ANCA-associated vasculitis is a rare but serious disease. It affects small blood vessels and can lead to organ failure and death. It needs aggressive and evidence-based treatment to save lives.
We offer top-notch care by following the 2024 KDIGO clinical guidelines. We also use strict immunosuppressive protocols. These focus on both treating the disease well and keeping patients safe.treatment of anca vasculitisTest for Antibodies: The Ultimate, Simple Guide
Recent updates from KDIGO and EULAR highlight the importance of rituximab and avacopan. These treatments offer new hope for those with ANCA-associated vasculitis. This complex condition has long been a challenge.

ANCA-associated vasculitis (AAV) is a group of autoimmune diseases that harm small blood vessels. We will look into what it is, how common it is, and why it happens.
AAV is marked by the presence of anti-neutrophil cytoplasmic antibodies (ANCA). It mainly affects small blood vessels. It’s quite rare, with about 20 cases per million people each year.
The disease comes in different forms. These include Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
AAV used to be very deadly, often because of kidney failure or organ damage. But thanks to better treatments, like immunosuppressive therapy, the outlook has changed. Now, AAV is seen as a chronic condition that can be managed for many patients.
The disease starts when ANCA activates neutrophils. This leads to the release of harmful substances that damage small blood vessels. This damage causes the symptoms of AAV, like vasculitis and kidney problems.
|
Type of AAV |
Characteristics |
Common Organ Involvement |
|---|---|---|
|
GPA |
Presence of granulomas, PR3-ANCA positive |
Upper respiratory tract, lungs, kidneys |
|
MPA |
Necrotizing vasculitis, MPO-ANCA positive |
Kidneys, lungs |
|
EGPA |
Eosinophilia, asthma, MPO-ANCA positive in some cases |
Lungs, heart, gastrointestinal tract |
By understanding AAV, we can see how complex it is. This helps us know why we need specific treatments for each patient.
It’s important to know the different types of ANCA vasculitis, like GPA, MPA, and EGPA. This knowledge helps doctors make the right diagnosis and treatment plan. Each type has its own challenges and ways to treat it.
GPA, also known as Wegener’s granulomatosis, causes inflammation and damage to the airways and blood vessels. PR3-ANCA is found in about 80-90% of GPA patients.
GPA can show up in many ways, from mild to severe. Symptoms include sinus infections, ear infections, and lung problems. Kidney damage is also common and can be serious.
MPA mainly affects small blood vessels and doesn’t have many immune deposits. MPO-ANCA is more common in MPA than PR3-ANCA. It often causes kidney and lung problems.
MPA can make people feel very sick, with symptoms like weight loss, fever, and joint pain. It can get worse quickly, so fast action is needed.
EGPA is known for its eosinophils and granulomas in the airways and blood vessels. Asthma and high eosinophil counts are key signs. People with EGPA often have allergies and asthma before the disease starts.
EGPA goes through three stages: allergic symptoms, eosinophilic phase, and vasculitic phase. Heart problems are a big worry and can be deadly.
|
Phenotype |
Common ANCA Association |
Key Clinical Features |
|---|---|---|
|
GPA |
PR3-ANCA |
Necrotizing granulomatous inflammation, upper and lower respiratory tract involvement, renal disease |
|
MPA |
MPO-ANCA |
Necrotizing vasculitis, renal involvement, pulmonary hemorrhage |
|
EGPA |
Variable |
Asthma, eosinophilia, granulomatous inflammation, cardiac involvement |
Knowing the different types of ANCA vasculitis is key for doctors. It helps them diagnose and treat each type better. This way, patients get the care they need.
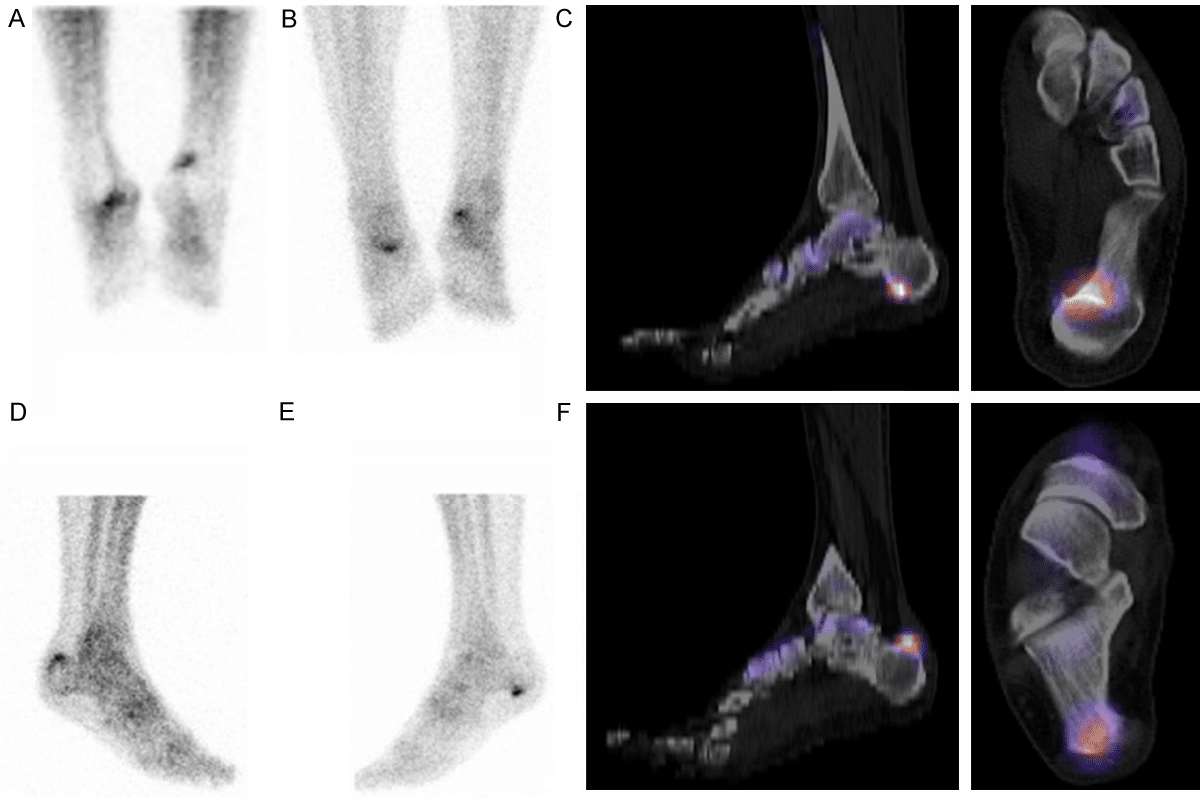
Diagnosing ANCA vasculitis needs a detailed approach. This includes looking at symptoms, lab tests, and tissue samples. This method helps identify the disease and tell it apart from others.
ANCA vasculitis shows up in different ways, based on which organs are affected. Symptoms can include kidney problems, breathing issues, and systemic signs like fever and weight loss. It’s important to carefully assess each patient’s symptoms.
For example, people with Granulomatosis with Polyangiitis (GPA) often have sinusitis and nasal crusting. Those with Microscopic Polyangiitis (MPA) might have kidney and lung issues. Eosinophilic Granulomatosis with Polyangiitis (EGPA) usually starts with asthma and high eosinophil counts.
Lab tests are key in diagnosing ANCA vasculitis. Finding anti-neutrophil cytoplasmic antibodies (ANCA) is a major diagnostic tool. There are two main types: PR3-ANCA and MPO-ANCA. PR3-ANCA is linked to GPA, while MPO-ANCA is seen in MPA and EGPA.
Testing for ANCA has gotten better with new methods. Indirect immunofluorescence (IIF) and enzyme-linked immunosorbent assay (ELISA) are used to find ANCA. A positive test, along with symptoms, helps confirm ANCA vasculitis.
Looking at tissue samples is often needed to confirm the diagnosis. A kidney biopsy is very helpful in checking kidney health and finding vasculitis. The biopsy shows necrotizing vasculitis and granulomatous inflammation.
A biopsy gives important info on organ damage and helps decide treatment. Sometimes, biopsies from other organs like the lung or skin are done to support the diagnosis.
“The diagnosis of ANCA-associated vasculitis is a complex process that requires integration of clinical, laboratory, and histopathological findings.”
— Expert Consensus Statement
The way we classify ANCA-associated vasculitis has changed a lot in recent years. This change helps us understand the disease better. It also makes diagnosing and treating patients more effective.
The 2023 updates in vasculitis classification have brought big changes. Now, we can tell different types of ANCA-associated vasculitis apart more clearly. This is thanks to new ways of looking at the disease.
Key Updates in 2023 Classification:
Serological classification is key in diagnosing and managing ANCA vasculitis. Knowing if a patient has PR3-ANCA or MPO-ANCA helps doctors decide on treatment. It also helps predict how the disease will progress.
PR3-ANCA Positive Vasculitis is often seen in GPA and has a different set of symptoms than MPO-ANCA Positive Vasculitis. The latter is more common in MPA and usually affects the kidneys.
|
Characteristics |
PR3-ANCA Positive |
MPO-ANCA Positive |
|---|---|---|
|
Common Clinical Presentation |
GPA, often with upper respiratory tract involvement |
MPA, typically with renal involvement |
|
Serological Marker |
PR3-ANCA |
MPO-ANCA |
The new classification of ANCA vasculitis has big implications for doctors. Knowing the exact type of vasculitis helps doctors create better treatment plans. This leads to better health outcomes for patients.
Understanding the differences between PR3-ANCA and MPO-ANCA helps doctors tailor treatments. This makes therapy more effective for each patient.
Clinical Implications:
Managing ANCA vasculitis has evolved with new KDIGO and EULAR guidelines. These updates aim to improve patient care and reduce side effects. They focus on better treatment options for this complex condition.
The 2024 KDIGO guidelines update treatment recommendations for ANCA vasculitis. They highlight the importance of rituximab and avacopan in starting treatment. Rituximab is seen as a good alternative to cyclophosphamide for starting therapy.
The 2022 EULAR guidelines match the KDIGO recommendations. They offer a detailed plan for managing ANCA vasculitis. They stress the need to assess disease severity to choose the right treatment.
It’s key to assess disease severity in ANCA vasculitis. We use clinical checks, lab tests, and imaging to see how much organs are affected. This helps decide the best treatment.
By tailoring treatment to disease severity, we can improve patient results and lower treatment risks.
Managing ANCA vasculitis starts with the right induction therapy. This phase is key to getting the disease under control and into remission.
Glucocorticoids are vital in treating ANCA vasculitis. They are given in high doses first, then slowly reduced. “The use of glucocorticoids has significantly improved outcomes in patients with ANCA vasculitis,” as noted in recent clinical guidelines.
We start with pulse intravenous methylprednisolone for severe cases. Then, we switch to oral prednisone. The tapering schedule is important to avoid side effects while keeping the disease in check.
Rituximab targets CD20-positive B cells and is a key part of induction therapy. It’s shown to be as effective as cyclophosphamide in achieving remission. Rituximab offers a valuable alternative for patients who are intolerant to cyclophosphamide or have relapsing disease.
The usual dose of rituximab is two 1g doses, given two weeks apart. It’s important to watch for infections due to its immunosuppressive effects.
Cyclophosphamide is a traditional treatment for ANCA vasculitis. It’s effective for severe cases but has side effects like infertility and cancer risk.
“Cyclophosphamide remains a critical agent in the treatment of ANCA vasculitis, particular for patients with severe renal involvement or other life-threatening manifestations.” The dose and duration of cyclophosphamide therapy are adjusted based on patient response and tolerance.
In conclusion, the choice of induction therapy for ANCA vasculitis depends on disease severity, patient health, and side effects. A personalized approach, following the latest guidelines and considering patient preferences, is key for the best management.
Maintenance therapy is key in managing ANCA vasculitis long-term. It helps prevent relapse and keeps the disease in remission.
The right length of maintenance therapy in ANCA vasculitis is debated. Current guidelines suggest at least 24 months of therapy after remission. But, the decision to keep going or stop depends on the patient’s risk and disease details.
Rituximab is a good choice for keeping ANCA vasculitis under control. Studies have shown it can stop relapses, mainly in those who often relapse or are PR3-ANCA positive.
Besides rituximab, azathioprine and methotrexate are also used. The choice depends on the patient’s health, other medications, and how they’ve reacted to treatments before.
|
Therapy |
Advantages |
Disadvantages |
|---|---|---|
|
Rituximab |
Effective in preventing relapses, mainly in PR3-ANCA positive patients |
Needs intravenous use, might cause infusion reactions |
|
Azathioprine |
Easy to take orally, generally well-tolerated |
Can lower blood cells, liver damage risk |
|
Methotrexate |
Easy to take orally, safe for those with kidney issues |
Can harm the liver, not safe during pregnancy |
Managing ANCA vasculitis needs careful thought, mainly for complex patient groups. Certain groups need a special approach to manage the disease well and avoid complications.
Renal issues are a big worry in ANCA vasculitis, often showing as rapidly progressive glomerulonephritis. Prompt diagnosis and treatment are key to avoid permanent kidney damage. We suggest regular checks on kidney function and urine to spot kidney problems early.
Having anti-MPO or anti-PR3 antibodies can affect how likely and severe kidney problems are. Studies show MPO-ANCA positive patients are more likely to have kidney disease.
|
Renal Involvement Characteristics |
MPO-ANCA Positive |
PR3-ANCA Positive |
|---|---|---|
|
Frequency of Renal Disease |
Higher Incidence |
Lower Incidence |
|
Severity of Renal Involvement |
Often Severe |
Variable Severity |
Managing ANCA vasculitis in pregnancy is challenging. It’s important to balance controlling the disease with keeping the mother and baby safe. Close collaboration between rheumatologists and obstetricians is key.
Pregnant patients with ANCA vasculitis need regular checks on disease activity and kidney function. Choosing the right immunosuppressive therapy is critical to avoid harming the fetus.
Elderly patients with ANCA vasculitis often have other health issues and may face more side effects from treatment. Comprehensive geriatric assessment helps make treatment decisions and improve care.
We suggest adjusting treatments based on the patient’s health, kidney function, and drug interactions. Rituximab and glucocorticoids are common choices, with careful watch for infections and other issues.
Atypical cases of ANCA vasculitis, including B-ANCA positivity, need a quick and thorough diagnosis. Early recognition is vital to start the right treatment and prevent organ damage.
Managing atypical cases requires a team effort from rheumatology, nephrology, and other specialists as needed.
ANCA-associated vasculitis (AAV) is a complex disease needing a detailed treatment plan. The 2023 updates and 2024 KDIGO guidelines have helped us better understand and manage AAV. They show how important it is to tailor treatments based on how severe the disease is and the patient’s specific needs.
New research and treatments are on the horizon to help AAV patients. We’re learning more about the disease’s causes and finding new ways to treat it. In the future, treatments will likely be more personalized, taking into account the patient’s specific situation.
As we look ahead, using rituximab and other new treatments will become more common. This will bring new hope to those with hard-to-treat AAV. By keeping up with the latest in AAV management, healthcare providers can give better care and improve patient outcomes.
ANCA-associated vasculitis (AAV) is a group of autoimmune disorders. They cause inflammation in blood vessels, mainly in small ones. The main types are Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
Doctors use a mix of symptoms, lab tests, and tissue samples to diagnose it. Kidney biopsies or other tissue samples are often needed.
The 2024 KDIGO Clinical Practice Guidelines and 2022 EULAR recommendations guide treatment. They focus on how severe the disease is and how to treat it.
Rituximab is used to start and keep treatment going in ANCA vasculitis. It’s an alternative to cyclophosphamide and helps some patients.
How long and what to use for maintenance therapy depends on the disease’s severity. It also depends on how the patient responds and other clinical factors.
Managing ANCA vasculitis during pregnancy needs careful planning. A team of doctors works together to control the disease while considering pregnancy risks.
Elderly patients face unique challenges. These include other health issues, higher risk of treatment side effects, and the need for tailored treatment plans.
PR3 and MPO ANCA help classify AAV. This classification affects treatment choices and might influence how well the patient does.
The 2023 updates bring new insights into AAV. They might lead to better diagnosis and treatment, based on the latest research and classification.
New research and treatments are on the horizon. They aim to make treatments more targeted and effective for AAV.
National Center for Biotechnology Information. Positive ANCA Test: Meaning and Implications for Patient Health. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750501/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!