Last Updated on November 25, 2025 by Ugurkan Demir

Atrial fibrillation (AFib) is a common heart condition. It causes an irregular and often fast heart rate. Medications are key in controlling heart rate and rhythm, helping people with AFib live better lives.Discover 9 key AFib drugs that help control heart rate and rhythm for better atrial fibrillation management.
At Liv Hospital, we focus on personalized treatment for AFib. We make sure each person gets care that fits their needs. We’ll look at nine important medications for AFib, including how they work, their benefits, and possible side effects.
Key Takeaways
- AFib is a common type of irregular heart rhythm affecting millions worldwide.
- Medications are key in managing AFib to prevent complications.
- Personalized treatment plans are essential for effective AFib management.
- Lifestyle changes are important in managing AFib.
- Nine key medications are used to control heart rate and rhythm in AFib patients.
Understanding Atrial Fibrillation and Its Impact

Atrial fibrillation is a heart condition where the heart beats irregularly and fast. It needs careful management to avoid serious problems. This condition can lead to stroke, heart failure, and other heart issues.
What Is Atrial Fibrillation?
Atrial fibrillation, or AFib, happens when the heart’s upper chambers beat irregularly. This irregular heartbeat can cause symptoms like heart palpitations and shortness of breath. AFib symptoms can differ from person to person, and some may not show any symptoms at all.
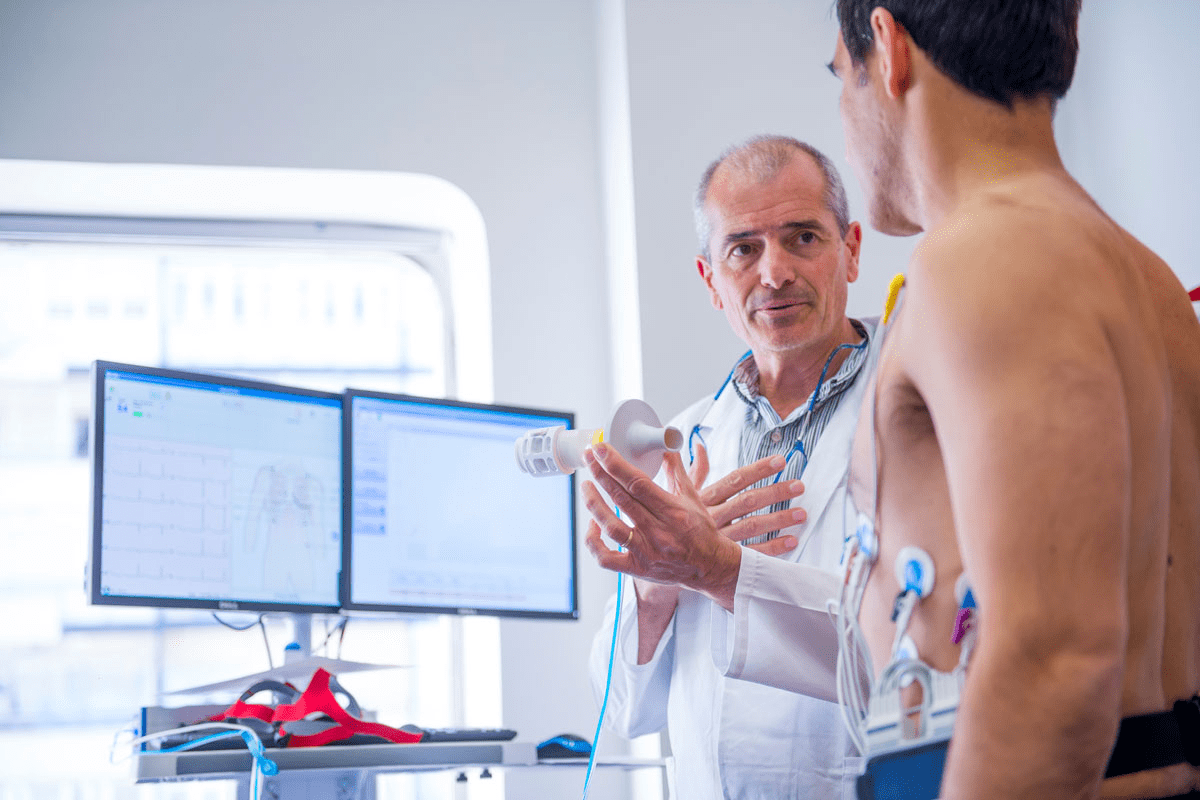
To diagnose AFib, doctors use tests like an electrocardiogram (ECG) and an echocardiogram. These tests help identify the condition and start the right treatment.
Global Prevalence and Health Risks
Atrial fibrillation is a big health issue worldwide. It’s more common as people get older. The risks of stroke and heart failure are higher with AFib. The risk of stroke is a big concern because AFib can cause blood clots in the heart.
As the world’s population ages, more people will get AFib. This will put a strain on healthcare systems everywhere.
The Need for Medication Management
Managing AFib with medication is key to controlling symptoms and preventing complications. Doctors use different medicines to slow the heart rate, restore rhythm, and prevent stroke. The right medicine depends on the person’s health and other conditions.
Managing AFib well requires a team effort. This includes making lifestyle changes, taking medication as directed, and regular check-ups. Understanding AFib helps people manage their condition and lower the risk of serious health problems.
Rate Control vs. Rhythm Control: Two Approaches to Afib Management

Managing Afib can be complex. Doctors often choose between controlling the heart rate or restoring a normal rhythm. The choice depends on symptoms, health, and personal preferences.
The Rate Control Strategy
The rate control strategy slows the heart rate to 60 to 100 beats per minute. It’s often chosen for those with mild symptoms. Rate control medications like beta-blockers and digoxin are used. They improve heart function and reduce symptoms.
The Rhythm Control Strategy
The rhythm control strategy aims to restore a normal rhythm. It’s best for those with severe symptoms or who are young and active. Rhythm control medications like amiodarone are used. They can have side effects and need close monitoring.
How Doctors Decide Between Approaches
Choosing between rate and rhythm control is personal. Doctors look at symptoms, Afib duration, health, and lifestyle. For example, rhythm control might be better for persistent Afib. Rate control could work for paroxysmal Afib. The goal is to find the best balance for each patient.
Essential Afib Drugs: Overview of Medication Categories
Managing AFib often means using different types of drugs. These help control the heart rate, get the rhythm back to normal, and prevent strokes. The right drug depends on the patient’s symptoms, how long they’ve had AFib, and any other health issues.
Rate Control Medications
Rate control drugs slow the heart rate in AFib patients. They aim to lessen symptoms and improve life quality. Here are some common ones:
- Beta-blockers: Great for controlling heart rate, even when you’re active.
- Calcium channel blockers: Good for those who can’t take beta-blockers.
- Digoxin: Often used in heart failure patients or those who don’t move much.
Rhythm Control Medications
Rhythm control drugs try to get the heart back to a normal rhythm. They’re for patients who keep feeling symptoms even with rate control drugs. Or if there’s a reason for AFib that can be fixed.
- Antiarrhythmic drugs: Like amiodarone, flecainide, and sotalol, help keep the rhythm normal.
- Role of rhythm control: It can make symptoms better and improve life quality for some patients.
Anticoagulants and Their Role
Anticoagulants are key to preventing strokes and blood clots in AFib patients. They stop blood clots from forming.
- Warfarin: A traditional anticoagulant that needs regular blood tests.
- Direct Oral Anticoagulants (DOACs): Dabigatran, rivaroxaban, apixaban, and edoxaban are easier to take than warfarin.
First-Line vs. Second-Line Treatments
Choosing between first-line and second-line treatments depends on how well the patient responds to the first drug. It also depends on side effects and the patient’s specific needs.
| Treatment Line | Medication Category | Examples |
| First-Line | Rate Control | Beta-blockers, Calcium channel blockers |
| First-Line | Anticoagulants | DOACs (e.g., apixaban), Warfarin |
| Second-Line | Rhythm Control | Amiodarone, Flecainide |
In conclusion, treating AFib requires a mix of different drugs. Knowing how rate control, rhythm control, and anticoagulants work is key to effective treatment.
Beta-Blockers for Rate Control in Atrial Fibrillation
Beta-blockers are key in managing atrial fibrillation, focusing on heart rate control. They reduce heart rate, improving heart function and easing AFib symptoms.
Metoprolol: Mechanism and Usage
Metoprolol is a top choice for AFib treatment. It blocks beta-1 receptors in the heart, lowering heart rate and contraction force. This helps control the ventricular rate in AFib patients.
Metoprolol comes in immediate-release and extended-release tablets. The choice depends on the patient’s needs and the doctor’s advice.
Atenolol: Benefits and Considerations
Atenolol is used for rate control in AFib. It’s given once a day, making it easier for patients to stick to their treatment. Atenolol is usually well-tolerated but needs careful use in patients with kidney issues.
Atenolol is effective in lowering heart rate and has fewer side effects than some other beta-blockers.
Bisoprolol and Carvedilol: Alternative Options
Bisoprolol and carvedilol are other beta-blockers for AFib rate control. Bisoprolol is great for patients with breathing problems due to its high beta-1 selectivity. Carvedilol has beta-blocking and alpha-blocking effects, benefiting some patients more.
These options give doctors more choices for treating patients, tailoring therapy to each individual’s needs.
Side Effects and Precautions
Beta-blockers are usually safe but can cause side effects like fatigue, dizziness, and shortness of breath. Patients with asthma or severe COPD should use them with caution or avoid them.
It’s important to monitor heart rate, blood pressure, and symptoms closely. This helps manage side effects and adjust treatment as needed.
Calcium Channel Blockers as Heart Rate Control Medication
Calcium channel blockers are key in managing heart rate for atrial fibrillation (AFib) patients. They block calcium ions in heart and blood vessels. This action lowers heart rate and strength, helping control AFib.
Diltiazem: How It Works for Afib
Diltiazem is a common calcium channel blocker for AFib. It comes in oral and intravenous forms, fitting various needs. It slows heart rate by affecting the AV node, easing AFib symptoms.
The oral form is for long-term use, while the intravenous form is for quick heart rate control. Its effectiveness and safety make it a top choice for doctors.
Verapamil: Applications and Dosing
Verapamil is another calcium channel blocker for AFib. It’s great for controlling heart rate, often chosen when diltiazem isn’t an option. It comes in immediate and extended-release tablets for flexible dosing.
It’s important to watch for side effects like constipation and low blood pressure. The dose of verapamil should be tailored to each patient’s needs.
Comparing Effectiveness with Beta-Blockers
Calcium channel blockers and beta-blockers both control heart rate in AFib. But they act differently and have different side effects. Calcium channel blockers like diltiazem and verapamil are better for some patients, like those with COPD.
The choice between these medications depends on the patient’s health, how well they tolerate drugs, and their specific situation.
Common Side Effects and Contraindications
Calcium channel blockers are usually safe but can cause side effects. Common issues include swelling, dizziness, and headaches. Serious problems include severe low blood pressure and certain heart blocks.
Healthcare providers must carefully check patients before starting these drugs. Regular monitoring is key to safe and effective treatment of AFib.
Digoxin: Traditional Medicine for Atrial Fibrillation
Digoxin has been used for centuries to treat heart conditions, including atrial fibrillation (AFib). It’s a cardiac glycoside that helps manage AFib, focusing on controlling the heart rate.
Mechanism of Action in Afib
Digoxin boosts the strength of heart contractions and slows the heart rate. It does this by blocking the sodium-potassium ATPase pump. This action increases vagal tone and reduces AV node conduction. It’s great for controlling the ventricular rate in AFib patients.
Key benefits of digoxin include:
- Effective heart rate control
- Improved cardiac output
- Potential reduction in symptoms
When Digoxin Is Prescribed
Digoxin is often given to AFib patients, mainly those with heart failure or instability. It’s a good choice for those not responding to other treatments. It’s a valuable option for managing AFib in specific cases.
Specific scenarios where digoxin may be preferred include:
- Patients with heart failure
- Those who are sedentary or have limited physical activity
- Patients with contraindications to other rate-control medications
Monitoring and Safety Considerations
Digoxin is effective for AFib but needs careful monitoring. We watch serum digoxin levels, renal function, and electrolytes like potassium and magnesium. Regular follow-ups are key to avoid toxicity.
Safety considerations include:
| Monitoring Parameter | Importance |
| Serum Digoxin Levels | Ensures therapeutic range (0.8-2.0 ng/mL) |
| Renal Function | Digoxin is excreted by the kidneys; impaired function can lead to toxicity |
| Electrolyte Levels | Hypokalemia and hypomagnesemia increase the risk of toxicity |
Understanding digoxin’s role in AFib management helps us offer safe and effective treatment to our patients.
Antiarrhythmic Medications for Maintaining Normal Rhythm
Antiarrhythmic medications are key in treating atrial fibrillation. They help keep the heart beating normally. Each medication works differently and is chosen based on the patient’s needs.
Amiodarone: Powerful but Complex
Amiodarone is very effective in treating atrial fibrillation. But, it has complex effects and can cause serious side effects. It’s very good at stopping arrhythmias from coming back, but it can harm the thyroid and lungs.
Flecainide: Uses and Limitations
Flecainide is good for people with healthy hearts. It slows down heart signals. It’s great for keeping the heart rhythm normal, but it’s not for everyone. It’s not safe for those with heart disease or heart failure.
Sotalol: Dual Action Properties
Sotalol does two things: blocks beta receptors and fights arrhythmias. It’s very helpful for patients needing both treatments. But, it can make the heart’s electrical system unstable, leading to dangerous arrhythmias.
Propafenone and Dronedarone: Additional Options
Propafenone is good for keeping the heart rhythm normal. Dronedarone is like amiodarone but safer. Propafenone works well for rhythm control, and dronedarone is safer but less effective.
In summary, antiarrhythmic medications are vital for treating atrial fibrillation. They offer many options for keeping the heart rhythm normal. Choosing the right medication is important. It depends on the patient’s health and how they might react to the medication.
Managing Afib with RVR: Emergency Medications and Protocols
Atrial fibrillation with rapid ventricular response (RVR) is a serious condition that needs immediate medical attention. It happens when the heart’s upper chambers beat irregularly and very fast. This can be life-threatening if not treated quickly.
What Is Rapid Ventricular Response?
Rapid ventricular response (RVR) is a complication of atrial fibrillation. It’s when the heart rate goes over 100 beats per minute. Symptoms include palpitations, shortness of breath, and chest discomfort. Knowing about RVR is key for healthcare providers to give the right care.
RVR is not just a high heart rate; it can lead to serious heart problems if not treated fast. The irregular heart rhythm of Afib and RVR raises the risk of stroke, heart failure, and other heart issues.
Intravenous Medications for Acute Management
In emergency situations, intravenous (IV) medications are used to control heart rate and convert Afib with RVR to a normal rhythm. Beta-blockers and calcium channel blockers are common IV medications for this purpose.
- Beta-blockers like metoprolol and esmolol are effective in rapidly controlling heart rate.
- Calcium channel blockers such as diltiazem are also used for their ability to slow the heart rate without significantly depressing myocardial contractility.
Transitioning from Hospital to Home Treatment
After managing Afib with RVR in the hospital, transitioning to home treatment is important. Patients are usually switched from IV medications to oral forms to manage their condition at home.
We stress the need for patient education on medication adherence, lifestyle changes, and recognizing symptoms that need immediate medical attention. Effective transition to home care is key to preventing readmissions and improving patient outcomes.
Understanding the causes of RVR, the medications used to treat it, and the protocols for transitioning from hospital to home care helps healthcare providers give complete care to patients with Afib and RVR.
Personalized Afib Drug Treatment: Selection Factors
Personalized medicine is changing how we treat Atrial Fibrillation. It tailors treatment to each patient’s needs. The right medication is key to managing AFib, based on each patient’s health.
Patient-Specific Factors in Medication Selection
Choosing the right medication for AFib involves looking at several factors. We consider the patient’s medical history, any comorbid conditions, and their current health. Understanding these factors helps us predict how a patient will respond to a particular medication and minimizes the risk of adverse effects.
Comorbidities and Their Impact on Drug Choice
Comorbidities are important in picking the right AFib medication. For example, patients with heart failure need medications that won’t make their condition worse. Beta-blockers, for example, are often used in patients with heart failure as they can help improve heart function. But, certain antiarrhythmic drugs may not be safe for patients with specific comorbidities.
Age and Gender Considerations
Age and gender are also key in choosing AFib medication. Older patients may metabolize drugs differently and may be more susceptible to side effects. Gender differences can also affect how well a drug works and how safe it is. For example, some studies suggest that women may be at a higher risk of certain side effects from AFib medications.
Lifestyle Factors Affecting Medication Efficacy
Lifestyle factors, like diet, exercise, and smoking status, can greatly affect how well AFib medications work. Patients who lead a healthier lifestyle may require different medication strategies compared to those with less healthy habits. For instance, patients who are physically active may need to adjust their medication dosage or type to accommodate their lifestyle.
By taking these factors into account, we can create a treatment plan that not only manages AFib but also improves the patient’s quality of life. The goal is to find the right balance between the benefits and risks of different medications, tailored to each patient’s needs.
- Patient-specific factors influence AFib medication choice.
- Comorbidities significantly impact drug selection.
- Age and gender considerations are critical in treatment planning.
- Lifestyle factors affect medication efficacy and safety.
Balancing Benefits and Risks: Side Effect Management
Managing Afib well means finding the right balance between the good and bad of medication. Atrial fibrillation treatment often includes many medications, each with its own side effects and interactions. Knowing these details is key to getting the best results and avoiding bad effects.
Common Side Effects Across Afib Medications
Afib meds can cause many side effects, some common to many drugs. For example, beta-blockers and calcium channel blockers can make you tired, dizzy, and short of breath. Antiarrhythmic drugs might cause stomach problems, tremors, and in rare cases, make arrhythmias worse. It’s important to watch for these side effects and adjust treatment as needed.
Monitoring Requirements for Different Drugs
Each Afib medication needs different monitoring to ensure safety. For instance, amiodarone patients need regular thyroid and liver tests, and chest X-rays because of its risk of lung problems. Patients on warfarin must have their INR checked often to avoid blood clots and bleeding. Seeing your healthcare provider regularly is vital for adjusting doses and switching meds when needed.
When to Consider Medication Changes
Changing Afib meds is usually based on how bad the side effects are, how well the current treatment works, and any health changes. If side effects are severe or the treatment isn’t working, a change might be needed. Also, if new health issues arise or kidney or liver function changes, a medication switch might be necessary. Working closely with your healthcare provider is important for making the right treatment changes.
Drug Interactions to Be Aware Of
Afib meds can interact with other drugs, leading to bad effects or reduced effectiveness. For example, some antiarrhythmic drugs can increase bleeding risk when taken with blood thinners. Also, rate control meds can interact with drugs that affect heart rate or blood pressure. Telling your healthcare provider about all your medications and supplements is critical to avoid drug interactions.
By understanding the side effects, monitoring needs, and drug interactions of Afib meds, healthcare providers and patients can work together to improve treatment plans and outcomes.
Conclusion: Effective Long-Term Management of Atrial Fibrillation
We’ve looked at many ways to manage Atrial Fibrillation (AFib). This includes understanding the condition, different medications, and lifestyle changes. Managing AFib well over time means using a mix of treatments, lifestyle changes, and regular checks.
Working with doctors, following treatment plans, and choosing a healthy lifestyle can help people with AFib live well. This approach is key for managing AFib and caring for it in the long run. It helps patients feel better and lowers the chance of serious problems.
Changing your lifestyle is important for managing AFib. Eating right, staying active, and handling stress well can improve your health. Taking your medicine as directed is also critical. It helps control your heart’s rhythm and lowers the risk of stroke and other serious issues.
By combining medical treatment with lifestyle changes, people with AFib can get better health results. We stress the need for ongoing care and monitoring. This ensures that each person’s AFib management plan is made just for them, helping them stay healthy in the long run.
FAQ
What are the primary goals of AFib medication management?
The main goals are to control the heart rate and rhythm. They also aim to prevent stroke and other complications.
What is the difference between rate control and rhythm control strategies in AFib management?
Rate control slows the heart rate to normal. Rhythm control tries to restore a normal rhythm.
What are the most commonly used medications for rate control in AFib?
Beta-blockers like metoprolol and atenolol are used. Calcium channel blockers, such as diltiazem and verapamil, are also common.
What are antiarrhythmic medications used for in AFib management?
Antiarrhythmic drugs, like amiodarone, flecainide, and sotalol, help keep the rhythm normal in AFib patients.
What is the role of anticoagulants in AFib management?
Anticoagulants are key in preventing stroke. They reduce the risk of blood clots in AFib patients.
How is digoxin used in AFib management?
Digoxin helps control heart rate and improve output in AFib patients, mainly those with heart failure.
What are the possible side effects of AFib medications?
Side effects can include fatigue, dizziness, and stomach issues. The specific side effects vary by medication.
How are AFib medications monitored and adjusted?
Medications are checked regularly through check-ups, electrocardiograms, and blood tests. Adjustments are made as needed to manage side effects and ensure effectiveness.
What lifestyle modifications can help manage AFib?
Maintaining a healthy weight, exercising, and managing stress can help manage symptoms and improve health.
How do comorbidities impact AFib medication choice?
Conditions like heart failure, diabetes, and kidney disease affect medication choice. Healthcare providers must consider these when planning treatment.
What are the signs that AFib medication needs to be changed?
Signs include persistent or worsening symptoms, significant side effects, or if heart rate or rhythm control is not achieved.
How do drug interactions affect AFib medication?
Interactions can impact how well and safely the medication works. Healthcare providers must be aware of these when prescribing multiple drugs.
References:
- Mahfoud, F., et al. (2024). The current position of β-blockers in hypertension. Current Medical Research and Opinion, 40(3), 311-318. https://www.tandfonline.com/doi/full/10.1080/03007995.2024.2318003