, older patients might do better with a gentler approach to treatment timing.
Patients with Significant Comorbidities
Those with serious health problems, like heart disease or diabetes, need a thorough check before starting chemotherapy. Their health can affect how well they handle chemotherapy, sometimes requiring changes in treatment plans or timing. A team effort is vital, with doctors, primary care physicians, and specialists working together.
Pregnant and Postpartum Women
Pregnant and new moms also need careful thought when it comes to chemotherapy timing. The choice to start chemotherapy during pregnancy must weigh cancer control against risks to the baby. Sometimes, treatment is delayed until after the baby is born, based on the cancer type, stage, and the mom’s health.
Managing chemotherapy in special populations shows the importance of tailored cancer care. By focusing on each patient’s unique needs, healthcare teams can improve treatment results and enhance life quality.
Impact of COVID-19 on Adjuvant Chemotherapy Timing
The COVID-19 pandemic has changed how we treat cancer, including when we give adjuvant chemotherapy. The crisis made it hard to manage cancer care, causing delays in treatment.
Healthcare systems had to adjust to keep patients safe from COVID-19. This meant changing how we treat cancer. Adjuvant chemotherapy, a key part of cancer treatment, was also affected.
Pandemic-Related Delays
The pandemic caused big delays in starting adjuvant chemotherapy. A study in the Journal of Clinical Oncology showed delays of up to 8 weeks or more.
These delays happened for many reasons. Hospitals were busy, patients were scared, and there were logistical problems. Researchers are studying how these delays affect patients.
| Factor | Impact on Adjuvant Chemotherapy Timing | Potential Consequences |
| Hospital Capacity Issues | Delays in treatment initiation | Increased risk of cancer recurrence |
| Patient Fear of Infection | Postponement of treatment | Potential for reduced treatment efficacy |
| Logistical Challenges | Disruptions in supply chains and scheduling | Increased burden on healthcare systems |
Modified Protocols During Healthcare Crises
Healthcare providers made changes to keep patients safe and care going. They used teleconsultations, adjusted schedules, and focused on urgent cases.
- Teleconsultations to reduce hospital visits
- Adjusted treatment schedules to accommodate patient needs
- Prioritization of urgent cases
These changes helped keep cancer care on track, even with the pandemic.
Risk Mitigation Strategies
Healthcare providers used several strategies to manage risks. They quickly assessed patients, used expedited treatment for high-risk ones, and improved communication.
- Rapid assessment and prioritization of patients based on clinical need
- Implementation of expedited treatment pathways for high-risk patients
- Enhanced communication between healthcare teams and patients to manage expectations and coordinate care
These efforts helped reduce the pandemic’s impact on adjuvant chemotherapy timing. They ensured patients got the care they needed.
Conclusion
Choosing the right time for adjuvant chemotherapy is key in cancer treatment. It greatly affects how well a patient does and how long they live. This article looked at what makes the best time to start this treatment.
It talked about the type and stage of cancer, any surgery problems, the patient’s age, and any other health issues. These all play a big role in when to start chemotherapy.
Following guidelines from groups like ASCO and NCCN is very important. Starting treatment within 6-8 weeks after surgery is best. This helps the treatment work better.
Knowing what affects when to start chemotherapy and working together with a team is important. This way, patients get the best care at the right time. It helps make cancer treatment better and more effective.
FAQ
What is adjuvant chemotherapy, and when should it start?
Adjuvant chemotherapy is a treatment given after primary treatments like surgery. It aims to reduce the risk of cancer coming back. The best time to start it varies based on the cancer type and the patient’s health. Usually, it’s recommended to start within 6-8 weeks after surgery.
What is the difference between adjuvant and neoadjuvant chemotherapy?
Adjuvant chemotherapy is given after the main treatment to lower cancer recurrence risk. Neoadjuvant chemotherapy is given before to shrink the tumor.
Why is the timing of adjuvant chemotherapy important?
Starting adjuvant chemotherapy early can greatly improve survival rates in many cancers. The timing is key to its effectiveness.
What are the standard guidelines for initiating adjuvant chemotherapy?
Groups like ASCO and NCCN set guidelines based on clinical trials. These guidelines help ensure patients get timely and effective treatment.
What is the “optimal window” for starting adjuvant chemotherapy?
Starting adjuvant chemotherapy within 6 weeks after surgery is often beneficial. But, the best time can vary based on the cancer and the patient.
What factors affect the timing of adjuvant chemotherapy?
Many factors influence when to start adjuvant chemotherapy. These include the cancer type and stage, any surgery complications, the patient’s age and health, and the tumor’s genetic makeup.
How does the type of cancer affect the timing of adjuvant chemotherapy?
Different cancers have unique needs for adjuvant chemotherapy timing. For example, breast, colorectal, and lung cancers have different start times.
What is the impact of delaying adjuvant chemotherapy?
Delaying adjuvant chemotherapy can harm treatment outcomes and survival rates. The impact depends on the cancer type and the patient’s health.
How does patient-provider communication affect adjuvant chemotherapy timing?
Good communication between patients and healthcare providers is vital. It ensures patients understand their treatment plans and are involved in decisions about adjuvant chemotherapy timing.
What is the role of a multidisciplinary approach in adjuvant therapy scheduling?
A team approach involving different specialties ensures the best care and timing for adjuvant chemotherapy. This includes the tumor board, coordination between teams, and patient advocacy.
How does the COVID-19 pandemic affect adjuvant chemotherapy timing?
The pandemic has caused delays and changes in cancer treatment worldwide. Understanding its impact on adjuvant chemotherapy timing is key for managing patient care during crises.
Are there special considerations for certain patient populations regarding adjuvant chemotherapy timing?
Yes, special populations like elderly patients, those with serious health issues, and pregnant women face unique challenges. Age, health, and pregnancy status must be carefully considered when deciding on adjuvant chemotherapy timing.
References
- Sirohi, B., & Garre, K., et al. (2016). Determining the optimal timing for initiation of adjuvant chemotherapy after resection for stage II and III colon cancer. Journal of Clinical Oncology, 34(6), 576-584. https://pubmed.ncbi.nlm.nih.gov/26734965/