Last Updated on December 2, 2025 by Bilal Hasdemir
Radiation oncology uses radiation as a primary treatment method for cancer.Learn the 4 R’s principles (Repair, Repopulation, Reassortment, Reoxygenation) that guide Advocate radiation oncology treatment.
These plans incorporate radiation therapy along with other treatments, adhering to the guidelines set by the American Society of Radiation Oncology.
We at our institution aim to give top-notch healthcare, supporting patients from around the world. Knowing the 4 R’s helps us give care that’s just right for each patient.
Key Takeaways
- The 4 R’s of radiation therapy are repair, redistribution, repopulation, and reoxygenation.
- Understanding these principles is key for good radiotherapy treatment planning.
- Our team is dedicated to providing personalized care based on these principles.
- The 4 R’s are very important in radiation oncology.
- Good radiation therapy needs a deep understanding of the 4 R’s.
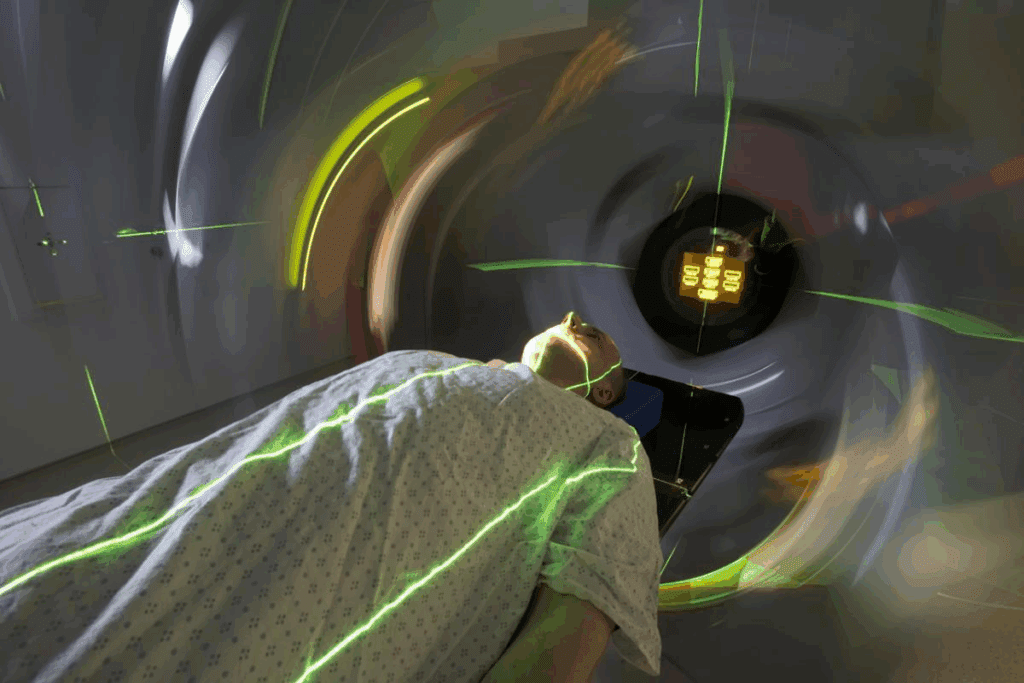
Radiation oncology uses radiation as a primary treatment method for cancer.
Radiation oncology uses radiation as a primary treatment method for cancer. It aims to improve patient outcomes and quality of life. Understanding radiation therapy is essential since it plays a crucial role in cancer treatment.
Definition and Purpose of Radiation Therapy
Radiation therapy uses ionizing radiation to kill cancer cells. Its main goal is to destroy or damage cancer cells. This helps to ease symptoms and increase survival chances. It can be used alone or with other treatments like surgery and chemotherapy.
Types of Radiation Therapy
There are several types of radiation therapy:
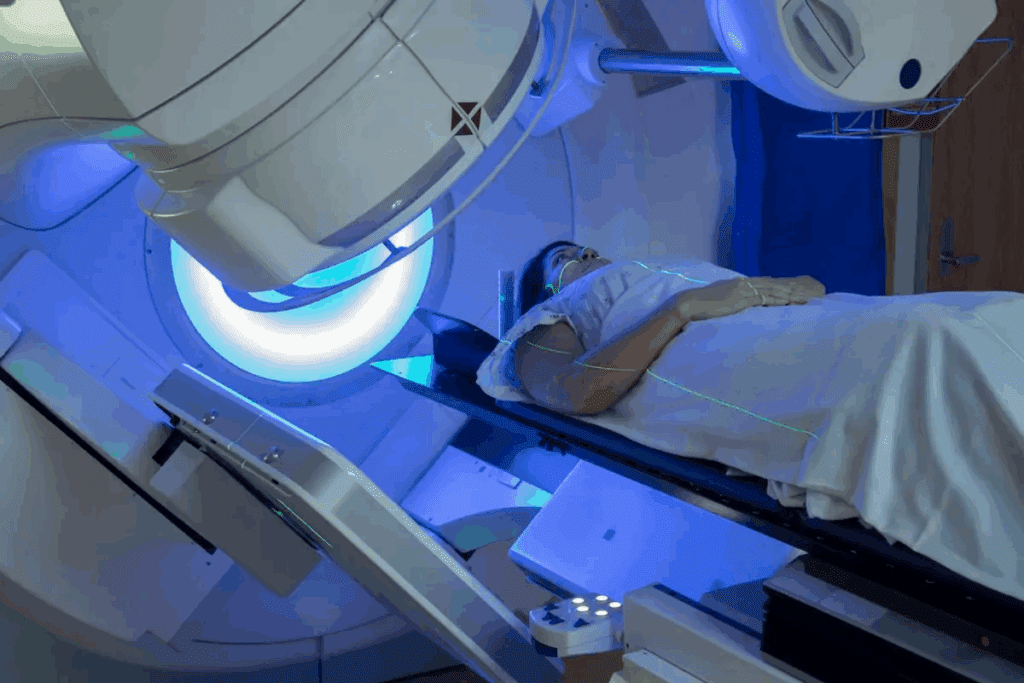
- External Beam Radiation Therapy (EBRT): This type delivers radiation from outside the body.
- Brachytherapy: Places a radioactive source inside or near the tumor.
- Systemic Radiation Therapy: Uses radioactive substances that are swallowed or injected into the body.
We choose the type based on the cancer type, stage, and patient’s health.
Common Conditions Treated with Radiation
Radiation therapy treats many cancers, including:
- Breast cancer
- Prostate cancer
- Lung cancer
- Brain tumors
- Hodgkin and non-Hodgkin lymphoma
Our radiation oncology department has the latest technology. We offer precise radiation treatment planning and follow contour guidelines.
The four R’s significantly influence the effectiveness of radiation therapy.
The four R’s significantly influence the effectiveness of radiation therapy.
Repair of Normal Tissue
Repair is when cells fix DNA damage from radiation. The repair ability of normal tissues varies. This affects how well radiation therapy works and its side effects.
We use systems like Mosaiq radiation oncology. It helps us create treatment plans. These plans aim to fix normal tissues while hitting tumor cells hard.
Reoxygenation of Tumor Cells
Reoxygenation happens as oxygen levels in tumors change during treatment. This affects how well tumor cells respond to radiation. At first, some cells are harder to kill because they lack oxygen. But as treatment goes on, oxygen levels can rise, making these cells more vulnerable.
Our research focuses on ways to boost reoxygenation. This can make treatments more effective.
Redistribution of Cell Cycle
Redistribution is when tumor cells change their cell cycle phases after radiation. As some cells die, others move to different phases. This can change how they react to more radiation.
Understanding this helps us plan radiation therapy better. We can adjust how often we give radiation to get the best results.
Repopulation of Tumor Cells
Repopulation is when tumor cells grow back between treatments. How fast this happens can affect treatment success. If cells grow back quickly, we might need to change the treatment plan to stop the tumor from getting bigger.
We take repopulation into account when making treatment plans. This ensures our patients get the best care possible.
Our ongoing studies are vital to driving innovation and improving patient care.
- Repair: Ability of cells to repair DNA damage.
- Reoxygenation: Changes in tumor oxygen levels affecting radiation sensitivity.
- Redistribution: Changes in cell cycle phases of tumor cells.
- Repopulation: Regeneration of tumor cells between radiation fractions.
The Importance of Each R
The four R’s – repair, reoxygenation, redistribution, and repopulation – are key in radiation therapy. They help make cancer treatments more effective. Understanding these factors is essential.
Impact on Treatment Outcomes
The four R’s significantly influence the effectiveness of radiation therapy. Repair of normal tissue helps reduce side effects. This lets patients recover better.
Reoxygenation of tumor cells makes them more vulnerable to radiation. This boosts the therapy’s success rate.
Redistribution of cell cycle and repopulation of tumor cells are also key. Radiation oncologists use these to plan treatments. This helps improve results.
Enhancing Efficacy of Cancer Therapies
Our radiation oncology department focuses on personalized care. We aim for the best outcomes for our patients. This is like what UVM Radiation Oncology and Baystate Radiation Oncology do.
Understanding the four R’s helps us tailor treatments. This makes cancer therapies more effective. Our team is always learning to offer top-notch care.
Combining the 4 R’s with Other Treatments
By mixing the 4 R’s with chemotherapy and immunotherapy, we can make treatments better. Our team works with other experts to create detailed plans. These plans incorporate radiation therapy along with other treatments, adhering to the guidelines set by the American Society of Radiation Oncology.
Synergy with Chemotherapy
Chemotherapy and radiation therapy work well together. Chemotherapy makes cancer cells more sensitive to radiation, making the treatment more effective. This combo is great for some cancers, leading to better survival rates.
Our radiation oncologists team up with medical oncologists. They figure out the best order and amount of chemotherapy and radiation. This teamwork ensures patients get the best treatment for their needs.
Integration with Immunotherapy
Immunotherapy uses the immune system to fight cancer. Radiation therapy can make immunotherapy work better by releasing tumor antigens. This helps the immune system find and attack cancer cells more easily.
We’re leading the way in combining radiation therapy with immunotherapy. We’re in clinical trials to learn more about this combo. Our aim is to offer the latest treatments that improve patient outcomes and quality of life.
The future of cancer treatment is combining different methods, like radiation therapy, chemotherapy, and immunotherapy. By figuring out how to use these together, we can keep improving treatment results and care for patients.
Radiation oncology uses radiation as a primary treatment method for cancer.
Radiation oncology uses radiation as a primary treatment method for cancer.
Technological Innovations in Radiation Delivery
New technologies have changed radiation therapy for the better. Intensity-Modulated Radiation Therapy (IMRT) shapes beams to fit tumors, protecting healthy tissues. Image-Guided Radiation Therapy (IGRT) and Stereotactic Body Radiation Therapy (SBRT) also improve treatment precision and results.
These new tools have made treatments more effective and less harmful. Our team works hard to keep up with these advancements. We want to give our patients the best care possible.
Personalized Radiation Therapy Approaches
Personalized medicine is changing how we treat cancer. We use genetic tests, advanced imaging, and patient data to create personalized radiation therapy plans. This makes treatments more effective and safer.
This approach is key for complex cancers. It means we can tailor treatments to each patient’s needs. We use the latest tech and knowledge of cancer to make targeted plans.
We’re always looking to improve in radiation oncology. Our goal is to provide top-notch, patient-focused care. We’re committed to using new technologies and personalized methods to better patient outcomes and lives.
Role of the Radiation Oncologist
Radiation oncologists are key in the fight against cancer. They create and carry out treatment plans. We work with patients, giving them care and support every step of the way.
Responsibilities in Patient Care
Radiation oncologists check patients’ conditions and pick the best radiation therapy. We look at the cancer type and stage, and the patient’s health too.
Key responsibilities include:
- Conducting initial consultations to discuss treatment options
- Developing personalized treatment plans
- Overseeing the delivery of radiation therapy
- Monitoring patients’ progress and adjusting treatment plans as necessary
Collaborating with Multidisciplinary Teams
For effective cancer treatment, many medical specialties must work together. We team up with surgeons, medical oncologists, and others for complete care.
| Specialty | Role in Cancer Treatment |
| Surgery | Removing tumors and affected tissues |
| Medical Oncology | Administering chemotherapy and other systemic treatments |
| Radiation Oncology | Delivering radiation therapy to target cancer cells |
Together, we make treatment plans that work best for patients. Our teamwork ensures patients get top-notch care from start to finish.
Our approach is patient-focused, like at OSU Radiation Oncology. We make sure our patients get the best care possible.
Patient Experience in Radiation Therapy
Starting radiation therapy can feel scary, but with the right help, patients can feel more confident. Our radiation oncology departments focus on both physical and emotional care. We aim to support our patients fully.
Preparing for Treatment
Radiation oncology uses radiation as a primary treatment method for cancer.
- Detailed explanations of the treatment process
- Guidance on managing common side effects
- Support in developing a personalized care plan
We also encourage patients to ask questions and share their worries. This open and supportive setting helps patients feel more at ease and confident during their treatment.
Managing Side Effects
Handling side effects is a big part of radiation therapy. Side effects can differ based on the treatment area. Our team offers advice on managing common issues like fatigue, skin reactions, and nausea.
- Fatigue management techniques
- Skin care advice to prevent reactions
- Nutrition guidance to manage nausea and maintain strength
At places like Kent Radiation Oncology and VCU Radiation Oncology, our experts work together to quickly address side effects. This ensures our patients get the best care. By combining radiation therapy with supportive care, we improve the patient experience and treatment results.
In summary, the patient experience in radiation therapy involves careful preparation and managing side effects. Our goal is to provide top-notch healthcare with full support. We want to make sure our patients get the care they need every step of the way.
Research and Future Directions
We are committed to improving radiation oncology through research. We aim to make treatments more effective. Our work includes exploring new technologies and methods to enhance radiation therapy.
Ongoing Studies
Our ongoing studies are vital to driving innovation and improving patient care. We focus on new radiation therapy methods, like combining it with immunotherapy and targeted therapies. Our research is published in top journals like the Journal of Radiation Oncology Biology Physics.
Some of our current research areas include:
- Improving radiation delivery techniques to enhance tumor targeting and reduce side effects
- Exploring the role of radiation therapy in combination with other cancer treatments
- Investigating the use of personalized radiation therapy based on genetic profiling
Future Trends and Innovations
The future of radiation oncology looks bright. New technologies like image-guided radiation therapy and proton therapy will be key. Also, artificial intelligence and machine learning will improve treatment planning and delivery.
| Innovation | Description | Potential Impact |
| Radiation oncology uses radiation as a primary treatment method for cancer. | Real-time imaging during treatment to ensure accurate targeting | Improved tumor control and reduced side effects |
| Proton Therapy | Precision radiation therapy using protons instead of X-rays | Enhanced sparing of healthy tissues and reduced long-term toxicity |
| Artificial Intelligence in Treatment Planning | AI-assisted optimization of radiation therapy plans | More efficient and personalized treatment planning |
We aim to keep advancing in radiation oncology. We will use the latest research and innovations to improve patient outcomes.
Conclusion: Impact of the 4 R’s
Learning about the 4 R’s of radiation therapy is key for treating cancer well. As we move forward in radiation oncology, we’ll see better treatment results.
The 4 R’s – repair of normal tissue, reoxygenation of tumor cells, redistribution of cell cycle, and repopulation of tumor cells – are critical. They help us understand how to fight cancer more effectively. Knowing these concepts helps us see the complexity of cancer treatment and the need for personalized care.
As research grows, we keep up with new discoveries in journals like Radiotherapy and Oncology. This ensures our patients get the top care. The future of radiation therapy looks bright, with new studies and ideas ready to improve treatment and patient results.
FAQ
What are the 4 R’s of radiation therapy?
The 4 R’s are key in radiation therapy. They are Repair, Reoxygenation, Redistribution, and Repopulation. Knowing these helps plan treatment effectively.
The four R’s significantly influence the effectiveness of radiation therapy.
Radiation therapy uses high-energy particles to kill cancer cells. It’s a major part of cancer treatment. Our department has the latest technology for effective treatments.
What is the role of a radiation oncologist?
A radiation oncologist specializes in using radiation to treat cancer. They create treatment plans and work with other doctors for complete care.
How can I prepare for radiation treatment?
Preparing for treatment means understanding the process and managing side effects. Your radiation oncologist will guide you. Our team supports you every step of the way.
What are the benefits of combining radiation therapy with other treatments?
Mixing radiation therapy with other treatments like chemotherapy boosts therapy results. Our team creates detailed plans that include all treatment options.
What is the importance of contour guidelines in radiation therapy?
Contour guidelines are vital for precise treatment planning. They help target the tumor while protecting healthy tissues.
How does Mosaiq radiation oncology system improve treatment outcomes?
Mosaiq makes treatment planning and delivery more efficient. This leads to better treatment results by ensuring accuracy and speed.
What are the latest advances in radiation oncology?
New tech in radiation delivery and personalized therapy are the latest advances. These innovations improve treatment outcomes.
How can I find a radiation oncologist near me?
Search online or ask your doctor for a referral. Our team can also help you find the right radiation oncologist.
What is the impact of radiation oncology research on patient care?
Research is key to improving patient care in radiation oncology. Our department is committed to research and education, publishing in top journals.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/1134278/





