Last Updated on November 26, 2025 by Bilal Hasdemir
Colorectal cancer is a big problem for men all over the world. It gets worse as men get older. 1 in 23 men will develop colon cancer in their lifetime. This makes it a serious health issue. Knowing the right age for colonoscopy is a powerful, life-saving decision. This ultimate guide provides the amazing new guidelines you must know.
Men should get a colonoscopy to check for cancer early. This test looks for polyps in the colon. These can be removed before they turn into cancer.
Knowing when to get a colonoscopy is key to staying healthy. It helps find cancer early. This can lead to better treatment and more chances of living longer.
Key Takeaways
- Men should consider colonoscopy as a vital screening tool for colorectal cancer.
- The risk of colorectal cancer increases with age, making screening after 50 important.
- Colonoscopy can detect and remove polyps before they become cancerous.
- Early detection significantly improves treatment outcomes and survival rates.
- Discussing the right colon cancer screening age with a healthcare provider is essential.
Understanding Colonoscopy: A Vital Screening Tool
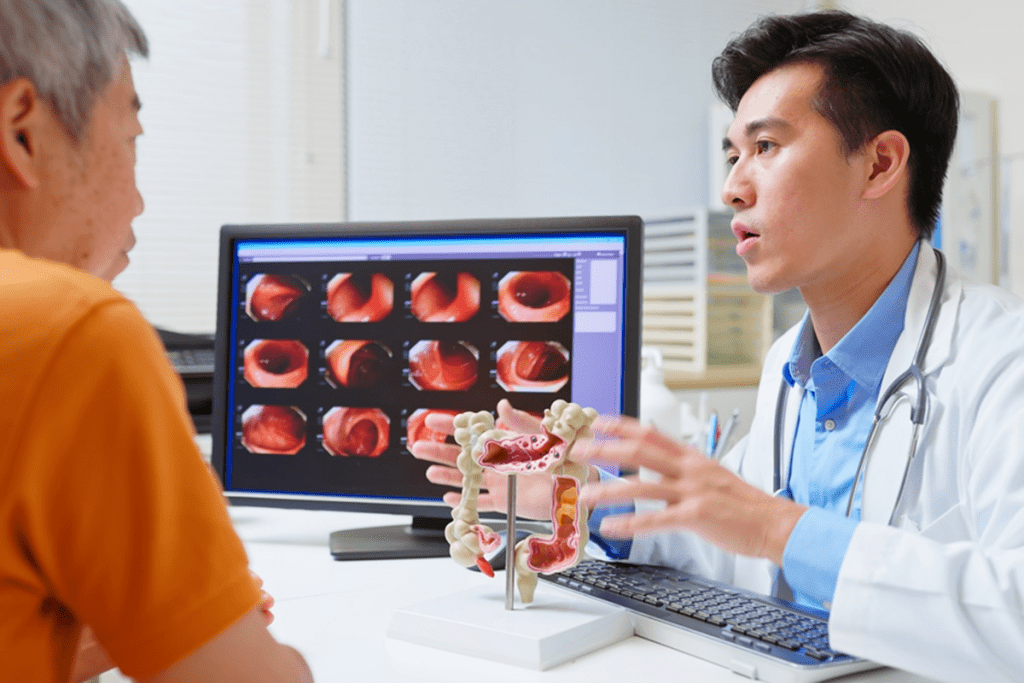
A colonoscopy is more than a medical test; it’s key for catching colorectal cancer early. We’ll look at its importance for men’s health and how it helps prevent colorectal cancer.
What is a colonoscopy?
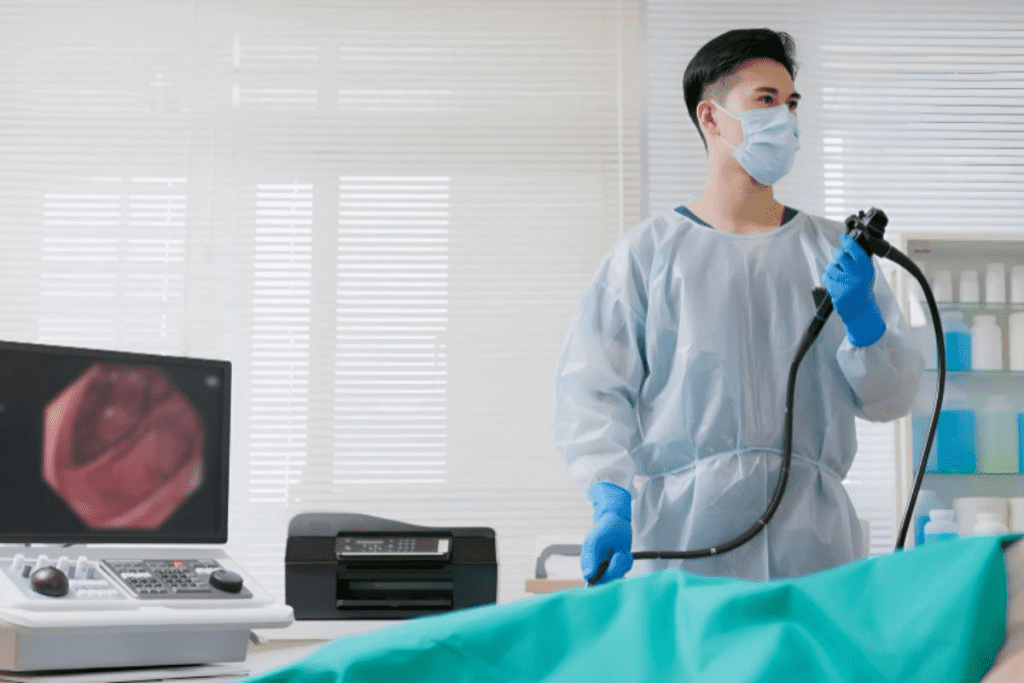
A colonoscopy lets doctors see inside the colon and rectum. They use a flexible tube with a camera, called a colonoscope. This helps find polyps, cancer, and other issues in the colon.
Why colonoscopies are important for men’s health
Colonoscopies are vital for men’s health. They let doctors see the colon and rectum directly. This is key for men at risk of colorectal cancer, as it catches and removes polyps early.
The role of colonoscopies in preventing colorectal cancer
The American Cancer Society says colonoscopy is a top screening for colorectal cancer. It finds and removes polyps, stopping cancer before it starts. This is key in cutting down colorectal cancer cases and deaths.
| Benefit | Description | Statistic |
| Early Detection | Identifies polyps and cancer early | Colonoscopy can reduce colorectal cancer mortality by up to 60% (Source: American Cancer Society) |
| Prevention | Removes polyps before they become cancerous | Regular colonoscopies can prevent up to 90% of colorectal cancers (Source: National Cancer Institute) |
| Risk Reduction | Reduces risk of developing colorectal cancer | Men who undergo regular screening have a significantly lower risk of dying from colorectal cancer |
In conclusion, colonoscopy is a critical tool for men’s health. It’s key in preventing and catching colorectal cancer early. By knowing what colonoscopy is and its benefits, men can stay healthy.
The Recommended Age for Colonoscopy in Men
Knowing when a man should have his first colonoscopy is key to catching colorectal cancer early. The rules for this have changed, thanks to new studies and insights into men’s health.
Standard Guidelines for First-Time Screening
The US Preventive Services Task Force says adults should start screening at 45 if they’re at average risk. This advice is for both men and women, based on a lot of research.
When a man should get his first colonoscopy depends on his family history, lifestyle, and health. Early screening is key to preventing colorectal cancer, as it catches and removes polyps before they turn cancerous.
How Men’s Risk Factors Differ from Women’s
Men face different risks for colorectal cancer than women. For example, men are more likely to get it as they get older. Lifestyle choices, like diet and smoking, also affect a person’s risk.
- Diet: Eating a lot of red and processed meats can raise your risk.
- Smoking: It’s a big risk factor for many cancers, including colorectal cancer.
- Family History: Having a family history of colorectal cancer or polyps increases your risk.
Recent Changes in Screening Age Recommendations
Guidelines have changed, now saying men should start screening at 45 instead of 50. This change comes from evidence that screening earlier can help prevent and treat colorectal cancer better.
A gastroenterologist, says,
“The shift to earlier screening ages acknowledges the rising incidence of colorectal cancer in younger populations and the importance of early detection.”
By knowing these guidelines and risk factors, men can make better health choices. They can take steps to prevent colorectal cancer.
Current Medical Guidelines for Colonoscopy Screening
Many medical groups have set guidelines for colonoscopy screening. This is key for men to prevent health issues. Knowing these guidelines helps men plan their screenings wisely.
American Cancer Society Recommendations
The American Cancer Society (ACS) says adults should start screening at 45 if they’re at average risk. They suggest a stool test every year or a colonoscopy every 10 years. If you have a family history or other risk factors, you might need to screen more often.
U.S. Preventive Services Task Force Guidelines
The U.S. Preventive Services Task Force (USPSTF) advises screening for colorectal cancer in those aged 50 to 75. They recommend several tests, including colonoscopy every 10 years. For those 45 to 49, they suggest screening too, but it’s not as strongly recommended.
American College of Gastroenterology Guidelines
The American College of Gastroenterology (ACG) says African Americans and those with a family history of colorectal cancer should start screening at 45. For others, they recommend starting at 50.
Differences in Guidelines for Men
Guidelines vary slightly, but they all aim to help men stay healthy. The ACS starts screening at 45, while the USPSTF focuses on 50 to 75. It’s best to talk to your doctor to figure out the right schedule for you.
Key Considerations:
- Family history of colorectal cancer
- Personal history of polyps or inflammatory bowel disease
- Genetic syndromes that increase risk
- Racial and ethnic background
By understanding these guidelines and talking to your doctor, men can make smart choices about their colonoscopy screenings.
Risk Factors That May Lower the Age for Colonoscopy
Knowing the risk factors for an early colonoscopy is key for men’s health. General guidelines are a starting point. But, individual situations can change the recommended age for screening.
Family History of Colorectal Cancer
A family history of colorectal cancer can mean an earlier colonoscopy. Men with a first-degree relative (parent, sibling, or child) diagnosed with colorectal cancer face a higher risk. If the relative was diagnosed before age 60, the risk is even greater.
Men with a family history of colorectal cancer should talk to their doctor about when to start screening. Usually, screening starts 10 years before the relative’s diagnosis.
Personal History of Polyps or Inflammatory Bowel Disease
Men with a history of colorectal polyps or inflammatory bowel disease (IBD) are at higher risk. This risk is higher for those with multiple or large polyps, or a history of dysplasia.
Surveillance colonoscopy is often recommended for these individuals. The frequency depends on previous colonoscopy findings and the severity of their condition.
Genetic Syndromes That Increase Risk
Certain genetic syndromes can greatly increase the risk of colorectal cancer. These include:
- Lynch syndrome (also known as hereditary nonpolyposis colorectal cancer or HNPCC)
- Familial adenomatous polyposis (FAP)
- Other rare syndromes such as Peutz-Jeghers syndrome and juvenile polyposis syndrome
Men with known or suspected genetic syndromes should get genetic counseling. They may need to start colonoscopy screening in their teens.
Racial and Ethnic Risk Factors for Men
Racial and ethnic background can affect colorectal cancer risk. African American men, for example, have a higher incidence of colorectal cancer. They are also more likely to be diagnosed at a younger age compared to other racial groups.
| Racial/Ethnic Group | Relative Risk Compared to Non-Hispanic Whites | Recommended Age for First Colonoscopy |
| African Americans | Higher risk | 45 years old |
| Non-Hispanic Whites | Baseline risk | 50 years old |
| Ashkenazi Jews | Higher risk due to genetic syndromes | 40-50 years old, depending on family history |
It’s important for men to talk to their healthcare provider about their risk factors. This will help determine the best screening schedule for them.
Signs and Symptoms That Warrant Earlier Screening
It’s important to know when you might need a colonoscopy sooner than usual. Routine screenings are key for staying healthy. But, some symptoms mean you should see a doctor right away.
Rectal Bleeding and Other Warning Signs
Rectal bleeding is a common sign of colorectal cancer. If you see blood in your stool or from your rectum, see a doctor fast. Also, watch for persistent abdominal pain, weakness, or feeling like you can’t fully empty your bowels.
Changes in Bowel Habits
Changes in how often you go to the bathroom can be a sign. If you have diarrhea or constipation that lasts, talk to your doctor.
Unexplained Weight Loss and Fatigue
Unexplained weight loss and constant tiredness can mean many things, including cancer. If you’re losing weight or feeling very tired without a reason, get checked by a doctor.
When Symptoms Should Prompt Immediate Medical Attention
Severe symptoms like severe abdominal pain, vomiting blood, or passing black tarry stools need urgent care. These could be signs of a serious problem that needs quick treatment.
How Often Should Men Get a Colonoscopy?
Knowing when to get a colonoscopy is key for men’s health. The timing depends on your risk and past results.
Standard Intervals for Average-Risk Individuals
Men at low risk should get a colonoscopy every 10 years starting at 45. But, guidelines can change slightly.
The American Cancer Society says men without risk factors can stick to the 10-year rule. Talk to your doctor about your health history to set the right schedule.
Modified Schedules for High-Risk Men
Those at higher risk need more checks. This includes family history, past polyps, or certain genetic conditions.
For example, men with a family history of early colon cancer should start screening at 40. Or 10 years before their relative’s diagnosis, whichever is sooner. They might need a colonoscopy every 5 years or more, based on their risk.
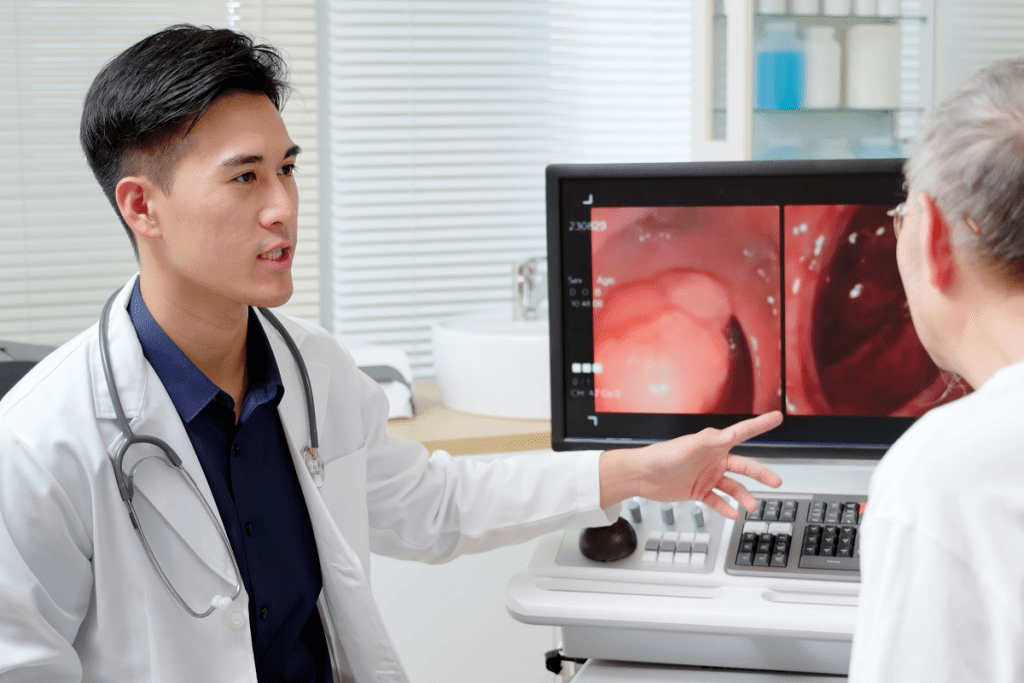
Follow-up Colonoscopies After Polyp Removal
After finding polyps, your next screenings will depend on the polyps’ size and type.
| Polyp Characteristics | Recommended Follow-up Interval |
| 1-2 small ( | 5-10 years |
| 3-4 tubular adenomas or 1 ≥10 mm | 3 years |
| 5 or more adenomas or serrated polyposis syndrome | 1-3 years |
Surveillance Recommendations Based on Findings
Your first colonoscopy’s results affect future screenings. Men with a history of cancer or high-risk polyps need closer checks.
“Surveillance colonoscopy is key for catching new problems in those with a history of colon cancer or high-risk polyps.”
” American Society for Gastrointestinal Endoscopy
By knowing these guidelines and talking to your doctor, you can protect your colon health.
Understanding the Risks of Colonoscopy Procedures
Colonoscopy is a key tool for finding colorectal cancer. But, it’s important to know the risks. It’s safe for most people, but it can have complications.
Common Side Effects and Complications
Most men have colonoscopies without big problems. But, some might feel bloated or have cramps. They might also see blood in their stool, feel nauseous, or vomit.
Even though these side effects are common, serious problems are rare. It’s good to know about these risks before getting a colonoscopy.
Serious but Rare Risks
Though rare, serious issues can happen. These include:
- Perforation of the colon, which might need surgery.
- Bleeding that could need a blood transfusion.
- Reaction to sedation, like breathing or heart problems.
- Infection, which is very rare.
Risk vs. Benefit Analysis
When thinking about colonoscopy, weigh the risks against the benefits. For most men, the benefits of finding and preventing colorectal cancer are greater. Early detection can greatly improve treatment and survival chances.
The American Cancer Society says the risk of dying from colorectal cancer is much higher than the risk of colonoscopy complications. This shows how important colonoscopy is for men’s health.
Age-Related Risks for Older Men
Older men, over 75, might face higher risks due to health issues or medications. It’s key for them to talk to their doctor about their specific risks. This helps them decide if colonoscopy is right for them.
In summary, colonoscopy has risks, but knowing them helps men make smart health choices. Regular screenings can save lives. Being aware of possible complications prepares people for the procedure.
Lifestyle Factors Affecting Colonoscopy Timing for Men
Knowing how lifestyle choices affect colorectal cancer risk is key for men. Lifestyle habits can change a man’s risk of getting colorectal cancer. This affects when he should get screened.
Diet and Nutrition Impact on Colorectal Health
A man’s diet is very important for his colorectal health. Eating lots of fruits, vegetables, and whole grains can lower the risk of colorectal cancer. But, eating a lot of processed meats and not enough fiber can raise this risk.
Nutritional Recommendations:
- Eat more fruits and vegetables
- Choose whole grains more often
- Eat less processed and red meats
Physical Activity and Obesity Considerations
Being active can lower the risk of colorectal cancer. But, being obese or inactive can increase this risk. Men who are active tend to have a lower risk of colorectal cancer.
| Activity Level | Relative Risk |
| High | 0.8 |
| Moderate | 1.0 |
| Low | 1.2 |
Smoking and Alcohol Consumption
Smoking is a big risk factor for colorectal cancer. Men who smoke are more likely to get colorectal cancer than non-smokers. Drinking too much alcohol also raises the risk of colorectal cancer.
Risk Reduction Strategies:
- Join smoking cessation programs
- Drink alcohol in moderation
Medications That May Increase Risk
Some medicines, like NSAIDs and hormone replacement therapy, can affect colorectal cancer risk. But, how they affect risk can vary. It’s best to talk to a healthcare provider about these medicines.
By changing these lifestyle factors, men can lower their risk of colorectal cancer. This might mean they don’t need a colonoscopy as soon. It’s important to talk to a healthcare provider to figure out the best screening time based on your risk.
Preparing for Your Colonoscopy: What Men Should Know
Getting ready for a colonoscopy might seem tough, but with the right info, men can feel more ready. It’s important to prepare well for a good procedure. We’re here to help you through it.
Dietary Restrictions Before the Procedure
You’ll need to eat a special diet before your colonoscopy. You’ll switch to a low-fiber diet and then clear liquids the day before. Avoid foods with seeds, nuts, or high fiber because they can stick in your colon.
Here are some foods to skip:
- Nuts and seeds
- Raw vegetables
- Fruits with seeds or skin
- Whole grains
Instead, eat clear broths, gelatin, and clear juices. Drinking lots of clear liquids is also key.
Bowel Preparation Process
Bowel prep is a big step to make sure your colon is clean. You’ll take a laxative solution to empty your colon. Your doctor will tell you exactly how to prepare, so listen carefully.
Prep can be tough, but it’s needed for a good colonoscopy. You might feel some discomfort, but it’s short-lived.
Medications to Avoid
Some medicines can mess with your colonoscopy or raise risks. Tell your doctor about all your medicines, like blood thinners, diabetes meds, and supplements.
You might need to change or stop some medicines before the test. Your doctor will tell you how to handle your meds.
Tips for an Easier Preparation Experience
Even though prep is hard, there are ways to make it easier. Drink lots of water and follow the prep instructions closely. Some people find drinking the prep through a straw or chilling it helps.
Having someone to support you during prep can also help a lot. They can remind you, offer emotional support, and answer any questions.
What to Expect During and After the Procedure
Knowing what happens during and after a colonoscopy can make you feel less anxious. We’ll guide you through the whole process. This includes the procedure itself, your recovery, and getting back to your daily activities.
The Colonoscopy Experience
A colonoscopy is usually done as an outpatient procedure. You won’t need to stay in the hospital overnight. You’ll get conscious sedation to relax and feel less pain during the test. The whole procedure takes about 30 to 60 minutes.
A flexible tube with a camera is inserted into your rectum. This lets the doctor see inside your colon. They can look for any problems like polyps or inflammation.
Recovery Time and Post-Procedure Care
After the test, you’ll go to a recovery area. Here, you’ll be watched until the sedation wears off. This can take 30 minutes to an hour. You might feel a bit drowsy or uncomfortable.
When you’re discharged, make sure someone drives you home. You might feel the effects of the sedation. You might also feel some gas or bloating, but this usually goes away quickly.
When to Contact Your Doctor After the Procedure
Even though complications are rare, it’s good to know when to call your doctor. Call them if you have:
- Severe abdominal pain
- Rectal bleeding that doesn’t stop
- Fever or chills
- Dizziness or fainting
Returning to Normal Activities
Most men can go back to their usual activities the day after. But, it’s best to avoid strenuous activities or heavy lifting for the rest of the day.
Your doctor will tell you what to eat and what medicines to avoid. Usually, you can go back to your normal diet the day after.
By knowing what to expect, you can prepare better for your colonoscopy. If you have any questions or concerns, talk to your healthcare provider.
Alternative Screening Options for Colorectal Cancer
Colonoscopy is the top choice for finding colorectal cancer. But, there are other ways to screen for it too. These options are good for people who can’t or don’t want to have a colonoscopy. They offer different levels of effectiveness and ease, helping those who are hesitant or can’t have a colonoscopy.
Stool-Based Tests (FIT, gFOBT, Cologuard)
Stool tests are easy and don’t hurt. They look for hidden blood or other signs in your stool that might mean cancer. The main types are:
- Fecal Immunochemical Test (FIT): Finds human hemoglobin in your stool.
- Guaiac-based Fecal Occult Blood Test (gFOBT): Looks for blood in your stool with a chemical reaction.
- Cologuard: A test that finds DNA markers and hemoglobin in your stool.
These tests are done once a year. They’re easier than colonoscopy but might miss some polyps.
CT Colonography (Virtual Colonoscopy)
CT colonography, or virtual colonoscopy, uses CT scans to see your colon. It’s not invasive and doesn’t need sedation or a colonoscope. You’ll need to prepare your bowel like for a colonoscopy.
Benefits include: It’s safer, you recover faster, and you can see your colon from outside.
But, if it finds something, you’ll need a colonoscopy to check it. There’s also a tiny chance of getting too much radiation.
Flexible Sigmoidoscopy
Flexible sigmoidoscopy looks at the lower colon with a flexible tube and camera. It needs less prep than colonoscopy and doesn’t need sedation.
It’s not as thorough as colonoscopy, looking only at the sigmoid colon and rectum. But, it can find cancers and polyps in those areas.
Comparing Effectiveness of Alternatives to Traditional Colonoscopy
When looking at different screening methods, we consider how accurate they are, how easy they are to do, and how safe they are.
| Screening Method | Accuracy | Convenience | Risk |
| Colonoscopy | High | Moderate | Low to Moderate |
| Stool-Based Tests | Moderate to High | High | Low |
| CT Colonography | High | Moderate | Low (radiation risk) |
| Flexible Sigmoidoscopy | Moderate | Moderate | Low |
In summary, while colonoscopy is the best way to screen for colorectal cancer, there are other options. These alternatives are good for those who can’t or don’t want to have a colonoscopy. It’s important to talk to a doctor to find the best screening method for you.
Insurance Coverage and Cost Considerations
Colonoscopies are key in fighting colorectal cancer. They are covered by many insurance plans, but the details can differ. Knowing your insurance options is key to making smart health choices.
Private Insurance Coverage
Private insurance plans differ in what they cover for colonoscopies. But, it matters if the test is for prevention or diagnosis. Always check your plan to know what you might pay.
Options for Uninsured Men
For men without insurance, a colonoscopy can seem too expensive. But, there are ways to make it more affordable. Some doctors offer lower prices for those paying out of pocket. Community health centers or clinics might also offer low-cost or free screenings. Plus, some companies and non-profits have programs to help with costs.
Understanding Preventive vs. Diagnostic Colonoscopy Billing
The type of colonoscopy you get affects your costs. A preventive test is for people without symptoms, while a diagnostic test is for those with symptoms or abnormal results. Insurance usually covers preventive tests without extra costs. Knowing the type of test you’re getting helps you plan for any costs.
| Insurance Type | Preventive Colonoscopy Coverage | Diagnostic Colonoscopy Coverage |
| Private Insurance | Varies by plan, often fully covered | Varies by plan, may involve copay or coinsurance |
| Uninsured | Self-pay rates or discounted programs available |
Knowing about your insurance and the cost of a colonoscopy helps you navigate healthcare. It ensures you get the screenings you need without financial surprises.
Upper Age Limits: When to Stop Getting Colonoscopies
For elderly men, figuring out when to stop colonoscopies is important. It depends on health factors. As we get older, the risks and benefits change. It’s key to look at health and how long we might live.
Guidelines for Men Over 75
Guidelines say men over 75 should talk to their doctor about colonoscopies. The American Cancer Society and others offer help in making these decisions.
“The decision to continue or stop colonoscopies should be based on a man’s overall health, life expectancy, and previous screening results,” as emphasized by recent medical guidelines.
Considerations for Men Over 85
For men over 85, the decision is more complex. Health issues, thinking ability, and quality of life are important. These factors help decide if screenings are right.
It’s clear that “one size does not fit all” for elderly men and colonoscopy screenings. A personalized approach is vital.
Quality of Life and Risk Assessment for Elderly Men
It’s important to think about quality of life and risks of colonoscopy for elderly men. Health conditions, physical and mental function, and past screenings matter.
- Life expectancy
- Presence of comorbid conditions
- Cognitive and physical function
- Previous colonoscopy results
These factors help doctors and patients make good choices about screenings.
Decision-Making Process with Healthcare Providers
Deciding on colonoscopies involves talking with your doctor. It’s important to think about the benefits and risks. Also, consider what matters most to you.
Shared decision-making is key. It means decisions are made based on your unique situation and what you value.
By talking openly with doctors, elderly men can make choices that fit their health goals and quality of life.
Colorectal Cancer Statistics and Trends in Men
Colorectal cancer in men is changing, with new trends in incidence and outcomes. It’s important to understand these trends to improve men’s health.
Incidence Rates by Age Group
Colorectal cancer rates differ by age. Men over 50 face higher rates. Here are the rates:
- Men aged 50-59: 34.6 per 100,000
- Men aged 60-69: 54.8 per 100,000
- Men aged 70 and above: 123.7 per 100,000
These numbers show why screening is key as men get older.
Survival Rates and Early Detection Benefits
Early detection boosts survival chances for colorectal cancer. At an early stage, the 5-year survival rate is about 90%. But, if caught late, it drops to 14%.
Early detection is key to better outcomes, making regular screening vital.
Changing Trends in Younger Men
Younger men are seeing more colorectal cancer cases. Studies show an increase in men under 50. This calls for earlier screening in those at high risk.
“The increasing incidence of colorectal cancer in younger adults is a significant concern, necessitating a reevaluation of current screening guidelines.”
” American Cancer Society
Disparities in Screening and Outcomes
There are disparities in screening and outcomes among different groups. For example, African American men face higher rates and later diagnoses than others.
It’s vital to tackle these disparities. Targeted interventions and awareness can help close the gap in screening and survival rates.
Conclusion:
Colonoscopy is key for men’s health, helping find and stop colorectal cancer early. Knowing when to get screened is important for your health. Men should think about their family history and age to decide when to have their first colonoscopy.
Good colorectal health is more than just a colonoscopy. It’s about taking care of your whole health. By learning about colonoscopy and other screenings, men can make smart health choices.
We urge men to talk to their doctors about their health risks and screening needs. This way, they can take care of their colorectal health and lower their cancer risk.
FAQ
What is the recommended age for men to get their first colonoscopy?
Men should get their first colonoscopy at 45 years old, say major medical groups. But, if you have a family history or health issues, you might need to start sooner.
How often should men get a colonoscopy?
How often you need a colonoscopy depends on your risk and past results. Most men with no risk factors need one every 10 years. Those with higher risks might need it every 3-5 years.
What are the signs and symptoms that warrant earlier colonoscopy screening?
Signs like rectal bleeding, changes in bowel habits, unexplained weight loss, and fatigue mean you might need a colonoscopy sooner. If you notice these, see your doctor right away.
Are there alternative screening options for colorectal cancer beside colonoscopy?
Yes, there are other tests like stool tests, CT colonography, and flexible sigmoidoscopy. But, they might not be as thorough as a colonoscopy.
What are the possible risks and complications of colonoscopy?
You might feel bloated, gassy, or uncomfortable after a colonoscopy. But, serious risks like bleeding or perforation are rare. Talking to your doctor about the risks can help you decide if screening is right for you.
How can men prepare for a colonoscopy?
To prepare, you’ll need to follow a special diet and use bowel prep. Drink plenty of water and follow your doctor’s advice closely for a smoother experience.
What can men expect during and after the colonoscopy procedure?
During the procedure, you’ll be sedated and watched over. After, you might feel some discomfort but can usually get back to normal in a day or two.
Are there any lifestyle factors that can impact the timing and necessity of colonoscopy?
Yes, your diet, exercise, smoking, and alcohol use can affect your colon health. These factors might influence when or if you need a colonoscopy.
At what age can men stop getting colonoscopies?
Men over 75 should talk to their doctor about stopping screenings. It depends on your health and how long you might live. For those over 85, it’s based on your health and quality of life.
Reference
- Cornford, P., et al. (2024). EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer. European Urology, 86(2), 183-204. https://pubmed.ncbi.nlm.nih.gov/38614820/