Last Updated on November 14, 2025 by Ugurkan Demir

Patients with advanced chronic kidney disease (CKD) often face a complex condition known as anemia of chronic renal failure. This affects up to 90% of them.
This condition means the body doesn’t have enough healthy red blood cells. These cells are needed to carry oxygen to the body’s tissues. Symptoms include weakness and fatigue. It’s important to understand the causes and treatments of anemia in renal failure to manage it well.
Anemia is a common problem for people with CKD. It makes their quality worse. It happens when there are fewer red blood cells or less hemoglobin in the blood. This means tissues and organs don’t get enough oxygen.
Anemia in CKD happens when the kidneys can’t make enough erythropoietin. This hormone helps make red blood cells. Without enough, patients feel tired, weak, and short of breath. These symptoms make it hard to do everyday things.
Anemia in CKD is serious because it affects how well patients do. It can make CKD worse, increase heart problems, and lower the quality of life. This is why treating anemia is so important.
Anemia is very common in CKD patients, more so in stages 3-5. As CKD gets worse, more people develop anemia. This shows how important it is to catch and treat anemia early.
Research shows anemia affects about 10% of CKD patients in the early stages. But in advanced stages, it affects nearly 75% or more. This highlights the need for early detection and treatment to help patients.
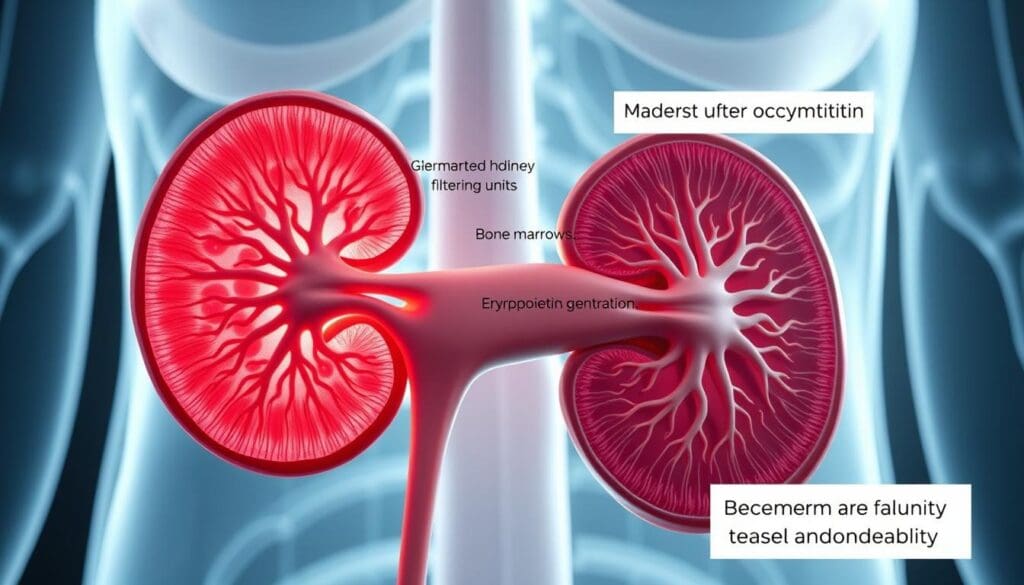
It’s important to know how the kidneys affect red blood cell production. This is key to understanding anemia in chronic kidney disease (CKD). The kidneys help keep our red blood cell count right by making erythropoietin, a hormone.
Erythropoiesis is how our body makes red blood cells. It involves many steps and cells working together. Erythropoietin, made by the kidneys, is a big player in this process. It helps grow and change cells in the bone marrow into red blood cells.
In healthy people, the kidneys make just the right amount of erythropoietin. This keeps the number of red blood cells stable. The kidneys make more erythropoietin when we need more oxygen, helping our body adjust.
CKD patients have trouble making erythropoietin. This means they don’t make enough red blood cells. This is a main reason for anemia in these patients. How bad the anemia is can depend on how well the kidneys work.
Chronic inflammation and iron deficiency also make anemia worse in CKD patients. These issues affect how well red blood cells are made and how much iron is available. Knowing about these problems helps doctors treat anemia better in patients with chronic kidney disease.
Chronic kidney disease often leads to anemia in patients. This condition has many symptoms that make life harder. Anemia of chronic renal failure affects red blood cell production and overall health.
Anemia in CKD patients shows in many ways. These symptoms can really hurt their quality of life. Here are some common ones:
Anemia’s symptoms can affect both physical and mental abilities in CKD patients. Physical limitations come from constant tiredness, making simple tasks hard. Mental problems, like trouble focusing and remembering things, can also happen because of a lack of brain oxygen.
| Symptom | Impact on Patients |
| Fatigue | Reduces the ability to perform daily activities |
| Cognitive Impairment | Affects concentration and memory |
| Dizziness and Shortness of Breath | Increases risk of falls and reduces exercise tolerance |
It’s key to know these symptoms to manage anemia in CKD patients well. By tackling the causes and symptoms, doctors can help patients live better lives and have better health outcomes.
Getting a correct diagnosis of anemia in chronic kidney disease (CKD) is key. It helps in managing the condition well. Doctors use both clinical checks and lab tests to find out how severe and why anemia is happening.
Lab tests are very important in finding anemia in CKD patients. They look at:
These tests help doctors figure out the type and how severe anemia is. This guides them in choosing the right treatment for the management of anaemia in CKD.
When looking at anemia in CKD patients, other reasons for anemia must be thought of, too. These include iron deficiency, vitamin deficiency anemia, anemia of chronic disease, and other conditions that might be present with CKD.
A detailed diagnostic process is needed to find the real cause of anemia. This might mean doing more tests, like:
By looking closely at lab results and thinking about other possible causes, doctors can create specific treatment plans. This helps improve how well patients do witthe h the treatment of anemia of chronic kidney disease.
Anemia of renal insufficiency is a complex condition with various contributing factors. Chronic kidney disease (CKD) leads to anemia through multiple mechanisms. It’s essential to understand these causes for effective management.
One of the primary causes of anemia in CKD is the reduced production of erythropoietin. This hormone is made by the kidneys and helps make red blood cells. As kidney function declines, erythropoietin production decreases, leading to a reduction in red blood cell production.
Iron deficiency is another significant cause of anemia in CKD patients. This can result from inadequate dietary intake, chronic blood loss during dialysis, or impaired iron absorption. Disorders in iron metabolism, such as those caused by inflammation, can further contribute to anemia.
Chronic inflammation is common in CKD patients and can lead to anemia. It disrupts iron metabolism and suppresses erythropoiesis. Pro-inflammatory cytokines can directly inhibit the production of red blood cells and interfere with the body’s response to erythropoietin.
Uremic toxins, which accumulate as kidney function declines, can also contribute to anemia. These toxins can inhibit erythropoiesis and reduce the lifespan of red blood cells, further exacerbating anemia.
The interplay of these factors highlights the complexity of anemia associated with chronic kidney disease. Understanding these causes is key to developing effective treatment strategies.
Managing anemia in CKD requires a holistic approach. By understanding the underlying mechanisms, healthcare providers can develop targeted treatment plans. This improves patient outcomes.
Hepcidin’s impact on iron metabolism is key in CKD anemia. Anemia is common in CKD patients. Knowing hepcidin’s role helps in finding better treatments.
Hepcidin is a protein that controls iron in our bodies. It affects how we absorb iron from food and release it from stores. High hepcidin levels mean less iron for making blood cells.
Key Functions of Hepcidin:
In CKD, hepcidin levels go up because of chronic inflammation. This makes it hard for the body to use iron for making blood cells. So, iron therapy alone may not work well for CKD patients.
The link between hepcidin and CKD anemia is complex. It involves inflammation, iron use, and how the body makes erythropoietin.
| Factor | Effect on Hepcidin | Impact on Anemia |
| Chronic Inflammation | Increases hepcidin levels | Contributes to functional iron deficiency |
| Iron Deficiency | Typically decreases hepcidin | It can cause anemia if not treated |
| Erythropoietin Production | Indirectly affected by hepcidin through iron availability | Influences erythropoiesis and anemia severity |
Understanding hepcidin’s role in CKD anemia is important for treatment. Targeting hepcidin or its pathways could help manage anemia in CKD patients.
ESAs have greatly improved the treatment of anemia in CKD. They are key in starting the process of making new red blood cells. ESAs are a mainstay in treating anemia linked to chronic kidney disease. They help fix the problem in a focused way.
There are different ESAs like epoetin alfa, epoetin beta, and darbepoetin alfa. They can be given through an IV or under the skin. The choice depends on the patient’s needs and the doctor’s preference.
“The use of ESAs has been shown to improve quality of life and reduce the need for blood transfusions in patients with CKD-related anemia,” as noted in clinical guidelines.
Dosing ESAs depends on the patient’s hemoglobin, iron levels, and health status. It’s important to check these regularly. This helps adjust the dose to avoid side effects.
While ESAs are mostly safe, there are risks like high blood pressure and heart problems. It’s important to carefully choose patients and monitor them closely to avoid these risks.
A leading nephrologist says, “The benefits of ESAs in managing anemia in CKD must be balanced against the possible risks. This requires a treatment plan tailored to each patient.”
Iron therapy is key in treating anemia linked to chronic kidney disease (CKD). Anemia is common in CKD patients due to less erythropoietin and iron. Giving iron helps fix these issues and boosts red blood cell production.
Choosing between oral and intravenous iron depends on several factors. These include how severe the iron deficiency is, how well the patient can take it, and any health issues that might affect iron absorption. Oral iron is usually the first choice because it’s easy to take and cheaper. But intravenous iron might be better for severe cases or when oral iron doesn’t work.
It’s important to keep an eye on iron levels to avoid too much iron. This can cause serious health problems. Checking iron levels, ferritin, and transferrin saturation regularly helps adjust treatment. This ensures the patient gets enough iron without risking overload.
| Parameter | Target Range | Clinical Significance |
| Serum Ferritin | 200-500 ng/mL | Indicative of iron stores; helps in assessing the risk of iron overload. |
| Transferrin Saturation | 20-50% | Reflects the availability of iron for erythropoiesis. |
| Hemoglobin | Typically >10 g/dL | Target level may vary based on individual patient needs and clinical guidelines. |
Effective iron therapy for renal disease anemia needs a careful balance. It’s about weighing the benefits and risks of different methods. By closely watching iron levels and adjusting treatment, doctors can improve patient outcomes and quality of life.
New ways to treat anemia in chronic kidney disease (CKD) are being explored. These methods aim to improve the lives of patients with CKD.
Nutrition is key in fighting anemia linked to CKD. It’s important to get enough iron, vitamin B12, and folate for making red blood cells. Vitamin supplements can help if these nutrients are lacking.
Eating a balanced diet is essential. Foods rich in iron, vitamin B12, and folate are recommended. Sometimes, dietary supplements are needed to fill nutritional gaps.
| Nutrient | Food Sources | Role in Erythropoiesis |
| Iron | Red meat, leafy greens | Essential for hemoglobin production |
| Vitamin B12 | Animal products | Critical for red blood cell formation |
| Folate | Legumes, citrus fruits | Necessary for DNA synthesis in red blood cells |
New treatments for anemia in CKD are being researched. One area is the use of HIF-PHIs (Hypoxia-Inducible Factor Prolyl Hydroxylase Inhibitors). These help make more red blood cells by mimicking the body’s natural response to low oxygen.
Improving dialysis methods is important to reduce blood loss. Using biocompatible dialysis membranes and avoiding invasive procedures are key.
By using these advanced treatments, doctors can better manage anemia in CKD. This leads to better health outcomes for patients.
Managing anemia in chronic kidney disease needs a full approach. This includes using ESAs, iron supplements, and fixing nutritional gaps.
Marg
Anemia in chronic kidney disease is a complex issue. It happens when the body makes fewer red blood cells. This is due to less erythropoietin, iron deficiency, and chronic inflammation.
Marg
Marg
Treating anemia in CKD patients is key. It boosts hemoglobin levels and improves life quality.
Marg
Marg
Managing anemia in CKD requires a team effort. It involves ESAs, iron therapy, and nutritional support.
ars
The rewritten and refined output is
Here is the HWND finalider output that is putiderin the Essener required format
roller
Here is the UML rewritten and refined output that I put iinthe Essener required format.
Marg
Anemia of chronic renal failure is a condition where red blood cells or hemoglobin decrease. It happens in people with chronic kidney disease (CKD). This is mainly because the kidneys can’t make enough erythropoietin.
Anemia is very common in CKD patients. It affects a lot of people, mostly those in later stages of the disease.
The main causes of anemia in CKD include several factors. These are reduced erythropoietin production, iron deficiency, and chronic inflammation. Uremic toxins, hepcidin dysregulation, nutritional deficiencies, and blood loss during dialysis also play a role.
Erythropoietin is a hormone made by the kidneys that helps make red blood cells. In CKD, the kidneys can’t make enough of it. This leads to fewer red blood cells and anemia.
Hepcidin is a protein that controls iron use. In CKD, high hepcidin levels can lock up iron. This makes less iron available for making red blood cells, causing anemia.
Doctors use tests like complete blood counts (CBC), iron studies, and erythropoietin levels to diagnose anemia. These tests help find out how severe the anemia is and what’s causing it.
Treatments include erythropoiesis-stimulating agents (ESAs), iron supplements, and nutritional plans. They also work on dialysis to reduce blood loss.
ESAs might increase the risk of heart problems, stroke, and tumor growth. So, it’s important to watch patients closely.
Iron therapy checks iron levels to avoid too much. It uses oral or intravenous iron, based on how severe the deficiency is and what the patient needs.
Yes, nutritional plans can help. They include vitamin supplements to address deficiencies that might cause anemia.
New treatments include drugs that target hepcidin and other anemia causes. They also aim to improve dialysis to reduce blood loss.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!