Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know that nearly a quarter of the global population suffers from anaemia? This is a condition where there’s not enough red blood cells or hemoglobin level. Often, doctors need to give blood trans PageSpeed fusions to help. This helps restore normal red blood cell count and eases symptoms. Explaining the medical link between chronic Anaemia transfusion dependence and the need for regular red blood cell transfusions.
We’re going to talk about anaemia and transfusions. We’ll explain what they are and why knowing when to give a transfusion is key for treatment.
Key TakeawaysPageSpeed 3>
- A PageSpeed transfusion is often needed when hemoglobin levels get too low.
- Knowing when you need a blood trans PageSpeed fusion can save your life.
- Deciding to get a blood transfusion depends on many things, like why you have anaemia.
- How much Hemoglobin PageSpeed you have is very important for deciding on a transfusion.
- Doctors carefully check if you need a blood transfusion based on your needs.
What is Anaemia?
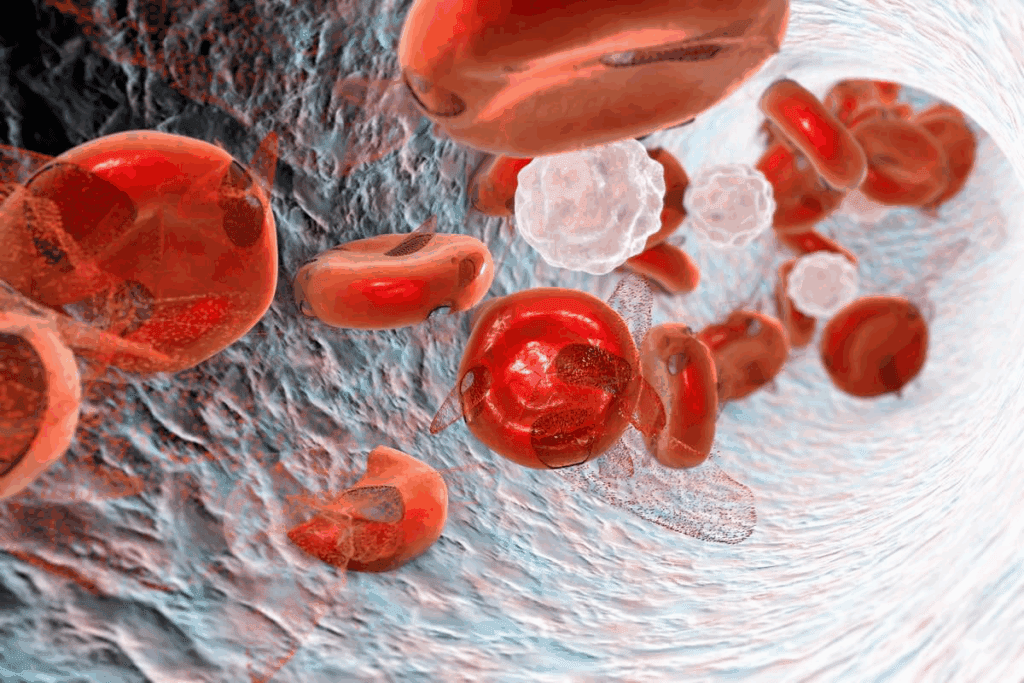
Anaemia is when your body doesn’t have enough healthy red blood cells. It’s a serious health problem. This happens when you don’t have enough red blood cells or when they don’t carry enough oxygen.
Definition and Types of Anaemia
The World Health Organization says anaemia is when your blood’s hemoglobin level is too low. This level changes based on your age, sex, and other factors. There are different types of anaemia, including:
- Iron deficiency anaemia: The most common type, caused by a lack of iron.
- Vitamin deficiency anaemia: Caused by a lack of vitamins like vitamin B12 or folate.
- Anaemia of chronic disease: Associated with chronic illnesses like kidney disease or rheumatoid arthritis.
- Sickle cell anaemia: A genetic disorder affecting hemoglobin production.
Causes of Anaemia
Many things can cause anaemia. Some common causes include:
- Nutritional deficiencies: Lack of iron, vitamin B12, or folate.
- Chronic diseases: Conditions like chronic kidney disease, cancer, or HIV/AIDS.
- Blood loss: Heavy menstrual periods, internal bleeding, or surgery.
- Genetic disorders: Sickle cell disease or thalassemia.
Symptoms of Anaemia
The symptoms of anaemia can vary. But common signs include:
- Fatigue and weakness: Feeling tired or lacking energy.
- Shortness of breath: Difficulty breathing or feeling winded even when sitting.
- Pale skin: Skin appearing pale or washed out.
- Dizziness or lightheadedness: Feeling like you might pass out.
Understanding anaemia is key to managing it. Knowing the symptoms and causes helps you get medical help early. This can prevent serious problems.
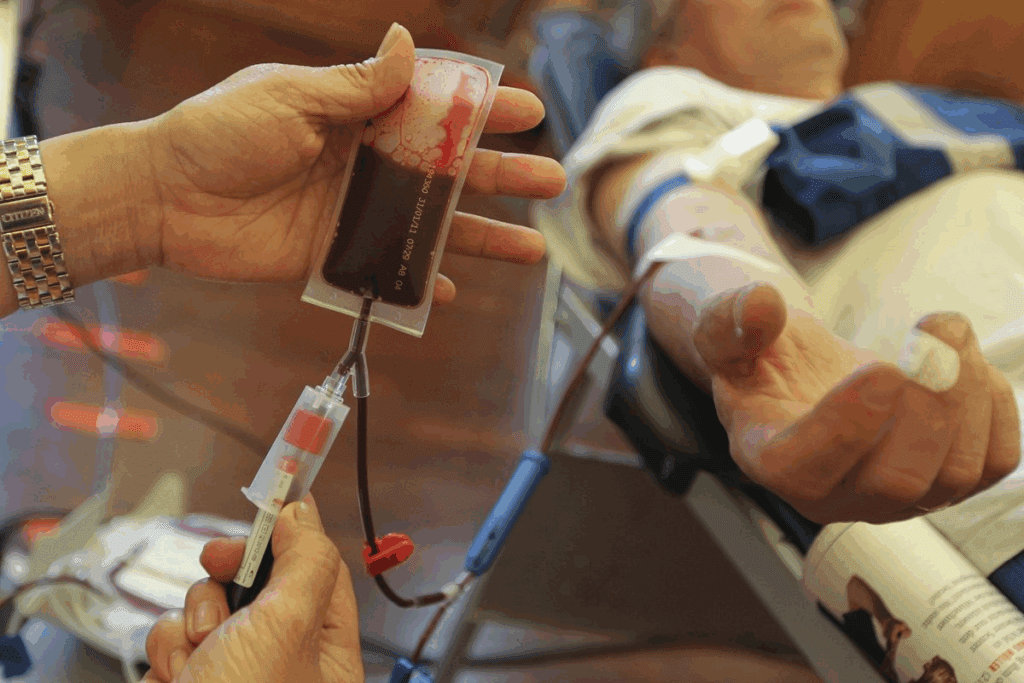
Understanding Transfusions
Blood transfusions are key in treating many medical conditions. They offer hope to patients all over the world. It’s important to understand this treatment to give our patients the best care.
What is a Blood Transfusion?
A blood transfusion is when blood or blood parts are given to a patient. This is vital for those who have had surgery, been injured, or have anaemia. It helps patients get the blood they need to recover and stay healthy.
When Are Transfusions Needed?
Transfusions are needed in many medical situations. This includes severe anaemia, blood loss from surgery or injuries, and some blood disorders. The decision to transfuse depends on the patient’s health, their condition, and their hemoglobin levels. We check each patient to see if a transfusion is right for them.
| Condition | Typical Hemoglobin Threshold for Transfusion | Considerations |
| Severe Anaemia | Less than 7 g/dL | Patient’s overall health, symptoms, and underlying cause |
| Significant Blood Loss | Varies based on the rate and volume of blood loss | Clinical judgment, patient’s vital signs, and hemoglobin levels |
| Blood Disorders | Varies depending on the disorder | Specific diagnosis, patient’s condition, and treatment goals |
Types of Blood Transfusions
There are many types of blood transfusions. Red blood cell transfusions help with anaemia or blood loss. Platelet transfusions are for those with low platelet counts. We also give plasma transfusions for clotting factors and cryoprecipitate transfusions for clotting factor deficiencies.
Knowing about these transfusions is key to effective care. We choose the right transfusion for each patient, based on their needs.
Importance of Hemoglobin Levels
Hemoglobin levels are very important. They help carry oxygen to all parts of the body. This protein in red blood cells is key for oxygen transport from the lungs to tissues.
Role of Hemoglobin in the Body
Hemoglobin is essential for the body’s health. It makes sure tissues and organs get enough oxygen. Low hemoglobin levels can cause fatigue and weakness. On the other hand, high hemoglobin levels might mean a rare blood disorder.
We will look into how hemoglobin levels affect us. Why keeping them normal is important for health.
Normal Hemoglobin Levels by Age and Sex
Hemoglobin levels change with age and sex. Adult men usually have more hemoglobin than women. For example, men’s levels are between 13.8 and 17.2 grams per deciliter (g/dL). Women’s levels are between 12.1 and 15.1 g/dL.
Children and pregnant women have their own ranges. Healthcare providers must know these to diagnose and treat anaemia correctly.
Factors Affecting Hemoglobin Levels
Many things can change hemoglobin levels. Nutritional deficiencies, like iron or vitamin B12, can affect it. So can chronic diseases, like kidney disease or cancer, and some medicines.
Altitude and smoking also play a role. Knowing these factors helps doctors treat anaemia and other conditions.
Guidelines for Blood Transfusion
It’s key for healthcare providers to know the blood transfusion guidelines. Blood transfusions are vital in patient care. They follow established medical guidelines.
Standard Hemoglobin Thresholds
The choice to give blood is often tied to the patient’s hemoglobin level. Standard hemoglobin thresholds are a guide, but not the only thing. Usually, a hemoglobin level of 7-8 g/dL is when transfusion is considered in many cases.
| Clinical Situation | Hemoglobin Threshold (g/dL) |
| Critically ill patients | 7 |
| Stable, non-critically ill patients | 8 |
| Patients with cardiovascular disease | 8-9 |
Individual Factors to Consider
While there are standard hemoglobin levels, individual patient factors are also key. These include the patient’s age, health, and symptoms like fatigue or shortness of breath.
- Age and overall health status
- Presence of cardiovascular disease or other comorbidities
- Symptoms indicative of anemia or decreased oxygen delivery
The Role of Clinical Judgment
Clinical judgment is essential in deciding to transfuse blood. Healthcare providers look at the patient’s hemoglobin level and overall health. They consider the risks of not transfusing and the benefits and risks of transfusing.
Every patient is different. So, guidelines should be flexible and consider each person’s unique situation.
Lowest Hemoglobin Level Before Transfusion
Knowing when to give blood transfusions is key for patient care. It’s not just about the hemoglobin level. Symptoms and the patient’s health also play a big role.
General Guidelines for Transfusion Thresholds
Most doctors agree that a hemoglobin level between 7 and 8 g/dL is when transfusions are usually needed. But, this can change based on the patient’s health and other factors.
For example, patients with heart problems or those having big surgeries might need transfusions at a higher hemoglobin level, around 8-10 g/dL. On the other hand, younger, healthier patients might not need transfusions even at lower levels.
Situational Exceptions to the Rule
There are times when the usual rules don’t apply. For chronic anemia patients, they might not need transfusions until their hemoglobin drops way lower than for others.
Also, patients with serious heart or lung issues might need transfusions at higher hemoglobin levels. This is to make sure they get enough oxygen. Doctors have to use their best judgment here.
Importance of Symptoms Over Numbers
Hemoglobin levels are important, but symptoms are just as key in deciding to transfuse. Signs like trouble breathing, feeling very tired, or dizzy can mean a patient needs a transfusion, even if their hemoglobin isn’t that low.
It’s vital to look at the patient’s whole situation, including their symptoms. This way, doctors can make sure the transfusion is right for the patient’s health and well-being.
Risks Associated with Blood Transfusions
Blood transfusions are lifesaving but come with risks. Knowing these risks is key to keeping patients safe. We’ll talk about the common risks, how to manage them, and why informed consent is so important.
Common Risks of Transfusions
Blood transfusions can cause immune system reactions, spread infectious diseases, and lead to serious issues like TRALI and TACO. Immune system reactions can be mild or severe. Though the chance of getting diseases like HIV and hepatitis is low, it’s not zero.
Some common risks include:
- Allergic reactions
- Hemolytic reactions
- TRALI
- TACO
- Infectious disease transmission
Managing Risks Effectively
To manage transfusion risks, we use a few key strategies. These include screening patients carefully, handling blood products right, and watching patients closely during and after transfusions. We also use advanced tests to lower the risk of disease transmission.
Our effective strategies are:
- Choosing donors carefully
- Testing blood products thoroughly
- Following proper transfusion practices
- Monitoring patients closely
Informed Consent and Patient Education
Informed consent is vital in transfusion medicine. Patients need to know the risks and benefits of blood transfusions. We educate them so they can make informed decisions about their care.
| Risk | Description | Mitigation Strategy |
| Allergic Reactions | Immune system reaction to transfused blood | Premedication with antihistamines |
| Hemolytic Reactions | Destruction of red blood cells due to incompatibility | Strict blood typing and cross-matching |
| TRALI | Non-cardiogenic pulmonary edema | Using male donors for plasma products |
| TACO | Circulatory overload due to transfusion | Transfusing at the lowest effective dose |
By understanding and managing the risks of blood transfusions, we can reduce complications. This ensures the best outcomes for our patients.
Post-Transfusion Care and Monitoring
Post-transfusion care is key to a patient’s recovery. It’s important to watch how the patient reacts to the transfusion. We also need to handle any complications that might come up.
Immediate Post-Transfusion Observations
Right after a transfusion, we keep a close eye on the patient’s vital signs. This includes checking their temperature, blood pressure, and heart rate. Monitoring hemoglobin levels is also a must to see if the transfusion worked.
- Look for signs of transfusion reactions, like fever or rash.
- Make sure the patient is making enough urine to check kidney function.
- Watch how the patient is doing overall, looking for any changes.
Long-Term Monitoring Strategies
Long-term care means regular check-ups to check hemoglobin levels and overall health. We also teach patients about iron-rich diets and lifestyle changes to help them recover.
| Monitoring Aspect | Frequency | Purpose |
| Hemoglobin Levels | After transfusion, then regularly as needed | Check if the transfusion worked and if more are needed |
| Vital Signs | Continuously during transfusion, then regularly post-transfusion | Watch for any bad reactions and overall health |
| Patient Education | Ongoing | Help patients manage their condition |
Handling Possible Complications
Even with careful watching, problems can happen. We’re ready to deal with them, like acute hemolytic reactions or iron overload.
- Spot the problem early by watching closely.
- Start the right treatment.
- Keep supporting and teaching the patient.
By following these steps for post-transfusion care, we can make sure our patients do well. We aim to reduce risks and make sure the transfusion helps them.
Alternatives to Blood Transfusion
There are many ways to manage anaemia without blood transfusions. We look at these options, which include medical treatments and lifestyle changes. These approaches help manage anaemia effectively.
Iron Supplements and Other Treatments
Iron supplements are key for treating iron-deficiency anaemia. We also look at other treatments based on the cause of anaemia.
Iron supplements are available in tablets and intravenous infusions. The choice depends on the severity of the deficiency and the patient’s health.
Erythropoietin Stimulating Agents
Erythropoietin stimulating agents (ESAs) are another option. They help make more red blood cells, easing anaemia.
ESAs are great for patients with chronic diseases like cancer or kidney disease. These diseases often lead to anaemia due to less erythropoietin.
Lifestyle Changes for Managing Anaemia
Medical treatments aren’t the only solution. Lifestyle changes can also help manage anaemia. These include dietary changes, more exercise, and avoiding substances that worsen anaemia.
Eating foods rich in iron, vitamin B12, and folate can help. Good choices include red meat, poultry, fish, beans, lentils, and leafy greens.
украин
| Treatment Option Page Page Page thu Page Page >th | ||
| Description | Benefit | |
| Iron Supplements | Oral Page Page or intravenous iron to treat iron-deficiency anaemia | Effective in treating iron era deficiency, can be used in various patient populations |
| Erythropoietin Stimulating Agents (ESAs) | Stimulate red blood cell production | Useful for Patien patients with chronic diseases like cancer or kidney disease |
| Lifestyle Changes | Dietary adjustments and increased physical activity | Can help manage anaemia, improve overall health |
The Future of Blood Transfusions
The world of transfusion medicine is changing fast. New technologies and research are leading the way. Blood transfusions will keep being key in healthcare, but with big improvements coming.
Advances in Transfusion Medicine
Recently, transfusion medicine has made big strides. Better tests for diseases and better blood matching are now available. Also, how we store and handle blood has improved a lot.
Key Developments:
- Enhanced screening for infectious agents
- Advanced blood component matching
- Innovations in blood product storage
The Role of Technology in Safety
Technology is making blood transfusions safer. Barcode systems and data analytics are key. Artificial intelligence (AI) is also being used to predict how patients will react to transfusions.
These tech advances not only boost safety but also make transfusions more efficient.
| Technological Advancement | Impact on Transfusion Safety |
| Barcode Scanning Systems | Reduces the risk of transfusion errors |
| Data Analytics | Enhances monitoring and management of blood supplies |
| Artificial Intelligence (AI) | Predicts patient responses and improves personalized care |
Potential for Artificial Blood Products
Artificial blood products are an exciting future possibility. Scientists are working on hemoglobin-based carriers and synthetic red blood cells. These could change transfusion medicine by providing new options when blood is hard to find or match.
Though early, artificial blood products show a lot of promise for transfusion medicine’s future.
The future of blood transfusions will blend new tech, medical research, and new products. We’re committed to leading these advancements to give our patients the best care.
Frequently Asked Questions About Anaemia and Transfusions
Frequently Asked Questions About Ana Pageand Transfusions
Patients and families often have Pagequestions about anaemia and transfusions. They want to know the basics and the details of transfusions. We answer some common FAQs on anaemia and transfusions. This includes when you might need a transfusion and other concerns.
Common Concerns and Misconceptions
Many people Pagearea Pageabout the safety and need for blood transfusions. We explain that transfusions are usually needed when hemoglobin levels get too low. But, this can change based on your health.
Understanding ‘common concerns about transfusions’ helps you make better choices.
PageResources for Patients and Families
For those looking for ‘resources for patients with anaemia’, many organizations can help. They offer support, education, and guidance. These Pageresources are key for managing anaemia and transfusion therapy.
We provide detailed information and support. This helps patients and families take charge of their healthcare. They can make informed decisions about their treatment options.
FAQ
What is the lowest hemoglobin level before a blood transfusion is required?
The need for a blood transfusion depends on many factors. These include the patient’s health, symptoms, and the cause of anemia. Usually, a hemoglobin level of 7-8 g/dL is when transfusion is considered.
What are the symptoms that indicate the need for a blood transfusion?
Signs like severe fatigue, shortness of breath, dizziness, and chest pain may mean a transfusion is needed. This is true if the hemoglobin levels are low.
Are there alternatives to blood transfusions for treating anemia?
Yes, there are other options. These include iron supplements, erythropoietin-stimulating agents, and making lifestyle changes. Changes like diet can help manage anemia.
What are the risks associated with blood transfusions?
Blood transfusions can have risks. These include reactions, infections, and iron overload. To manage these risks, blood products are carefully screened and patients are monitored after transfusion.
How is the decision made to transfuse blood in cases of postpartum anemia?
Deciding to transfuse blood in postpartum anemia is based on several factors. These include the severity of anemia, symptoms, and the patient’s overall health. A hemoglobin level of 7 g/dL is often a threshold for considering transfusion.
Can lifestyle changes help manage anemia and reduce the need for blood transfusions?
Yes, making lifestyle changes can help manage anemia. This includes increasing iron intake and other adjustments. These changes can potentially reduce the need for transfusions.
What advancements are being made in transfusion medicine?
Transfusion medicine is advancing. Improvements include better blood screening and the development of artificial blood products. Technology is also being used to make transfusions safer and more efficient.
How is post-transfusion care managed?
After a transfusion, immediate observations for reactions are done. Long-term monitoring for complications is also important. Patients are educated on signs of possible issues.
What hemoglobin level is considered safe for avoiding blood transfusions?
The safe hemoglobin level varies by individual and situation. Generally, levels above 7-8 g/dL are safe for many patients. This depends on symptoms and health status.
Are there different types of blood transfusions available?
Yes, there are different types. Red blood cell transfusions are commonly used. They help increase hemoglobin levels to treat anemia.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db519.htm