Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndrome, or MDS, is a condition where the bone marrow can’t make healthy blood cells. It’s also called myelodysplasia and preleukemia.
This condition affects how blood cells are made, leading to health problems. Knowing about MDS and its other names is important for both patients and doctors.
Myelodysplastic syndrome (MDS) is a complex disorder that affects the production of blood cells in the bone marrow. It’s important to understand the basics of MDS to grasp its implications on health.
MDS is a group of disorders caused by poorly formed or dysfunctional blood cells. This condition is characterized by the bone marrow’s failure to produce healthy, mature blood cells. As a result, patients with MDS often suffer from anemia, infections, and bleeding disorders due to the lack of functional blood cells.
The bone marrow’s inability to produce healthy blood cells is a hallmark of MDS. This disorder can progress to more severe conditions, such as acute myeloid leukemia (AML).
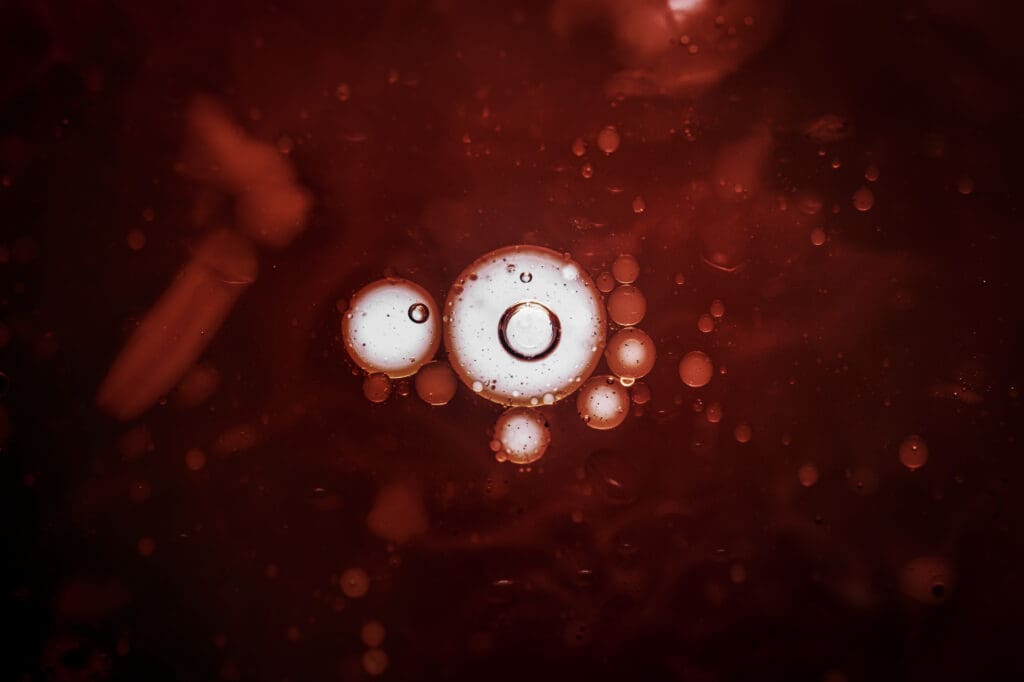
Blood cell production, or hematopoiesis, occurs in the bone marrow. It involves the development of blood cells from stem cells into mature cells, including red blood cells, white blood cells, and platelets. In MDS, this process is disrupted, leading to the production of abnormal blood cells.
Myelodysplastic syndrome (MDS) is known by many names. These names show its complex nature and different characteristics. Knowing these names helps us understand the condition’s many sides and its history.
Myelodysplasia is another name for MDS. It points out the changes in bone marrow cells. This term is often used with MDS, showing how the disorder affects blood cell production.
Myelodysplasia leads to low blood counts and can turn into a more serious disease like acute myeloid leukemia (AML).
The term preleukemia or pre-leukemia was used for MDS because it can turn into AML. It means MDS is a step before leukemia, showing a risk of becoming more aggressive. But not all MDS turns into leukemia, making this term a bit confusing.
Smoldering leukemia is a historical term once used for MDS when blast cells were few. It suggests a slow or hidden phase of leukemia. This shows MDS can stay mild for a while before becoming more serious.
Oligoblastic leukemia is for MDS with a small number of blast cells in the bone marrow. It’s used for MDS that’s not severe enough to be called AML but is at risk of getting worse. It highlights the range of MDS and its varying risks.
It’s key to know the abbreviations for Myelodysplastic Syndrome (MDS) for good patient care. Doctors use these abbreviations to talk about a patient’s health, treatment, and how they’re doing.
The term “MDS” is the top choice for Myelodysplastic Syndrome in medical writing and talks. It’s used in many fields like hematology and oncology. It helps doctors talk about the group of problems with making blood cells.
There are other abbreviations linked to MDS, seen in notes and studies. For example, “RA” for Refractory Anemia or “RARS” for Refractory Anemia with Ring Sideroblasts. Knowing these helps doctors understand patient information better and talk clearly.
The way we talk about myelodysplastic syndrome (MDS) has changed a lot. As doctors have learned more, the names for this condition have shifted. In the past, MDS was called many things, showing how complex and misunderstood it was.
Changes in MDS names came from better understanding of blood diseases. At first, MDS was mixed up with other bone marrow issues. But as research grew, so did the clarity in naming MDS. The World Health Organization (WHO) helped standardize these names, making it easier to diagnose and treat.
These updates show a deeper grasp of MDS and its ties to other blood cancers. Now, doctors can plan treatments more accurately, thanks to clearer names.
Old names like “preleukemia” and “smoldering leukemia” are no longer used. Today, we have more precise terms. “Myelodysplasia” is sometimes used, but MDS is more common. Knowing these old terms helps us understand older medical studies and the history of MDS research.
These changes came from new research and better diagnostic tools. Today’s names better describe MDS and its possible future.
It’s important to know the different types of myelodysplastic syndrome (MDS) for diagnosis and treatment. MDS is a group of disorders where blood cells are poorly formed or don’t work right. Over time, several systems have been used to classify MDS into its various types.
The World Health Organization (WHO) classification system is widely used for MDS. It sorts MDS based on how many blood cell lines are affected, the presence of ring sideroblasts, and the number of blasts in the bone marrow and blood. The WHO system identifies several subtypes, including MDS with single lineage dysplasia, MDS with multilineage dysplasia, and MDS with excess blasts.
The French-American-British (FAB) classification system is another old system for MDS. Even though the WHO system is now more common, the FAB system is important for understanding MDS history. The FAB system groups MDS into subtypes based on the number of blasts in the bone marrow and blood, including refractory anemia (RA), refractory anemia with ring sideroblasts (RARS), refractory anemia with excess blasts (RAEB), and chronic myelomonocytic leukemia (CMML).
| Classification System | Subtypes | Key Characteristics |
| WHO | MDS with single lineage dysplasia, MDS with multilineage dysplasia, MDS with excess blasts | Number of dysplastic lineages, presence of ring sideroblasts, percentage of blasts |
| FAB | RA, RARS, RAEB, CMML | Percentage of blasts in bone marrow and peripheral blood |
It’s important to know the differences between Myelodysplastic Syndrome (MDS) and other blood conditions. MDS shares some symptoms and bone marrow traits with other disorders.
MDS and leukemia are both blood disorders, but they differ in how they progress and what they are. Leukemia is a cancer of the blood or bone marrow that causes too many white blood cells. MDS, on the other hand, means the bone marrow doesn’t make enough blood cells.
While MDS can turn into leukemia, not everyone with MDS will get it. This shows that MDS and leukemia are not the same.
Aplastic anemia happens when the bone marrow can’t make blood cells. The main difference between MDS and aplastic anemia is the bone marrow’s look and cell count. MDS has a full bone marrow with abnormal cells, but aplastic anemia has a thin bone marrow.
Knowing this helps doctors choose the right treatment for each patient.
Myeloproliferative neoplasms (MPNs) are diseases where the body makes too many blood cells. MDS and MPNs can sometimes look similar, making diagnosis tricky. Some patients might have both MDS and MPN features.
Doctors need to look closely at the bone marrow and blood to make an accurate diagnosis.
MDS shows different signs, including physical symptoms and lab results. Each patient’s experience can vary. It’s key to know the possible symptoms.
People with MDS face many physical issues. These include fatigue, weakness, and shortness of breath. These problems come from not enough red blood cells.
Other symptoms are infections and bleeding easily. This is because of low platelet counts. It can cause easy bruising or nosebleeds.

Lab tests are vital for diagnosing MDS. They often show anemia, neutropenia, and thrombocytopenia. Blood tests can find abnormal cell morphology and blast cells.
These findings help doctors diagnose MDS and see how severe it is.
Knowing both physical symptoms and lab results is key. It helps doctors diagnose and manage MDS accurately.
Diagnosing myelodysplastic syndrome (MDS) requires several tests. These tests help find out if you have MDS and how severe it is. Knowing this is key to choosing the right treatment and understanding your future.
Doctors use a few important tests to diagnose MDS. These tests check the health of your blood cells and bone marrow.
A complete blood count (CBC) is often the first test for MDS. It looks at the numbers of red, white blood cells, and platelets. If these numbers are off, it might mean you have MDS.
Blood tests can show signs like anemia or low white blood cells, which are common in MDS. Looking closely at the blood smear can give more details about your blood cells.

A bone marrow biopsy and aspiration are key for diagnosing MDS. These tests take a bone marrow sample for study. The biopsy shows the marrow’s structure, and the aspiration looks at cell shape and genetics.
The bone marrow test can spot changes in cells that are typical of MDS. It also helps rule out other diseases that might look like MDS.
Genetic and molecular testing are very important for MDS diagnosis and treatment planning. These tests find specific genetic changes linked to MDS. This info helps doctors understand the risk and decide on treatment.
By using these tests, doctors can accurately diagnose MDS. Then, they can create a treatment plan that’s right for you.
Myelodysplastic Syndrome (MDS) has several key risk factors. Knowing these can help spot and manage the condition early.
Age is a big risk factor for MDS, with most cases found in people over 60. Older adults are more likely to get MDS because of genetic damage that builds up over time. Gender and ethnicity might also play a part, but the evidence is not as strong.
Being exposed to certain toxins, like benzene and pesticides, raises the risk of MDS. Working with harmful chemicals is also a risk factor.
Some people are born with genetic mutations that make them more likely to get MDS. Genetic counseling can help those with a family history of MDS or similar conditions.
Getting chemotherapy or radiation therapy before can raise the risk of MDS. This is true for treatments that use alkylating agents or topoisomerase inhibitors.
The International Prognostic Scoring System (IPSS) is key for predicting MDS patient outcomes. It helps doctors understand the risk of turning into acute myeloid leukemia (AML) and survival chances.
The IPSS sorts MDS patients into risk groups. It looks at bone marrow blasts, karyotype, and cytopenias. Each factor gets points, and the total score shows the risk level.
The risk levels are:
The Revised IPSS (IPSS-R) updates the original with new factors. It includes detailed cytogenetic analysis and refined blast percentage. This version offers a more precise prognosis.
The IPSS-R is more accurate than the original IPSS. It predicts survival and AML risk better. It’s now a main tool in treating MDS patients.
Treatment for myelodysplastic syndrome (MDS) involves many strategies. The right treatment depends on the MDS subtype, the patient’s health, and genetic mutations.
Supportive care is key in managing MDS. It aims to ease symptoms and improve life quality. This includes blood transfusions for anemia and infections, and antibiotics for infections.
Supportive care is essential for keeping patients healthy and functional.
Growth factors and cytokines help make more blood cells. Erythropoietin and granulocyte-colony stimulating factor (G-CSF) are examples. They help reduce blood transfusions and boost the immune system.
Hypomethylating agents, like azacitidine and decitabine, can improve blood counts. They may also slow MDS turning into acute myeloid leukemia (AML). These drugs change the DNA of cancer cells.
Immunomodulatory drugs, including lenalidomide, are effective for some MDS types. They help increase blood counts and lower transfusion needs. These drugs adjust how the immune system fights cancer cells.
Every patient with MDS needs a treatment plan that fits their unique situation. Knowing all the treatment options helps doctors create better plans for patients.
Living with myelodysplastic syndrome (MDS) means you need a full plan to handle its symptoms and boost your quality of life. MDS messes with your bone marrow, making it hard to produce healthy blood cells. This leads to many problems.
It’s key to manage MDS symptoms to keep your life good. Symptoms include feeling very tired, getting sick easily, and bleeding a lot because of low blood cell counts.
For MDS patients, it’s not just about symptoms. It’s also about how the disease affects your mind and feelings.
| Symptom/Challenge | Management Strategy | Benefits |
| Fatigue | Conserve energy, gentle exercises | Improved energy levels, reduced exhaustion |
| Infections | Good hygiene, vaccinations | Reduced risk of infections |
| Bleeding | Soft-bristled toothbrushes, avoid contact sports | Minimized bleeding risks |
MDS and AML are closely related diseases. MDS often leads to AML in some cases. Knowing this helps in managing MDS better.
MDS can turn into AML, a serious change in the disease. This change affects the disease’s severity and outlook. Certain genetic mutations and clinical features increase this risk.
Several factors raise the risk of MDS turning into AML. These include:
| Risk Factor | Description | Impact on AML Transformation |
| TP53 Mutations | Genetic mutations affecting the TP53 gene | Increased risk |
| Complex Karyotypic Abnormalities | Multiple chromosomal abnormalities | Higher risk of transformation |
| Higher Blast Counts | Elevated percentage of blasts in bone marrow | Increased risk of AML |
Understanding these risk factors is key. It helps doctors keep a close eye on MDS patients. They can then act quickly to prevent or delay AML transformation.
Research on Myelodysplastic Syndrome (MDS) has seen big steps forward. This includes new genetic discoveries and emerging treatments. These breakthroughs are changing how we see MDS and giving patients better treatment choices.
Studies have found several genetic mutations linked to MDS. This has helped us understand how MDS starts and grows. Important genes like SF3B1, TET2, and RUNX1 are key in MDS development.
Studying these mutations has given us a clearer picture of MDS. It shows the disease’s complexity and helps predict outcomes and treatments. Below is a table with some key genetic mutations and how common they are in MDS patients.
| Gene | Mutation Frequency | Clinical Significance |
| SF3B1 | 20-30% | Associated with better prognosis |
| TET2 | 20-25% | Influences response to hypomethylating agents |
| RUNX1 | 10-15% | Often associated with poorer prognosis |
New treatments for MDS are being developed. Hypomethylating agents and immunomodulatory drugs are showing promise. Clinical trials are also exploring new ways to treat MDS, like targeted therapies and combining different treatments.
Some of the new treatments being looked at include:
These advancements in MDS research are vital for better patient care. They bring hope for more effective treatments in the future.
The journey of MDS patients and their caregivers can be made easier with the right resources. Support organizations and educational content are key. They offer the support and information needed to manage MDS well.
Many organizations provide support to MDS patients and their families. Here are a few:
| Organization | Description | Services Offered |
| Aplastic Anemia & MDS International Foundation | A organization dedicated to providing support and resources for patients with aplastic anemia and MDS. | Patient support groups, educational materials, advocacy |
| Leukemia & Lymphoma Society | An organization focused on blood cancers, including MDS. | Financial assistance, patient education, support services |
Understanding MDS and its management is key. Educational materials and online resources help a lot. Here are some important ones:
Myelodysplastic syndrome (MDS) is a complex group of disorders. It happens when the bone marrow can’t make healthy blood cells. It’s important for patients, caregivers, and healthcare professionals to understand MDS well.
A summary of MDS shows it has different subtypes, risk factors, and treatments. The World Health Organization (WHO) and the International Prognostic Scoring System (IPSS) help diagnose and predict MDS outcomes.
New genetic discoveries and therapies bring hope to MDS patients. Support groups and educational resources help improve life quality for those affected.
In conclusion, knowing a lot about MDS is key to managing it well. By keeping up with the latest research and treatments, people can face MDS challenges better.
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure.
MDS is also known as myelodysplasia, preleukemia, smoldering leukemia, and oligoblastic leukemia.
The primary abbreviation for MDS is MDS. It stands for myelodysplastic syndrome.
MDS is diagnosed through blood tests, bone marrow biopsy, and genetic testing.
Common symptoms include fatigue, weakness, shortness of breath, and infections. These are due to low blood cell counts.
Risk factors include age, exposure to certain chemicals, radiation, and prior cancer treatments.
MDS is classified using the World Health Organization (WHO) and French-American-British (FAB) systems.
The IPSS predicts the prognosis of patients with MDS. It looks at bone marrow blast percentage and cytogenetics.
Treatment options include supportive care, growth factors, hypomethylating agents, and immunomodulatory drugs.
Yes, MDS can progress to AML, a more aggressive type of blood cancer.
MDS is a precursor to AML. Patients with MDS are at risk of transformation to AML.
Yes, there are support organizations, educational materials, and online resources for MDS patients and caregivers.
Recent advances include genetic discoveries and emerging therapies. There are also ongoing clinical trials.
MDS patients can manage symptoms and improve quality of life. This is through supportive care, symptom management, and lifestyle modifications.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!