Getting a correct and quick diagnosis of acute myeloid leukemia (AML) is key for the best health results. We use the newest global guidelines, like the European LeukemiaNet (ELN) 2022, to understand AML’s diagnostic signs.
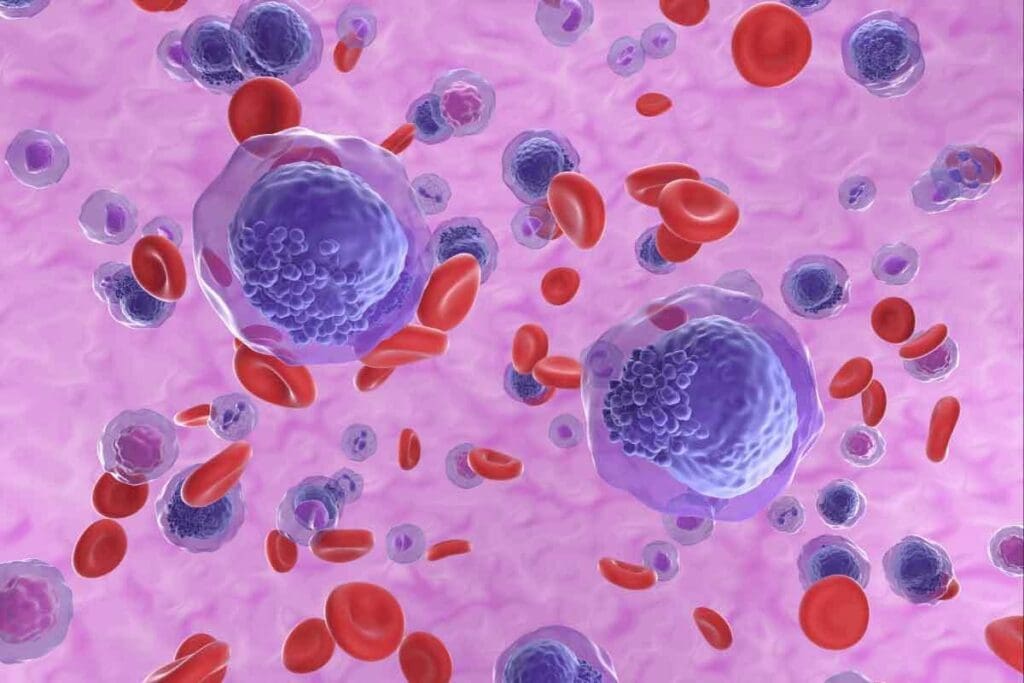
AML is a diverse group of blood cancers. It happens when myeloid cells grow too much in the bone marrow. A main sign of AML is having ≥20% myeloid blasts in the bone marrow or blood. We also use immunophenotyping, cytogenetic, and molecular studies to find AML’s specific mutations.
At Liv Hospital, we aim to give top-notch healthcare. We offer full support and help to international patients. Our AML diagnosis follows the latest criteria and guidelines. This ensures our patients get the best treatment.
Key Takeaways
- Accurate AML diagnosis relies on identifying ≥20% myeloid blasts in bone marrow or peripheral blood.
- The European LeukemiaNet (ELN) 2022 guidelines provide a framework for understanding AML diagnostic criteria.
- Modern diagnostics involve immunophenotyping, cytogenetic, and molecular studies to identify AML-defining mutations.
- Liv Hospital is committed to delivering world-class healthcare with full international patient support and guidance.
- Our approach to AML diagnosis is centered on the latest diagnostic criteria and guidelines.
Current Understanding of Acute Myeloid Leukemia
To understand AML, we need to look at many angles. This includes studying its causes, genetics, and how it first shows up. Knowing these things helps doctors figure out how to treat it.
Definition and Pathophysiology
AML is a serious blood cancer. It happens when the bone marrow makes too many immature cells. Doctors use immunophenotyping, cytogenetic, and molecular studies to find the exact cause. This helps them understand the disease better.
Epidemiology and Risk Factors
Most people with AML are over 60 years old. The disease is not very common in younger people. Studies show that certain chemicals, radiation, and genes can increase the risk of getting AML.
Clinical Presentation and Early Warning Signs
AML can show up in many ways, like feeling weak or getting infections easily. These signs are not unique to AML. So, it’s hard to know right away if someone has it. But, noticing these signs is important for getting tested.
Doctors use tests like bone marrow exams and molecular tests to confirm AML. This helps them decide the best treatment. Knowing about AML’s causes, signs, and how it’s diagnosed helps doctors do better for their patients.
The 7 Fundamental AML Diagnosis Criteria for 2025

In 2025, diagnosing Acute Myeloid Leukemia (AML) will involve several key steps. These include looking at cell shape, checking for specific proteins, and studying chromosomes. Getting an AML diagnosis right is key for better treatment and patient care.
The ≥20% Myeloid Blasts Threshold
A main sign of AML is having ≥20% myeloid blasts in the bone marrow or blood. This rule helps tell AML apart from other blood disorders.
Recent rules say you need 20% or more blasts in the blood or bone marrow to be diagnosed. But, some chromosome changes can also point to AML, even with fewer blasts.
Morphological Assessment
Morphological assessment is very important for AML diagnosis. It looks at bone marrow and blood smears to find specific cells. This helps figure out the cell’s type and how mature it is.
Immunophenotypic Profile
Immunophenotyping helps identify the proteins on AML cells’ surface. It uses flow cytometry to spot specific markers. This helps diagnose and classify AML accurately.
Cytogenetic Abnormalities
Cytogenetic analysis is key to finding chromosome changes in AML. These changes can help diagnose AML, predict how the disease will progress, and guide treatment. Some changes can even diagnose AML with fewer blasts.
| Diagnostic Criterion | Description | Clinical Significance |
| ≥20% Myeloid Blasts | Presence of 20% or more myeloid blasts in bone marrow or peripheral blood | Diagnostic threshold for AML |
| Morphological Assessment | Examination of bone marrow and peripheral blood smears | Identifies characteristic myeloid blast cells |
| Immunophenotypic Profile | Characterization of immunological markers on AML cells | Aids in diagnosis and subclassification |
| Cytogenetic Abnormalities | Identification of chromosomal abnormalities | Diagnostic, prognostic, and therapeutic targets |
Peripheral Blood Smear Analysis in AML Diagnosis
In diagnosing AML, a key first step is the peripheral blood smear analysis. This method looks at a blood sample under a microscope. It checks for any oddities in the blood cells.
Identifying Circulating Blasts
AML is often marked by the presence of circulating blasts in the blood. Blasts are immature cells that should be in the bone marrow. When they show up in the blood, it might mean leukemia. We spot these cells by their large size, large nucleoli, and little cytoplasm.
Morphological Features of AML Cells
Looking at AML cells under a microscope is a big part of diagnosing them. AML cells can look very different, making it hard to tell them apart. But features like Auer rods are a big clue that points to AML.
Limitations and Confirmatory Testing
Even though blood smear analysis is helpful, it’s not perfect. Blasts can be seen in other conditions too, not just AML. So, more tests like flow cytometry, cytogenetics, and molecular studies are needed to confirm the diagnosis.
Advanced Digital Morphology Techniques
New digital tools have made blood smear analysis better. Now, machines can spot and sort cells very accurately, making the job easier. These tools help make AML diagnosis faster and more precise.
| Diagnostic Method | Key Features | Advantages |
| Peripheral Blood Smear | Identifies circulating blasts, morphological features | Quick, initial assessment |
| Flow Cytometry | Immunophenotyping of cells | High specificity confirms the diagnosis |
| Digital Morphology | Automated cell analysis | Increased accuracy, efficiency |
European LeukemiaNet (ELN) 2022 Classification System
The ELN 2022 classification system is a big step forward in AML diagnosis. It updates the European LeukemiaNet’s guidelines with new molecular findings and clinical trial results. This helps us better understand and treat Acute Myeloid Leukemia (AML).
These updates are key to improving patient care. They give a clearer view of AML subtypes and how to manage them. The ELN 2022 guidelines use the latest knowledge to help doctors diagnose and treat AML.
Evolution from Previous Classifications
The ELN 2022 classification is a new version that includes fresh insights and trial data. This change is important because it shows how much we’ve learned about AML’s genetics and molecules.
By updating the system, the ELN wants to make AML diagnosis more accurate. It also aims to make treatments more personalized. New genetic markers and risk categories help doctors predict outcomes and choose the right treatments.
Risk Stratification Categories
The ELN 2022 guidelines have new risk categories for AML. These categories are vital for knowing how well a patient will do and what treatment they need.
The new risk categories are based on the latest genetic and molecular data. This makes it easier to put patients into the right risk groups. It helps find who might need stronger or more targeted treatments.
| Risk Category | Genetic Features | Clinical Implications |
| Favorable | NPM1 mutation, certain cytogenetic abnormalities | Better prognosis, less intensive therapy possible |
| Intermediate | Intermediate-risk cytogenetics, certain molecular mutations | Standard treatment approaches |
| Adverse | High-risk cytogenetics, TP53 mutations, complex karyotypes | Poor prognosis, intensive therapies or clinical trials may be needed |
Genetic Risk Groups in ELN 2022 AML
The ELN 2022 classification also updates genetic risk groups. These updates are important for finding patients with specific genetic profiles that affect treatment response.
By using genetic findings and clinical features, the ELN 2022 guidelines help tailor AML management. This personalized approach is expected to lead to better patient outcomes by matching treatments to each patient’s leukemia.
Clinical Implementation and Future Refinements
The ELN 2022 classification system is expected to improve AML diagnosis and treatment in clinical practice. As more data comes in, the system will likely evolve further. This will help make AML management even more precise and effective.
We expect the ELN 2022 guidelines to greatly impact how AML is treated. They will help healthcare providers give more targeted and effective care. As we learn more about AML, the classification system will continue to evolve, ensuring patients get the best treatments available.
AML-Defining Mutations and Their Clinical Significance
Understanding AML-defining mutations is key to accurate diagnosis and treatment planning in acute myeloid leukemia patients. Modern diagnostics rely on molecular studies to find these mutations. They play a big role in predicting outcomes and guiding treatment.
NPM1 Mutations: Diagnosis and Prognosis
NPM1 mutations are common in AML, found in about 30% of adult patients. These mutations cause the nucleophosmin protein to move to the wrong place in the cell. NPM1 mutations are linked to a better prognosis, mainly when there are no other bad genetic features. They also affect the decision to do stem cell transplantation in first complete remission.
FLT3 Mutations (ITD and TKD)
FLT3 mutations, including ITD and TKD, are found in about 30% of AML patients. FLT3-ITD mutations are linked to a higher risk of relapse and poorer survival. The ratio of FLT3-ITD to wild-type FLT3 is also important, with higher ratios meaning worse outcomes. FLT3 inhibitors are being used as targeted treatments for these mutations.
CEBPA and RUNX1 Alterations
CEBPA mutations are found in about 10% of AML cases and are linked to a good prognosis with double mutations. Double CEBPA mutations disrupt normal C/EBPα function. RUNX1 mutations, on the other hand, are linked to a bad prognosis and are often seen in AML with myelodysplasia-related changes.
TP53 Mutations and Complex Karyotypes
TP53 mutations are rare in AML but have a very poor prognosis, worse with complex karyotypes. Complex karyotypes have three or more chromosomal abnormalities and often come from myelodysplastic syndromes or genotoxic agents. TP53 mutations make treatment choices harder and often require new approaches.
Advanced Diagnostic Techniques in AML
Advanced diagnostic techniques are changing how we diagnose AML. They help us find the right treatment for each patient. Now, we use immunophenotyping and molecular studies to find AML-defining mutations. These are key for accurate diagnosis and treatment planning.
Multiparameter Flow Cytometry
Multiparameter flow cytometry is a key tool in AML diagnosis. It looks at many proteins on and inside cells at once. This helps us find specific markers of AML cells.
This method is great for telling AML apart from other blood cancers. It also helps us find different types of AML.
Key applications of multiparameter flow cytometry in AML diagnosis include:
- Identifying specific cell surface markers associated with AML
- Detecting minimal residual disease (MRD) after treatment
- Monitoring response to therapy
Next-Generation Sequencing Panels
Molecular diagnostics, like next-generation sequencing (NGS), are now common in AML diagnosis. NGS panels check many genes at once. This gives us a detailed genetic picture of the leukemia.
NGS offers several advantages in AML diagnosis:
- Comprehensive mutation profiling
- Identification of prognostic and predictive biomarkers
- Detection of possible therapeutic targets
Digital PCR Technologies
Digital PCR (dPCR) is becoming a powerful tool in AML diagnosis. dPCR can count specific DNA sequences exactly. This helps us find mutations and MRD very sensitively.
Benefits of dPCR in AML include:
- High sensitivity for detecting low-level mutations
- Accurate quantification of MRD
- Potential for monitoring response to targeted therapies
Artificial Intelligence in AML Diagnostics
Artificial intelligence (AI) is being explored in AML diagnostics. AI can look at lots of data, like genes and clinical info, to find patterns and predict outcomes.
Potential applications of AI in AML diagnostics include:
- Improving diagnostic accuracy through pattern recognition
- Predicting treatment response and outcomes
- Identifying novel prognostic markers
As we learn more about AML, these advanced techniques will be more important. They help us give more accurate diagnoses and treatments. This leads to better patient outcomes.
AML Response Criteria and Minimal Residual Disease
AML treatment response is checked using specific criteria, including minimal residual disease (MRD) status. It’s key to know how well treatment is working. This helps us see if the disease is getting worse or better.
Complete Remission Standards
Complete remission (CR) in AML means less than 5% blasts in the bone marrow. There should be no leukemic cells in the blood and blood counts should be back to normal. The patient’s health and no signs of disease outside the bone marrow are also important. CR shows the disease is being controlled.
MRD Assessment Methods
MRD assessment is key in AML treatment. We use multiparameter flow cytometry and molecular techniques like PCR and next-generation sequencing. These methods help find and measure small amounts of cancer cells.
Molecular Monitoring Strategies
Molecular monitoring is vital for MRD assessment. It lets us track specific genetic mutations in AML. We use quantitative PCR and next-generation sequencing to keep an eye on MRD levels. This helps us adjust treatment plans and make better decisions for patients.
Standardization of MRD Reporting
Standardizing MRD reporting is essential for consistency. We need clear protocols for MRD assessment and reporting. This way, we can compare results accurately and make informed decisions. Efforts to standardize MRD reporting are ongoing, with guidelines being developed.
In conclusion, AML response criteria, including MRD status, are vital for assessing treatment response and predicting outcomes in AML patients. By using standardized response criteria and advanced MRD assessment methods, we can provide more effective care and improve patient outcomes.
Risk-Adapted AML Treatment Guidelines
AML treatment is changing, focusing on tailoring therapy to each patient’s risk. This change comes from better diagnostic tools and new treatments.
Frontline Therapy Based on Diagnostic Findings
Today, AML treatment is more personalized than before. Treatment choices depend a lot on what the tests show, like genetic mutations. This new approach helps us understand AML better and treat it more effectively.
- Genetic Mutations: Certain mutations, like NPM1 or FLT3-ITD, play a big role in deciding treatment.
- Risk Stratification: Patients are sorted into risk groups based on their genetic and molecular features. This helps decide how intense the treatment should be.
Targeted Therapies for Specific Mutations
Targeted therapies have changed AML treatment a lot. They focus on specific mutations, helping certain patients more.
- FLT3 inhibitors for patients with FLT3 mutations.
- IDH1 and IDH2 inhibitors for patients with IDH1/2 mutations.
Stem Cell Transplantation Decision Criteria
Stem cell transplantation is key for many AML patients, mainly those with high-risk disease. Choosing to transplant involves many factors, like donor availability and patient health.
We’re making stem cell transplantation better by using new data on minimal residual disease (MRD) and its effect on transplant success.
Emerging Therapeutic Approaches for 2025
Looking ahead to 2025, new treatments are coming for AML. These include new targeted therapies, immunotherapies, and new ways to mix old treatments.
- Novel Targeted Therapies: New agents targeting specific molecular weaknesses are being developed.
- Immunotherapies: CAR-T cell therapy and other immunotherapies are being tested for AML.
By using these new approaches and updating our treatment guidelines, we’re making AML treatment better for patients.
Conclusion: Advancing AML Diagnosis for Improved Outcomes
Improving AML diagnosis is key to better patient care. We’ve made big strides in understanding Acute Myeloid Leukemia. This is thanks to new ways to diagnose and analyze the disease.
New diagnostic tools and treatment plans are changing how we manage AML. Technologies like flow cytometry and next-generation sequencing help us give patients more tailored care. This makes treatment more accurate and effective.
Research and updates in AML diagnosis will keep getting better. It’s important to keep up with the latest in AML diagnosis and treatment. This way, we can make sure patients get the best care possible. By improving how we diagnose AML, we can lead to better treatment and outcomes for patients.
FAQ
What are the key diagnostic criteria for Acute Myeloid Leukemia (AML)?
To diagnose AML, doctors look for several key signs. These include having ≥20% myeloid blasts in the bone marrow or blood. They also check the cell’s shape, its proteins, and its chromosomes.
What is the significance of the ≥20% myeloid blasts threshold in AML diagnosis?
Finding ≥20% myeloid blasts is a big clue for AML. It shows that abnormal myeloid cells are growing too much.
How is peripheral blood smear analysis used in AML diagnosis?
Peripheral blood smear analysis helps spot AML cells in the blood. It looks at the cells’ shape to help diagnose and plan treatment.
What is the European LeukemiaNet (ELN) 2022 classification system, and how does it impact AML diagnosis?
The ELN 2022 system is a new way to classify AML. It uses new findings and risk levels to better understand AML types.
What are AML-defining mutations, and how do they impact diagnosis and prognosis?
Certain mutations, like NPM1 and FLT3, are key in AML diagnosis and outlook. They help decide the risk level and treatment plan.
How are advanced diagnostic techniques, such as next-generation sequencing and digital PCR, used in AML diagnosis?
Next-generation sequencing and digital PCR help make AML diagnosis more accurate. They guide treatment choices.
What are the AML response criteria, and how is minimal residual disease (MRD) assessed?
AML response criteria help measure how well treatment works. MRD assessment, like molecular monitoring, checks for remaining disease.
How are risk-adapted AML treatment guidelines used to optimize patient outcomes?
Risk-adapted guidelines tailor treatment to each patient’s risk. This includes genetic factors and risk levels.
What is the role of targeted therapies in AML treatment, and how are they used?
Targeted therapies, like those for specific mutations, are becoming more common. They offer personalized and effective treatments.
How is stem cell transplantation used in AML treatment, and what are the decision criteria?
Stem cell transplantation is used in AML treatment. The decision to use it is based on genetic factors and risk levels.
References:
- Tripathi, A. K., & Lappin, D. (2025). Laboratory evaluation of acute leukemia. StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK611988/


































