Last Updated on November 20, 2025 by Ugurkan Demir
Anemia is a common condition where there’s less hemoglobin and hematocrit. The cut-off values are <12 g/dL in female adults and <13 g/dL in male adults. Often, anemia shows that there’s an underlying autoimmune disease. In these cases, the body’s immune system attacks its own cells.
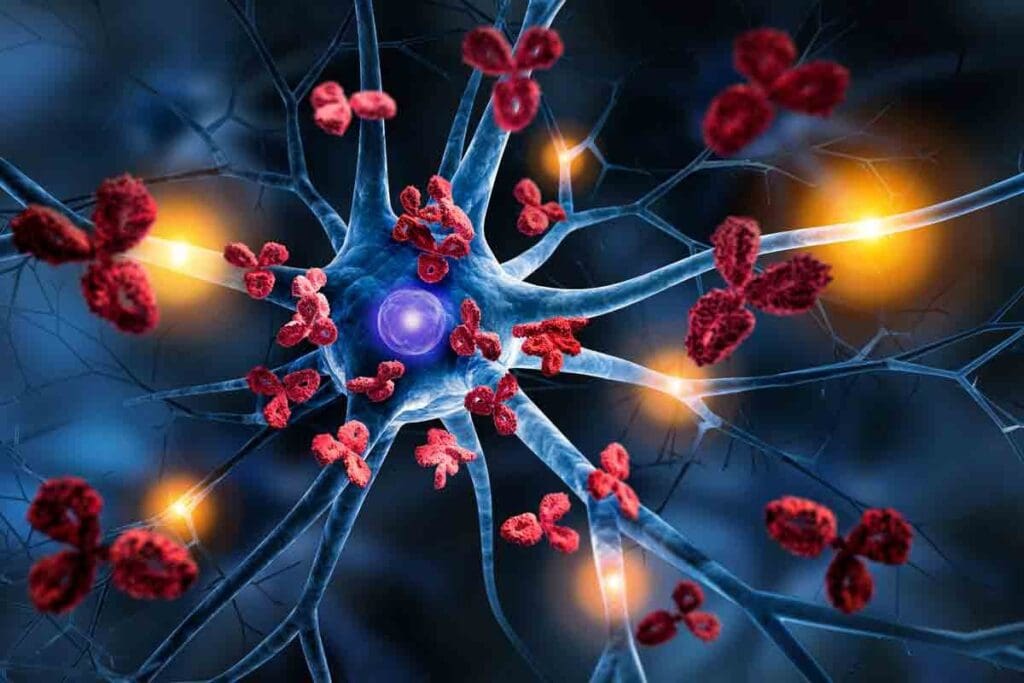
Autoimmune hemolytic anemia (AIHA) is a key example. Here, the immune system targets red blood cells. Understanding anemia autoimmune disease is essential for proper diagnosis and treatment. At Liv Hospital, we focus on patient care and use our expertise to manage complex conditions with confidence.
Anemia is when there are not enough red blood cells or hemoglobin. It’s common and has many causes. Doctors need to know about anemia to treat it well.
Red blood cells carry oxygen all over the body. They have hemoglobin, which picks up oxygen in the lungs and gives it to tissues. This is key to the body’s energy and health. Normal red blood cell function is critical for delivering oxygen to tissues and organs. Any problem with this can cause anemia.
The bone marrow, kidneys, and growth factors work together to make red blood cells. Erythropoietin, made by the kidneys, tells the bone marrow to make more red blood cells. This ensures the body has enough red blood cells.
Anemia is divided into types based on red cell size and hemoglobin. The main types are hypochromic microcytic, normochromic normocytic, and macrocytic anemia. Knowing these types helps find the cause of anemia.
Autoimmune diseases like lupus, rheumatoid arthritis, and inflammatory bowel disease can cause anemia. These diseases lead to anemia of chronic disease (ACD). ACD happens when long-term inflammation messes with iron and red blood cell production.

Anemia and autoimmune diseases are closely linked. This connection involves how the immune system goes wrong and affects blood cells. Autoimmune diseases happen when the body’s immune system attacks itself. This can cause different types of anemia, making the disease harder to treat.
Autoimmune diseases can harm blood cells, leading to anemia. Chronic inflammation is a big problem in these diseases. It messes with how red blood cells are made and how long they last.
Autoimmune hemolytic anemia (AIHA) occurs when the immune system attacks red blood cells. This makes them die off faster, causing severe anemia.
Anemia is common in many autoimmune diseases. For example, rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) often have anemia in their patients.
| Autoimmune Disease | Prevalence of Anemia |
| Rheumatoid Arthritis (RA) | 30-60% |
| Systemic Lupus Erythematosus (SLE) | 20-50% |
| Inflammatory Bowel Disease (IBD) | 20-40% |
“The presence of anemia in patients with autoimmune diseases is not just a simple comorbidity; it reflects the complex interplay between chronic inflammation, immune dysregulation, and hematopoiesis.”
It’s important to know about anemia in autoimmune diseases. By treating both the disease and the anemia, doctors can help patients live better lives.
Anemia of Chronic Disease (ACD) is a complex condition found in people with chronic illnesses. It affects millions worldwide. This condition is caused by changes in how the body uses iron and how long red blood cells last.
To understand ACD, we need to look at its medical definition and related terms. The term “Anemia of Chronic Disease” is often used the same way as “Chronic Disease Anemia.” Both terms describe the same condition.
The AOCD medical term stands for “Anemia of Chronic Disease.” It’s a specific type of anemia linked to chronic illnesses. The AOCD medical abbreviation is used in medical texts and patient records to refer to it briefly.
It’s important to know that AOCD is not a single disease. It’s a complication that can come from many chronic conditions. These include infections, inflammatory diseases, and cancers.
Anemia can be a chronic condition, often linked to chronic diseases. ACD illness refers to the ongoing health issues related to anemia in these cases. Managing ACD means treating both the anemia and the underlying chronic condition.
Because ACD is chronic, patients need long-term management strategies. These strategies aim to alleviate symptoms and improve quality of life.
The ACD medical definition sets it apart from other anemia types. These include iron deficiency anemia and vitamin deficiency anemia. ACD is linked to the body’s response to chronic inflammation or disease.
To better understand the differences, let’s look at a comparison table:
| Anemia Type | Cause | Key Characteristics |
| Anemia of Chronic Disease (ACD) | Chronic inflammation or disease | Reduced iron utilization, increased hepcidin levels |
| Iron Deficiency Anemia | Lack of sufficient iron | Low serum iron, low ferritin |
| Vitamin Deficiency Anemia | Deficiency in vitamins like B12 or folate | Specific vitamin levels are low |
Understanding these differences is key to accurate diagnosis and effective treatment planning.
Chronic disease anemia is complex, affecting how red blood cells are made and live. It’s a common type, often seen in people in the hospital. It’s known as normocytic, normochromic anemia.
Inflammation plays a big role in chronic disease anemia. It leads to the production of cytokines like hepcidin. This disrupts iron use for making red blood cells.
Even with enough iron, the body can’t use it well. This is because of hepcidin, as explained on the National Center for Biotechnology Information website.
The body’s response to make erythropoietin is weak in chronic anemia. This makes fewer red blood cells, making anemia worse.
Chronic inflammation also shortens red blood cell life. This leads to more anemia. It’s another way anemia of chronic disease happens.
| Pathophysiological Mechanism | Description | Effect on Anemia |
| Inflammation-Mediated Iron Sequestration | Disruption of iron homeostasis due to hepcidin production | Functional iron deficiency |
| Impaired Erythropoietin Response | Inadequate erythropoietin production relative to anemia severity | Reduced erythropoiesis |
| Reduced Red Blood Cell Lifespan | Shortened lifespan due to an inflammatory milieu | Increased anemia severity |
Autoimmune Hemolytic Anemia (AIHA) is a condition where the immune system attacks the body’s red blood cells. This can cause severe anemia, fatigue, and other health problems. It’s important to understand AIHA to diagnose and treat it effectively.
AIHA is divided into warm and cold types based on when the autoantibodies are most active. Warm AIHA happens at body temperature, marking red blood cells for destruction. Cold AIHA occurs at lower temperatures.
The causes of warm and cold AIHA are different. Warm AIHA is often linked to other autoimmune diseases. Cold AIHA can be caused by infections or lymphoproliferative diseases. Knowing these differences helps in managing the condition.
Key differences between warm and cold AIHA:
Diagnosing AIHA involves clinical evaluation, laboratory tests, and specialized assays. The direct antiglobulin test (DAT) is key in detecting antibodies or complement proteins on red blood cells.
Managing AIHA requires a personalized approach. Treatment may include corticosteroids, immunosuppressive drugs, and sometimes, splenectomy. For cold AIHA, avoiding cold temperatures is essential.
| Treatment Approach | Warm AIHA | Cold AIHA |
| Corticosteroids | First-line treatment | Limited effectiveness |
| Immunosuppressive drugs | Used in refractory cases | May be considered |
| Splenectomy | Considered for non-responders | Not typically recommended |
| Avoiding cold temperatures | Not applicable | Critical for management |
“The diagnosis of AIHA requires a high index of suspicion and a thorough diagnostic workup, including a direct antiglobulin test (DAT) to detect antibodies or complement on red blood cells.” – Hematology expert
We stress the need for a detailed treatment plan for AIHA. This should address the underlying cause, whether warm or cold AIHA, to improve patient outcomes.
Systemic Lupus Erythematosus (SLE) is a complex autoimmune disease. It affects many parts of the body, including the blood system. Anemia is a common problem for those with SLE.
Anemia in SLE patients comes from different causes. This makes it hard to diagnose and treat. We will look at these causes and how to treat SLE-related anemia.
Anemia in SLE can happen in several ways. These include:
A study in the Lupus journal found anemia in about 50% of SLE patients. This shows the need for detailed blood tests in these patients.
| Mechanism | Description | Key Features |
| Anemia of Chronic Disease (ACD) | Resulting from chronic inflammation | Normocytic or microcytic anemia, elevated ferritin |
| Autoimmune Hemolytic Anemia (AIHA) | Caused by autoantibodies against red blood cells | Positive direct Coombs test, hemolysis markers |
| Impaired Erythropoiesis | Suppression due to chronic inflammation and cytokines | Inappropriately low reticulocyte count |
Managing anemia in SLE patients needs a detailed plan. It must address the causes and the severity of anemia. Treatment options include:
“The management of anemia in SLE involves not only treating the anemia itself but also addressing the underlying autoimmune condition.”
The table below shows how treatment choices depend on the cause of anemia and the patient’s condition.
| Cause of Anemia | First-Line Treatment | Alternative/Additional Treatments |
| Iron Deficiency | Oral iron supplements | IV iron if oral therapy fails |
| Anemia of Chronic Disease | Erythropoiesis-stimulating agents | Addressing underlying inflammation |
| Autoimmune Hemolytic Anemia | Corticosteroids | Immunosuppressants, rituximab |
Understanding the causes of anemia in SLE patients and using the right treatments can improve their lives.
Rheumatoid arthritis is an autoimmune disease that mainly affects the joints. It can also lead to anemia through complex inflammatory pathways. We will look at how this chronic condition causes anemia of chronic disease (ACD) and discuss ways to manage it for patients.
The chronic inflammation in rheumatoid arthritis (RA) is caused by cytokines like tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6). These inflammatory cytokines are key in the development of anemia. They increase hepcidin, a protein that controls iron absorption and release.
High hepcidin levels mean less iron for making red blood cells, leading to anemia. Inflammation also affects erythropoietin production and how red blood cell precursors respond to it. This further contributes to anemia in RA patients.
Managing anemia in RA patients needs a full approach. It must tackle both the arthritis and the anemia. Treatment strategies include:
It’s important to monitor patients for anemia signs and adjust treatments as needed. This helps improve outcomes for RA patients with anemia.
Inflammatory bowel disease (IBD) is linked to anemia through chronic inflammation and poor nutrition. IBD, which includes Crohn’s disease and ulcerative colitis, makes it hard for the body to keep red blood cells healthy.
Anemia is common in IBD patients. It’s caused by blood loss, inflammation, and not getting enough nutrients. We’ll look at these causes and how to treat anemia in IBD patients.
Iron deficiency is a big reason for anemia in IBD patients. The inflammation in the gut can cause blood loss and lower iron levels. Also, IBD makes it hard for the body to absorb iron from food.
Malabsorption is key to anemia in IBD. Inflammation can mess with the gut’s ability to absorb nutrients like iron, vitamin B12, and folate. This makes anemia more likely.
To show how IBD affects nutrient absorption and anemia risk, here’s a table:
| Nutrient | Role in Red Blood Cell Production | Effect of IBD on Absorption |
| Iron | Essential for hemoglobin production | Reduced absorption due to inflammation |
| Vitamin B12 | Critical for red blood cell formation | Impaired absorption, especially in Crohn’s disease affecting the ileum |
| Folate | Necessary for red blood cell production | Malabsorption due to intestinal inflammation |
Dealing with anemia in IBD patients needs a full plan. This plan should tackle inflammation and nutritional gaps. Iron supplementation is often needed to fix iron deficiency anemia.
Here’s a treatment plan that works:
By tackling IBD and anemia, doctors can greatly improve patients’ lives.
Autoimmune diseases can lead to anemia in different ways. It’s important to understand these connections for better management. Some autoimmune conditions are well-known for causing anemia, while others are less recognized but just as significant.
Aplastic anemia is a rare but serious condition where the bone marrow fails to produce blood cells. This happens when the immune system mistakenly attacks the bone marrow. Treatment often involves immunosuppressive therapy to calm the immune system’s attack on the bone marrow, allowing it to resume normal blood cell production.
Understanding the immune system’s role in aplastic anemia is key. This condition shows how autoimmune responses can severely affect blood cell production, leading to severe anemia.
Celiac disease, an autoimmune reaction to gluten, can lead to malabsorption of essential nutrients. This includes iron and vitamin B12, which are critical for red blood cell production. This malabsorption can result in iron deficiency anemia or pernicious anemia, conditions that require careful management through dietary changes and supplementation.
Pernicious anemia is caused by a lack of intrinsic factor, leading to vitamin B12 deficiency. The autoimmune destruction of gastric parietal cells results in reduced intrinsic factor production, necessary for vitamin B12 absorption.
Thyroid disorders, including both hypothyroidism and hyperthyroidism, can affect red blood cell production. Hypothyroidism, for instance, can lead to anemia due to reduced erythropoietin production and decreased iron utilization. Treating the underlying thyroid condition is essential to managing associated anemia.
The complex interplay between thyroid function and red blood cell production highlights the need for thorough care. This includes monitoring for signs of anemia in patients with thyroid disorders.
Diagnosing anemia in patients with autoimmune diseases is complex. It involves many laboratory tests and clinical evaluations. We must understand how the autoimmune condition affects anemia.
Laboratory tests are key in diagnosing anemia of chronic disease (ACD). A complete blood count (CBC) checks hemoglobin and red blood cell indices. Iron studies, es as serum iron and ferritin, also help assess iron levels.
Biomarkers like C-reactive protein (CRP) and erythropoietin levels are important. They show the body’s inflammatory response and how it handles anemia. This helps us understand ACD better and make treatment plans.
Differential diagnosis is vital in managing anemia in autoimmune disease patients. We must tell apart anemia of chronic disease from other anemias. This involves looking at the patient’s history, physical exam, and lab results.
It’s hard to find the main cause of anemia because many factors can play a role. For example, a patient with rheumatoid arthritis might have both ACD and iron deficiency anemia. We need to carefully review lab data and clinical findings to find the main cause.
In some cases, a bone marrow examination is needed to find the cause of anemia. This test looks at bone marrow cells to check their shape, number, and iron stores. It can help diagnose aplastic anemia or myelodysplastic syndromes.
While not always needed, a bone marrow examination gives us important information. It helps us understand the anemia’s cause in autoimmune disease patients and guides treatment.
Managing anemia in chronic disease patients requires a two-step plan. First, treat the underlying autoimmune disease. Then, use specific treatments for anemia. This approach is key to better patient outcomes.
It’s vital to treat the autoimmune disease first. This can help lessen anemia’s impact or stop it from getting worse. Healthcare providers aim to control the disease to improve anemia management.
Iron supplements are often needed to fix an iron deficiency in chronic disease patients. Erythropoiesis-stimulating agents (ESAs) help make more red blood cells. They’re useful when the body doesn’t make enough erythropoietin.
Blood transfusions might be needed for severe anemia. They quickly raise red blood cell counts. New treatments and targeted therapies are also being explored for anemia in chronic disease patients.
Living with chronic anemia and autoimmune conditions needs a full plan. This plan includes medical care and changes in how we live. We know that handling anemia and autoimmune diseases well can really boost our quality of life.
By tackling the root cause of the autoimmune condition, adding iron and special medicines, and changing our diet, we can manage anemia better. Teaching patients about their condition is also key.
We stress the need for a complete approach to handle anemia linked to autoimmune diseases. This includes treatments, lifestyle changes, and support to improve our overall health and life quality.
Anemia of chronic disease (ACD) happens in people with long-term illnesses. This includes autoimmune diseases, infections, or cancer. It’s caused by less red blood cell production due to inflammation and immune system issues.
Autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus (SLE) can lead to anemia. Inflammatory bowel disease (IBD) and autoimmune hemolytic anemia (AIHA) also cause it.
Inflammation can lower red blood cell production. It does this by reducing iron, affecting erythropoietin production, and shortening red blood cell lifespan.
ACD happens in people with long-term illnesses. Iron deficiency anemia is due to not enough iron. Both can cause anemia, but have different causes and treatments.
Anemia can be long-term, often in people with autoimmune or chronic illnesses. But, with the right treatment, it can be managed to improve life quality.
AOCD stands for Anemia of Chronic Disease. It’s a medical term and abbreviation for this condition.
Diagnosing anemia in autoimmune patients involves tests like complete blood counts (CBCs) and iron studies. A physical exam and medical history are also key.
Treating anemia in chronic disease includes managing the underlying condition. Treatment also includes iron supplements, erythropoiesis-stimulating agents, blood transfusions, and new therapies.
Yes, AIHA can be treated. Medications like corticosteroids are used to suppress the immune system. Blood transfusions or other therapies may also be needed.
Rheumatoid arthritis can cause anemia of chronic disease. It does this by producing inflammatory cytokines. These cytokines lead to iron sequestration and impaired erythropoiesis.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!