Last Updated on November 27, 2025 by Bilal Hasdemir

It’s important to know the difference between an angina episode and a heart attack. At Liv Hospital, we focus on your health and quality care. We believe knowing these differences helps you act quickly.
Angina pectoris is chest discomfort from less blood to the heart muscle. It usually happens when you’re stressed or active. It gets better with rest or medicine. On the other hand, a heart attack (myocardial infarction) means no blood flow to the heart. This causes lasting damage and needs fast medical help.
It’s key to tell these two apart. This ensures you get the right care and the best results.
Key Takeaways
- Angina and heart attacks are linked to coronary artery disease but have different care needs.
- Knowing the difference between angina and heart attacks is key for quick and right medical help.
- Angina is temporary chest pain from less blood flow, which gets better with rest or medicine.
- A heart attack is from no blood flow, causing lasting heart damage.
- Understanding these differences is vital for your health and well-being.
Understanding Coronary Artery Disease: The Common Denominator

Coronary artery disease (CAD) is the main cause of both angina and heart attacks. It’s key to understanding these heart issues. CAD damages the coronary arteries, which are vital for blood flow to the heart.
What is Coronary Artery Disease?
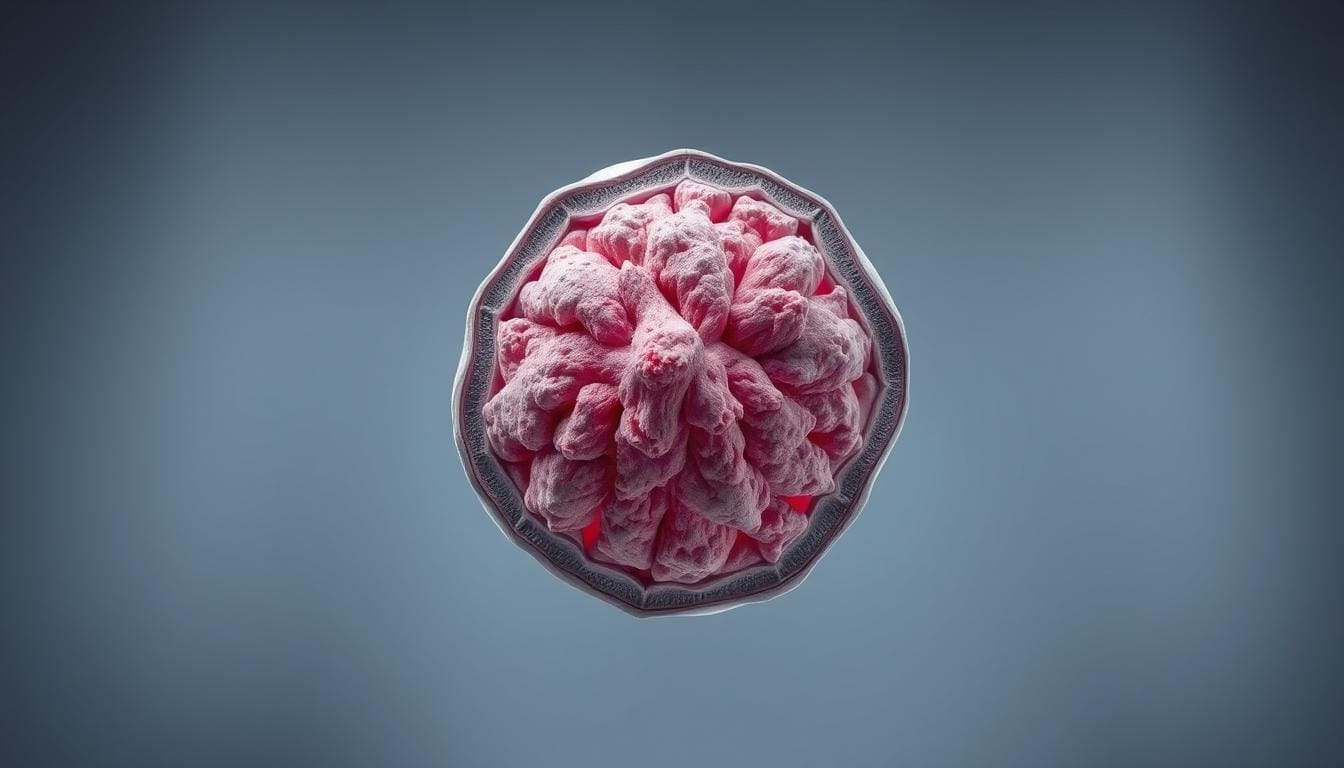
CAD is when plaque builds up in the coronary arteries. This plaque is made of fat, cholesterol, and other stuff. It can narrow or block the arteries, cutting off blood to the heart.
As we get older, the chance of getting CAD goes up. It’s also more common in families with heart disease history. High blood pressure, high cholesterol, and smoking are big risks for CAD.
How CAD Leads to Both Conditions
CAD can cause angina and heart attacks by reducing blood flow to the heart. When arteries narrow, the heart doesn’t get enough oxygen, leading to chest pain or discomfort.
Severe plaque buildup can cause a blood clot. This clot can block the artery, leading to a heart attack. The heart muscle gets damaged because it’s not getting enough blood.
Prevalence and Risk Factors
CAD is a big problem worldwide, leading to many deaths and illnesses. The World Health Organization (WHO) says cardiovascular diseases, including CAD, cause over 17.9 million deaths each year.
| Risk Factor | Description |
|---|---|
| High Blood Pressure | Increases the strain on coronary arteries, accelerating plaque buildup. |
| High Cholesterol | Elevated levels of LDL cholesterol contribute to plaque formation. |
| Smoking | Damages the inner lining of blood vessels, making them more susceptible to blockage. |
“The management of coronary artery disease requires a broad approach. This includes lifestyle changes, medical treatments, and sometimes surgery. Understanding risks and taking action can help prevent CAD and its complications.”
We need to tackle CAD with a wide-ranging plan. This includes prevention, early detection, and treatment. By doing this, we can lower the risk of angina and heart attacks, improving heart health.
What is an Angina Attack?
Angina attacks cause chest pain or discomfort due to less blood flow to the heart. This is a sign of coronary artery disease (CAD). CAD happens when the heart’s arteries narrow or block, leading to less oxygen for the heart.
Definition and Mechanism
Angina feels like pressure or squeezing in the chest. It can spread to the arms, back, neck, jaw, or stomach. It happens when the heart doesn’t get enough blood and oxygen, often during exercise or stress.
The heart’s arteries narrow, causing less oxygen-rich blood. This leads to ischemia and chest pain. Rest or medication can help by improving blood flow.
Types of Angina: Stable, Unstable, and Variant
There are different types of angina, each with its own signs and treatment needs.
- Stable Angina: This is the most common type. It follows a predictable pattern and is often triggered by physical exertion or emotional stress. Symptoms are usually relieved by rest or medication.
- Unstable Angina: Unstable angina is more unpredictable and can occur at rest. It is considered a medical emergency because it may signal an impending heart attack.
- Variant Angina: Also known as Prinzmetal’s angina, this type is caused by a spasm in the coronary arteries, leading to a temporary reduction in blood flow.
| Type of Angina | Characteristics | Triggers |
|---|---|---|
| Stable Angina | Predictable pattern, relieved by rest or medication | Physical exertion, emotional stress |
| Unstable Angina | Unpredictable, may occur at rest | Often occurs without a clear trigger |
| Variant Angina | Caused by coronary artery spasm | Often occurs at rest, sometimes related to smoking or stress |
Common Triggers for Angina
Knowing what triggers angina is key to managing it. Common triggers include:
- Physical exertion
- Emotional stress
- Extreme temperatures
- Heavy meals
- Smoking
By managing these triggers, people with angina can lessen their symptoms.
What is a Heart Attack (Myocardial Infarction)?
A heart attack, also known as myocardial infarction, is a serious condition. It happens when blood flow to the heart is blocked. This damage to the heart muscle can lead to serious health issues or even death if not treated quickly.
The term “heart attack” is often confused with “cardiac arrest.” But they are not the same. A heart attack is when blood flow to the heart stops. Cardiac arrest is when the heart suddenly stops working. We will explore what a heart attack is, its types, and risk factors in this section.
Definition and Mechanism
A heart attack happens when the coronary arteries, which supply blood to the heart, get blocked. This blockage is usually a blood clot on atherosclerosis (plaque) in the artery. The blockage stops blood flow to the heart, damaging or killing the heart muscle due to lack of oxygen and nutrients.
The process of a heart attack involves the rupture of atherosclerotic plaque, causing a blood clot. This clot blocks the artery, leading to reduced blood flow or death of heart muscle tissue.
Types of Heart Attacks: STEMI and NSTEMI
Heart attacks are divided into two types based on ECG findings: ST-Elevation Myocardial Infarction (STEMI) and Non-ST-Elevation Myocardial Infarction (NSTEMI).
- STEMI: This heart attack type has a complete blockage of a coronary artery, causing significant heart muscle damage. It is identified by an ST-segment elevation on an ECG.
- NSTEMI: NSTEMI happens with a partial blockage of a coronary artery. The damage to the heart muscle is less than STEMI, and the ECG may show ST-segment depression or T-wave inversion.
Risk Factors for Heart Attacks
Several factors increase the risk of having a heart attack. These include:
- High blood pressure
- High cholesterol levels
- Smoking
- Diabetes
- Obesity
- Family history of heart disease
- Age (risk increases after 45 for men and 55 for women)
Knowing these risk factors is key for prevention and management. By managing these factors, individuals can lower their risk of a heart attack.
Angina Attack vs Heart Attack: Understanding the Fundamental Differences
Knowing the difference between angina and heart attacks can save lives. Both are linked to coronary artery disease but have different impacts on treatment and outcomes.
Overview of the 4 Key Differences
We will look at four key differences between angina and heart attacks. These are important for doctors and patients to know. They cover the causes, symptoms, how they respond to treatment, and the long-term effects.
- Pathophysiology: Angina is caused by temporary blockages, while heart attacks result from long-lasting blockages.
- Symptom Duration and Intensity: Angina symptoms come on with effort and go away with rest. Heart attack symptoms are more severe and last longer.
- Response to Rest and Medication: Angina often gets better with rest and medication. Heart attack symptoms don’t improve with these treatments.
- Long-term Damage: Angina shows there’s disease in the arteries. A heart attack causes permanent damage to the heart.
Why Distinguishing Between Them Matters
It’s vital to tell angina and heart attacks apart because their treatments and outcomes are different. Getting it wrong can lead to bad results.
The wrong diagnosis can be very harmful. It can lead to more sickness and even death. So, knowing the differences is very important for patient care.
Statistics on Misdiagnosis and Consequences
Research shows that misdiagnosis of heart conditions is common and can be very harmful. Here are some stats on what happens when it happens.
| Condition | Misdiagnosis Rate | Consequences of Misdiagnosis |
|---|---|---|
| Angina | 20-30% | Inappropriate management, delayed treatment |
| Heart Attack | 2-5% | Increased mortality, complications |
Key Difference #1: Underlying Pathophysiology
The first key difference between angina and heart attacks is in their pathophysiology. Knowing this helps us see why they are different, even though they are related.
Temporary Ischemia vs. Permanent Damage
Angina is caused by temporary ischemia. This means the heart muscle doesn’t get enough oxygen-rich blood. It usually happens when the heart needs more oxygen, like during exercise or stress.
A heart attack, on the other hand, is caused by a blockage. This blockage leads to long-term ischemia, causing permanent damage to the heart muscle.
Reversible vs. Irreversible Cellular Changes
Angina leads to changes in cells that can be reversed. When oxygen demand goes down or with the right treatment, blood flow to the heart muscle can be restored. This reverses the ischemic condition.
A heart attack, though, causes permanent damage. The lack of blood flow for too long leads to the death of heart muscle cells.
What Happens at the Tissue Level
Angina causes temporary changes without scarring. But a heart attack leads to the death of heart muscle cells. This results in scarring and can harm the heart’s structure and function for a long time.
| Characteristics | Angina | Heart Attack |
|---|---|---|
| Ischemia Duration | Temporary | Prolonged |
| Cellular Changes | Reversible | Irreversible |
| Tissue Damage | No permanent scarring | Permanent scarring |
It’s key to understand these differences for diagnosis and treatment. Angina and heart attacks need different management and care because of their unique pathophysiology.
Key Difference #2: Symptom Duration and Intensity
It’s important to know the difference in symptom duration and intensity between angina attacks and heart attacks. Both can cause chest pain, but the pain’s nature, how long it lasts, and how intense it is can be very different.
Typical Angina Symptoms and Patterns
Angina symptoms usually follow a pattern. They happen during physical activity or stress and go away with rest or medicine. The pain feels like a squeeze in the chest and can spread to the arms, back, neck, jaw, or stomach.
Common characteristics of angina symptoms include:
- Triggered by exertion or stress
- Lasts between 5 to 15 minutes
- Relieved by rest or nitroglycerin
- Often feels like pressure or squeezing in the chest
Typical Heart Attack Symptoms and Patterns
Heart attack symptoms are often more severe and last longer. They can happen at any time, even when you’re not active, and don’t get better with rest or medicine. The pain is usually very intense and feels like a burning or crushing sensation.
Common characteristics of heart attack symptoms include:
- Can occur at rest
- Lasts more than 15 minutes
- Not relieved by rest or nitroglycerin
- Often feels like intense pressure or crushing in the chest
| Symptom Characteristics | Angina | Heart Attack |
|---|---|---|
| Duration | 5-15 minutes | More than 15 minutes |
| Triggered by | Exertion or stress | Can occur at rest |
| Relieved by | Rest or nitroglycerin | Not relieved by rest or nitroglycerin |
Atypical Presentations in Different Populations
Some groups might not show the usual symptoms. Women, diabetics, and older adults might not have chest pain. They might feel short of breath, tired, or have pain in the back or jaw instead.
How to Distinguish Based on Symptoms
To tell angina from heart attacks by symptoms, look at the pain’s length, how bad it is, and what makes it better or worse. If the symptoms don’t go away or are very bad, get help right away.
Key Difference #3: Response to Rest and Medication
Knowing how angina and heart attacks react to rest and medicine is key. This knowledge helps doctors diagnose and treat them correctly. Chest pain can tell us a lot about what’s happening in the heart.
How Angina Typically Responds to Interventions
Angina pain usually goes away with rest or nitroglycerin. This is because angina is caused by the heart needing more oxygen or having less blood flow. Resting or taking nitroglycerin helps by:
- Lowering the heart’s oxygen needs
- Making blood vessels wider for better heart flow
Nitroglycerin is a vasodilator that widens blood vessels. This improves blood flow and reduces heart work. If symptoms get better with rest or nitroglycerin, it’s likely angina.
Why Heart Attack Symptoms Persist Despite Rest
Heart attack symptoms don’t go away with rest or nitroglycerin. A heart attack happens when a blockage cuts off blood to the heart for too long. This damages or kills heart muscle. The blockage doesn’t clear with rest, so symptoms keep coming until medical help works.
The Nitroglycerin Response Test
The nitroglycerin test can help doctors figure out what’s wrong. If nitroglycerin makes chest pain better, it’s probably angina. But if pain doesn’t go away, it might be a heart attack or something serious. Not all heart attacks respond to nitroglycerin, so not getting relief means you need to act fast.
It’s important for both patients and doctors to understand these differences. If you have chest pain, it’s best to get medical help right away.
Key Difference #4: Long-term Damage and Prognosis
It’s important to know how angina and heart attacks affect the heart long-term. Both are linked to coronary artery disease. But, they impact heart health and future outlook differently.
Angina’s Impact on Heart Health
Angina itself doesn’t permanently harm the heart muscle. But, it signals coronary artery disease, which can worsen. Frequent angina episodes may mean a higher risk of heart attack. So, managing it and making lifestyle changes are key.
Heart Attack’s Lasting Effects on Cardiac Function
A heart attack causes permanent damage to the heart muscle. The damage’s extent depends on the attack’s length and the heart area affected. It can lead to reduced heart function and even heart failure over time.
Recovery Expectations for Both Conditions
Recovery plans vary for angina and heart attack patients. For angina, managing symptoms and lowering risk factors can greatly improve life quality. For heart attack survivors, recovery means managing heart disease and rehabilitating the heart muscle.
Quality of Life Considerations
Life quality after angina or a heart attack depends on treatment success, lifestyle changes, and heart disease management. Heart attack patients often need big lifestyle changes to prevent more heart problems and improve their future outlook.
Understanding these differences helps patients and doctors manage heart disease better. This leads to better outcomes and a better quality of life.
Prevention and Risk Reduction Strategies
To lower the risk of angina and heart attacks, it’s important to know and use effective prevention strategies. By taking a complete approach, people can greatly reduce their risk of getting these conditions.
Lifestyle Modifications for Both Conditions
Making lifestyle changes is key to preventing angina and heart attacks. Here are some recommendations:
- Dietary Changes: Eat a diet full of fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: Do at least 150 minutes of moderate exercise, or 75 minutes of vigorous exercise, or a mix of both, each week.
- Smoking Cessation: Quit smoking and avoid secondhand smoke.
- Stress Management: Use stress-reducing activities like meditation, yoga, or deep breathing exercises.
Medical Management of Risk Factors
Effective medical management is key to reducing the risk of angina and heart attacks. This includes:
- Managing Hypertension: Control high blood pressure with medication, lifestyle changes, or both.
- Cholesterol Management: Lower LDL cholesterol and raise HDL cholesterol through diet, exercise, and medication if needed.
- Diabetes Management: Keep blood sugar levels in a target range to avoid diabetes complications.
Monitoring and Follow-up Recommendations
Regular monitoring and follow-up are vital for those at risk of angina and heart attacks. We suggest:
- Regular Check-ups: Have regular appointments with your healthcare provider to check risk factors and adjust treatment plans as needed.
- Risk Factor Assessment: Regularly check risk factors like blood pressure, cholesterol levels, and blood glucose.
Emerging Preventive Approaches
New preventive approaches for angina and heart attacks are being researched. Some new strategies include:
- Genetic Screening: Find genetic predispositions to cardiovascular disease.
- Advanced Lipid Testing: Use advanced lipid profiles to better understand an individual’s risk.
- Personalized Medicine: Tailor prevention and treatment strategies to an individual’s unique genetic and environmental factors.
Conclusion: When to Seek Emergency Help
It’s important to know the difference between an angina attack and a heart attack. This knowledge can save lives. We’ve highlighted four main differences to help you understand the difference.
Knowing the signs of a heart attack is key. If you have severe chest pain, trouble breathing, or pain in your arm or jaw, get help right away.
Angina and heart attacks differ in how long and how bad the symptoms are. Angina is usually temporary chest pain that goes away with rest. A heart attack, on the other hand, has more severe and lasting symptoms.
If you’re not sure what’s happening, it’s better to be safe than sorry. Always seek medical help if you’re unsure. Knowing the difference between angina and a heart attack can be life-saving.
We urge you to take care of your heart. If you’re feeling symptoms or have concerns, talk to a doctor. They can guide you on when to get emergency help.
FAQ
What is the main difference between angina and a heart attack?
Angina is a sign of heart disease that causes temporary pain. A heart attack, on the other hand, causes lasting damage.
How do I know if I’m having an angina attack or a heart attack?
Angina pain goes away with rest or medicine. Heart attack pain doesn’t. If unsure, call for help right away.
What are the typical symptoms of angina and heart attacks?
Angina feels like chest pain that gets better with rest. Heart attacks have worse pain that lasts longer. They might also cause shortness of breath or nausea.
Can angina lead to a heart attack?
Yes, angina warns of heart disease. If not treated, it can lead to a heart attack.
How can I reduce my risk of both angina and heart attacks?
Eating well, exercising, quitting smoking, and managing stress can lower your risk.
What is the role of nitroglycerin in managing angina?
Nitroglycerin helps by opening blood vessels. This improves blood flow to the heart.
What are the long-term implications of having angina or experiencing a heart attack?
Both can harm your heart health. Heart attacks can cause more serious damage.
How do STEMI and NSTEMI heart attacks differ?
STEMI heart attacks block a coronary artery completely. NSTEMI heart attacks block it partially.
Can I have a heart attack without knowing it?
Yes, some heart attacks have no symptoms. This is more common in diabetics or older adults.
What should I do if I think I’m having a heart attack?
Call emergency services right away if you think you’re having a heart attack. Quick action is key.
How does coronary artery disease lead to both angina and heart attacks?
Coronary artery disease narrows or blocks arteries. This reduces blood flow to the heart, causing both angina and heart attacks.
What are the differences between stable, unstable, and variant angina?
Stable angina follows a pattern. Unstable angina is unpredictable and may signal a heart attack risk. Variant angina happens at rest due to artery spasm.
References
The Cardiology Advisor. Angina vs. Heart Attack: Comparing Presentations and Treatments. https://www.thecardiologyadvisor.com/features/angina-vs-heart-attack
Healthline. Angina vs. Heart Attack: How to Tell the Difference and Next Steps. https://www.healthline.com/health/heart/angina-vs-heart-attack
Heart Foundation New Zealand. Angina. https://www.heartfoundation.org.nz/your-heart/heart-conditions/angina