Last Updated on November 26, 2025 by Bilal Hasdemir

Managing airways is key in today’s surgery. It ensures safe general anesthesia and keeps oxygen flowing. Intubation is important for keeping the airway open, letting oxygen in and stopping food from going into the lungs.
Anesthesia and intubation are key parts of safe surgical care. Liv Hospital is all about keeping patients safe and using the latest methods. They make sure your airway is in good hands. Good airway care is vital for surgery success, showing how important skilled doctors are in this field.
Key Takeaways
- Airway management is critical in modern surgery for patient safety.
- General anesthesia requires careful airway management.
- Intubation is a key procedure for securing the airway.
- Liv Hospital prioritizes patient safety with advanced protocols.
- Effective airway management is essential for successful surgery.
Understanding the Fundamentals of Airway Management
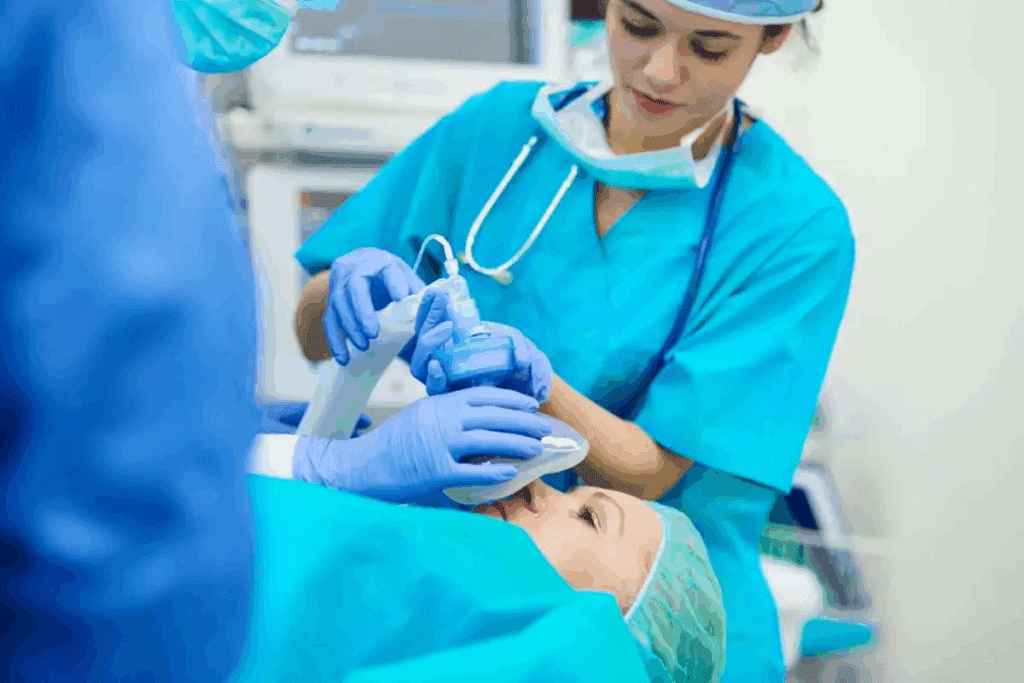
Airway management is key in giving general anesthesia during surgery. It makes sure air can flow freely between the lungs and the outside. This is vital for getting enough oxygen and breathing well.
The Role of Airway Management in Modern Surgery
Airway management is very important in today’s surgeries. It’s most critical in surgeries needing general anesthesia and intubation. Here, keeping the airway safe is a top priority. Research shows over 70 percent of general anesthesia cases use intubation for safety.
Managing the airway in surgery is complex. It involves more than just knowing how to intubate. It also means understanding the patient’s body, how it works, and the possible problems that could happen.
Key Components of Successful Airway Management
For airway management to be successful, several things are important. These include:
- Pre-anesthetic assessment: Checking the patient’s airway and health to spot any possible issues.
- Appropriate equipment preparation: Making sure all needed tools, like endotracheal tubes and laryngoscopes, are ready and work well.
- Skilled personnel: Having trained people who can handle the airway well.
Indications for Endotracheal Intubation
Endotracheal intubation is needed in many situations. These include:
- Surgeries needing general anesthesia, where keeping the airway safe is critical.
- Patients who might have trouble breathing because of their health or the surgery.
- Cases where breathing support is needed for a long time.
Knowing when to use endotracheal intubation is key for good airway management. It helps doctors get ready and deal with any problems early on.
Pre-Anesthetic Assessment and Planning

Effective airway management starts with a detailed pre-anesthetic assessment. This step is key to keeping patients safe during general anesthesia intubation. It involves checking the patient’s medical history, examining the airway, and spotting any possible issues during intubation.
Patient History Evaluation
Looking into a patient’s history is vital in pre-anesthetic assessment. It means checking past anesthetic records, noting any tough intubation history, and looking at the patient’s overall health. A top anesthesiologist says, “The key to successful airway management lies in meticulous planning and preparation.”
Important things to think about in patient history evaluation include:
- Previous anesthetic experiences and outcomes
- Known allergies and sensitivities
- Existing medical conditions that could impact airway management
Airway Examination Techniques
Airway examination is a key part of pre-anesthetic assessment. Methods like the Mallampati classification, measuring thyromental distance, and checking neck mobility help assess intubation ease. airway assessment.
A detailed airway check can show issues like small mouth opening or stiff neck. These are important to spot before starting intubation.
Identifying Potentail Difficult Airways
Spotting possible difficult airways is a key part of pre-anesthetic planning. It uses info from patient history and airway check to predict challenges.
“The ability to predict a difficult airway is as important as the ability to manage it.”
For managing expected difficult airways, having backup plans and being ready for complications is important.
By carefully looking at patient history, doing detailed airway checks, and spotting possible difficult airways, healthcare providers can make general anesthesia intubation safer and more effective.
Equipment Preparation for Anesthesia and Intubation
Getting equipment ready is key for safe anesthesia and intubation. It helps healthcare teams work well together. This makes the procedure smoother and safer for everyone.
Essential Equipment Checklist
Before starting, a detailed checklist is essential. It lists all the must-have tools. These include:
- Endotracheal tubes of various sizes
- Laryngoscopes with different blade types and sizes
- Stylets and bougies
- Anesthesia machine with ventilator
- Monitoring equipment (ECG, pulse oximeter, capnograph)
Table 1: Essential Equipment for Anesthesia and Intubation
| Equipment | Description | Importance |
| Endotracheal Tube | Tube inserted into the trachea for airway management | High |
| Laryngoscope | Instrument used to visualize the vocal cords | High |
| Anesthesia Machine | Device that delivers anesthetic gases and ventilates the patient | Critical |
Endotracheal Tube Selection and Preparation
Choosing the right endotracheal tube (ETT) size and type is critical. The tube must be checked for damage. The cuff should also be tested for leaks. Proper preparation of the ETT means it’s sterile and the cuff works right.
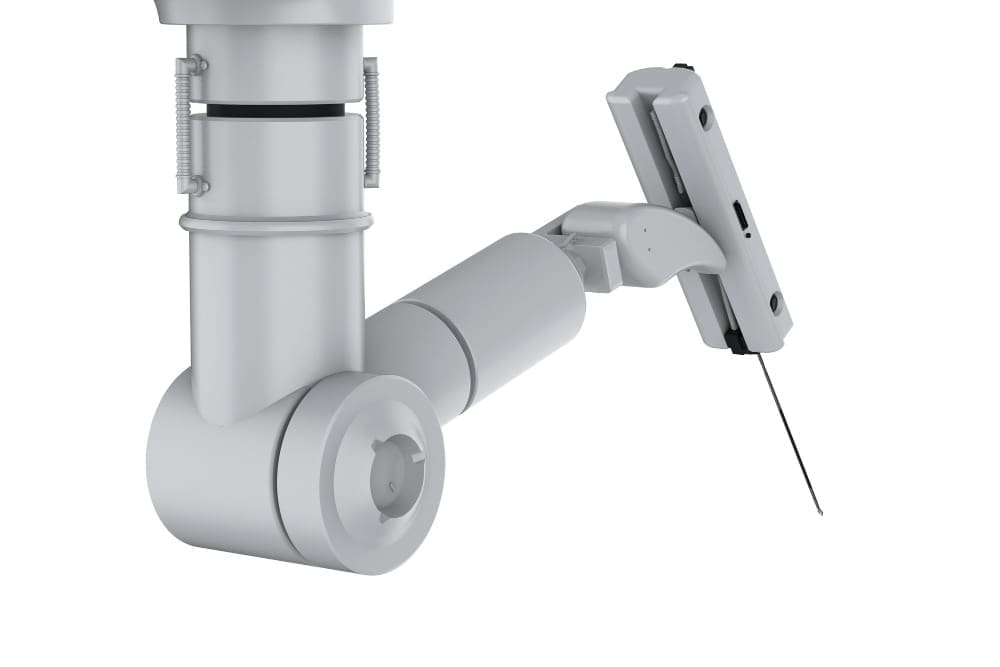
Laryngoscope Types and Selection
Laryngoscopes vary, like Macintosh and Miller blades, each with benefits. The right choice depends on the patient and the doctor’s style. Proper selection and preparation of the laryngoscope are key for clear airway views.
By following these steps and making sure all equipment is ready, healthcare teams can reduce risks. This leads to better care for patients.
Patient Positioning for Optimal Intubation
Getting the patient in the right position is key in airway management during anesthesia. It’s important for successful intubation. The right position helps align the airway axes, making the process easier and safer.
The Sniffing Position Technique
The sniffing position is a common technique for intubation. It involves bending the neck and tilting the head. This makes it easier to insert the laryngoscope and endotracheal tube.
To achieve this, a pillow or sheet is placed under the patient’s head and sometimes shoulders. This depends on the patient’s body shape.
Key elements of the sniffing position include:
- Flexion of the neck to align the pharyngeal and laryngeal axes
- Extension of the head at the atlanto-occipital joint to align the oral axis with the other two
- Careful adjustment to avoid excessive strain on the patient’s neck
Modifications for Special Populations
Some patients need special adjustments to the sniffing position. For example, obese or pregnant patients might benefit from a ramped position. This position helps improve lung capacity and makes intubation easier.
Special considerations include:
- Patients with cervical spine injuries or conditions that limit neck flexion
- Pregnant patients in their third trimester, who may require a wedge or ramp to improve respiratory mechanics
- Obese patients, who may benefit from a ramped position to enhance lung volumes
Ramping Techniques for Difficult Airways
Ramping techniques involve lifting the patient’s upper body. This makes the airway axes more aligned. It’s helpful for patients with difficult airways, as it improves the view during intubation.
Benefits of ramping include:
- Improved laryngoscopic view
- Enhanced patient comfort during the procedure
- Better alignment of the airway axes, facilitating easier intubation
Pre-Oxygenation Techniques and Protocols
Ensuring patient safety during intubation is key. Pre-oxygenation fills oxygen reserves before the procedure. This prevents hypoxia.
Standard Pre-Oxygenation Methods
High-flow oxygen therapy through a tight-fitting face mask is a standard method. It denitrogenates the lungs and fills them with oxygen.
Key steps in standard pre-oxygenation:
- Administer 100% oxygen for 3-5 minutes
- Ensure a tight seal with the face mask
- Monitor end-tidal oxygen levels
Optimizing Oxygen Reserves
It’s important to optimize oxygen reserves, more so in patients with reduced respiratory capacity. Techniques like non-invasive ventilation (NIV) or high-flow nasal cannula (HFNC) oxygen therapy can be used.
“Pre-oxygenation is not just about delivering oxygen; it’s about maximizing the patient’s oxygen reserves to ensure safety during the apneic period.” – Dr. John Smith, Anesthesiologist
| Technique | Oxygen Flow Rate | Duration |
| High-Flow Oxygen Therapy | 10-15 L/min | 3-5 minutes |
| Non-Invasive Ventilation (NIV) | Varies | 3-5 minutes |
Monitoring Effectiveness of Pre-Oxygenation
It’s vital to monitor pre-oxygenation’s effectiveness. End-tidal oxygen monitoring gives real-time feedback on oxygenation status.
Special Considerations for High-Risk Patients
High-risk patients, like those with obesity or respiratory disease, need special care. Rapid sequence intubation (RSI) with pre-oxygenation can be beneficial.
Understanding and applying these pre-oxygenation techniques and protocols can greatly improve patient safety during intubation.
Induction of General Anesthesia
Starting general anesthesia is key. It needs a deep understanding of anesthetics and patient health. This step is vital for the patient’s safety and comfort during surgery.
Selecting Appropriate Induction Agents
The right induction agent depends on many things. These include the patient’s medical history, current health, and the surgery type. Etomidate, fentanyl, and propofol are common choices. Each is picked based on the patient’s needs and the anesthesiologist’s preference.
Dosing Considerations and Adjustments
Choosing the right dose of anesthetic is important. The patient’s age, weight, and liver or kidney health matter. Adjustments may be needed to ensure a safe and smooth start.
Monitoring During Induction Phase
Keeping an eye on the patient during induction is essential. This means watching heart rate, blood pressure, and oxygen levels. The anesthesiologist must be ready to act fast if anything changes.
Rapid Sequence Induction Protocol
Rapid sequence induction (RSI) is used when there’s a high risk of food going into the lungs. It quickly gives an anesthetic and then a muscle relaxant to help intubate. The aim is to quickly secure the airway to prevent aspiration.
Rapid sequence induction needs careful planning and skill. It’s often used in emergencies or when there’s a risk of food aspiration. The anesthesiologist must be well-trained in this method to handle any issues that might arise.
The Science of Anesthesia and Intubation
Anesthesia and intubation involve many scientific principles. These are key for safe airway management.
Physiological Effects of General Anesthesia
General anesthesia impacts the body in many ways. It affects breathing and heart functions. Knowing these effects is vital for patient care.
As a study in a medical journal noted, “General anesthesia’s impact on breathing can be big. Anesthesiologists need to handle these changes well.”
“General anesthesia slows down breathing, reducing the amount of air inhaled and exhaled.”
Pharmacokinetics of Anesthetic Agents
The way anesthetics work is important for their safety and effectiveness. How they spread, break down, and leave the body affects how long and deep the anesthesia lasts. Anesthesiologists must think about these factors when choosing and using anesthetics.
- Distribution: How the anesthetic spreads in the body.
- Metabolism: The process of breaking down the anesthetic.
- Elimination: How the anesthetic is removed from the body.
Evidence-Based Practices in Modern Intubation
Today’s intubation methods are backed by research to improve patient results. Video laryngoscopy is gaining popularity for its better success rates.
Statistical Safety Profiles of Different Techniques
Research has looked at the safety of different intubation methods. For instance, a study showed video laryngoscopy works better on the first try than direct laryngoscopy.
“Video laryngoscopy lowers the risk of hard intubations and improves seeing the vocal cords.”
| Technique | Success Rate | Complication Rate |
| Direct Laryngoscopy | 80% | 15% |
| Video Laryngoscopy | 95% | 5% |
Neuromuscular Blockade for Intubation
Neuromuscular blockade is key for making endotracheal intubation easier by relaxing muscles. It’s vital for keeping the patient’s airway safe and ready for intubation.
Types of Neuromuscular Blocking Agents
There are two main types of neuromuscular blocking agents: depolarizing and non-depolarizing. Depolarizing agents, like succinylcholine, act like acetylcholine at the neuromuscular junction. This causes muscle contraction followed by long-lasting relaxation. Non-depolarizing agents, such as rocuronium and vecuronium, block acetylcholine receptors. This leads to muscle paralysis without the initial contraction.
Timing of Administration
When to give neuromuscular blocking agents is very important for successful intubation. They are given after the patient is fully anesthetized. The time it takes for these agents to work varies. For example, succinylcholine works fast, while rocuronium takes a bit longer. It’s important to check how well the blockade is working to know when to intubate.
Assessing Adequate Blockade
To check if the blockade is strong enough, peripheral nerve stimulation is used. This involves stimulating a nerve and watching the muscle response. The blockade’s strength is measured by how many twitches there are in response to stimulation. For intubation, the goal is to have very few or no twitches.
Reversal Agents and Their Application
After surgery, reversal agents are used to bring back muscle function. Neostigmine and sugammadex are common reversal agents. Neostigmine increases acetylcholine levels to reverse the blockade. Sugammadex, on the other hand, binds to rocuronium and vecuronium to reverse their effects. The right reversal agent depends on the neuromuscular blocking agent used and the patient’s health.
Step-by-Step General Anesthesia Intubation Procedure
Managing airways during general anesthesia and intubation needs a careful step-by-step plan. This ensures the procedure is done safely and well, reducing risks to the patient.
Laryngoscopy Technique
Laryngoscopy is a key step in intubation, needing precision and care. The laryngoscopy technique involves inserting the laryngoscope into the patient’s mouth. It then goes to the oropharynx and gently lifts to show the glottis. Proper positioning is key for clear vocal cord view.
The type of laryngoscope blade used depends on the patient’s anatomy and the anesthesiologist’s choice. Blades like Macintosh and Miller are commonly used, each with its own benefits.
Endotracheal Tube Placement
After the glottis is seen, the next step is endotracheal tube placement. The tube is inserted through the vocal cords into the trachea. It’s important to avoid touching nearby structures to prevent trauma and complications.
The tube is moved until the cuff is just past the vocal cords. Then, the cuff is inflated to seal the airway. This keeps the tube in place and prevents leaks.
Confirmation of Proper Tube Position
Confirmation of proper tube position is essential to ensure the tube is correctly placed in the trachea. This is done through a mix of clinical checks and technology.
- Clinical signs include end-tidal CO2, bilateral breath sounds, and chest rise.
- Technology like capnography gives a clear sign by showing CO2 in exhaled breath.
Checking tube placement is a critical safety step. Wrong placement can cause serious issues, like hypoxia and airway trauma.
Managing Difficult Airways and Complications
Managing difficult airways and complications needs a detailed plan. This includes spotting hard airways, trying different ways to intubate, and having a backup plan for failed intubation.
Recognizing a Difficult Airway
The first step is to spot a difficult airway. Look at the patient’s airway structure. Check for signs like hard neck movement, big tongue, or small jaw.
Key signs of a hard airway include:
- Limited mouth opening
- High Mallampati score
- Thyromental distance
- Neck mobility issues
Alternative Intubation Strategies
When a difficult airway is found, try different ways to intubate. Use a video laryngoscope, flexible fiberoptic bronchoscopy, or other advanced methods.
| Technique | Description | Advantages |
| Video Laryngoscopy | Uses a camera to see the airway | Clear view, easier to intubate |
| Flexible Fiberoptic Bronchoscopy | Can go through tricky airways | Works well in hard airways |
Failed Intubation Protocol
A failed intubation plan is key when intubation doesn’t work. It should include getting help, using other airway tools, and being ready for emergency surgery.
Emergency Surgical Airway Techniques
If all else fails, emergency surgery might be needed. This includes cricothyrotomy, making an airway through the cricothyroid membrane.
Steps for cricothyrotomy:
- Find the cricothyroid membrane
- Make a vertical cut
- Put in a tracheostomy or endotracheal tube
- Secure the tube
Ventilation Management with Breathing Tubes
Managing ventilation with breathing tubes is a complex task. It requires careful attention to several key factors. This ensures patient safety and the best outcomes during general anesthesia.
Initial Ventilator Settings
Setting the initial ventilator settings is critical. You need to choose the right tidal volume, respiratory rate, and positive end-expiratory pressure (PEEP). Tidal volume should be between 6-8 mL/kg of ideal body weight to prevent lung injury.
The respiratory rate must be adjusted based on the patient’s CO2 production and ventilation needs. A good starting point is 12-15 breaths per minute.
Monitoring Respiratory Parameters
It’s essential to continuously monitor respiratory parameters. This ensures the patient is getting enough ventilation. You should watch end-tidal CO2 (ETCO2), oxygen saturation, and peak airway pressures.
ETCO2 monitoring helps check the patient’s ventilatory status. It can show issues like hypoventilation or hyperventilation.
| Parameter | Normal Range | Clinical Significance |
| Tidal Volume | 6-8 mL/kg | Adequate lung ventilation |
| Respiratory Rate | 12-15 breaths/min | Maintains normocapnia |
| PEEP | 5-10 cmH2O | Prevents atelectasis |
Adjusting Ventilation Based on Patient Needs
Adjusting ventilation settings is vital. It may involve changing tidal volume, respiratory rate, or PEEP levels. These changes should be based on the patient’s clinical status.
Troubleshooting Common Breathing Tube Issues
Common issues like tube obstruction, kinking, or displacement must be quickly identified and fixed. Regular checks of the tube position and patency are key.
In cases of tube obstruction, suctioning may be needed to clear secretions. If the tube is kinked, repositioning the tube or patient may solve the problem.
Extubation Process and Post-Anesthesia Care
The extubation process is a key part of patient care. It’s when a patient moves from needing a breathing machine to breathing on their own. It’s important to plan and execute it carefully to ensure safety and success.
Criteria for Safe Extubation
For safe extubation, a patient must meet certain criteria. They need stable vital signs, good oxygenation, and the ability to protect their airway. Doctors must check these carefully to avoid problems.
Extubation Techniques
There are different ways to extubate a patient, but the main goal is to remove the tube safely. Steps like pre-extubation suctioning and patient preparation are key. Using the right techniques can help avoid complications.
Post-Extubation Monitoring
After extubation, it’s important to watch the patient closely. Look for signs of respiratory distress, oxygen saturation, and comfort. Good care after extubation helps with a smooth recovery.
Managing Post-Extubation Complications
Even with careful planning, complications can happen after extubation. Issues like laryngospasm or reintubation needs can occur. It’s important to have a clear plan for these situations. Doctors need to be ready to act quickly and effectively.
Conclusion
Airway management is key in surgery, keeping patients safe under general anesthesia and intubation. It’s vital for healthcare workers to know how to handle airways well. This knowledge helps them deal with the challenges of anesthesia care.
This guide shows how important a full approach to airway management is. By learning these steps, healthcare pros can lower risks and improve patient results.
Good airway management needs a strong grasp of physiology, pharmacology, and technical skills. When these are combined, doctors can give top-notch care. This ensures the best outcomes for patients going through surgery.
FAQ
What is the primary purpose of airway management in general anesthesia?
Airway management in general anesthesia ensures a safe airway for the patient. It allows for safe breathing and protects against aspiration during surgery.
What is general anesthesia intubation?
General anesthesia intubation is a procedure where a breathing tube is inserted into the patient’s airway. It helps with ventilation and keeps the airway secure during anesthesia.
Why is pre-anesthetic assessment important before intubation?
Pre-anesthetic assessment is key before intubation. It helps identify any airway challenges and reviews the patient’s medical history. It also guides the choice of airway management strategies.
What are the key components of successful airway management?
Successful airway management includes a thorough pre-anesthetic assessment and proper patient positioning. It also involves effective pre-oxygenation and the use of the right equipment, like endotracheal tubes and laryngoscopes.
What is the role of neuromuscular blockade in intubation?
Neuromuscular blockade relaxes muscles, making it easier to insert the breathing tube. It ensures a secure airway during intubation.
How is the effectiveness of pre-oxygenation monitored?
The success of pre-oxygenation is checked by looking at oxygen saturation levels and end-tidal oxygen concentration. It also involves ensuring the patient has enough oxygen.
What are the indications for endotracheal intubation?
Endotracheal intubation is needed for general anesthesia, airway protection, and mechanical ventilation. This is during surgery or in critically ill patients.
What is the sniffing position technique used for?
The sniffing position technique is used to position the patient for intubation. It aligns the oral, pharyngeal, and laryngeal axes to make tube insertion easier.
How is the proper position of the endotracheal tube confirmed?
The endotracheal tube’s correct position is confirmed through clinical assessment and capnography. Capnography detects end-tidal carbon dioxide, ensuring the tube is in the right place.
What are the common complications associated with intubation?
Intubation can lead to complications like difficult intubation, airway trauma, and aspiration. Respiratory issues, such as hypoxia and hypercapnia, are also common.
What is the role of ventilation management with breathing tubes?
Ventilation management involves adjusting ventilator settings to meet the patient’s needs. It includes monitoring respiratory parameters and troubleshooting common issues for optimal ventilation.
What are the criteria for safe extubation?
Safe extubation requires the patient to breathe on their own, have adequate oxygenation, and have neuromuscular blockade reversed. There should be no significant respiratory or cardiac complications.
Does general anesthesia require intubation?
Not all general anesthesia needs intubation. But it’s often used to ensure a secure airway and facilitate ventilation during surgery.
What is airway management anesthesia?
Airway management anesthesia involves techniques and strategies for managing the patient’s airway during general anesthesia. This includes intubation, ventilation, and airway protection.
What is a breathing tube for general anesthesia?
A breathing tube for general anesthesia is an endotracheal tube inserted into the patient’s airway. It facilitates ventilation and maintains a secure airway during surgery.
References
- Garruti, G., et al. (2018). Cholecystectomy: a way forward and back to metabolic disease? Current Opinion in Lipidology, 29(3), 189-195. Retrieved from