Diagnosed with aortic valve stenosis? We get it. It’s scary and uncertain. At Liv Hospital, we’re here to offer top-notch care. We aim to help you manage this condition with confidence.
Aortic valve stenosis makes the aortic valve narrow. This blocks blood flow from the heart. Studies show transcatheter aortic valve implantation (TAVI) is a good option for severe cases.
We’ll walk you through the treatment options. We’ll talk about their benefits and risks. Our team is here to support you every step of the way.
Key Takeaways
- Understanding aortic valve stenosis and its impact on heart health
- Exploring the available treatment options, including TAVI and surgical aortic valve replacement
- Learning about the benefits and risks of each treatment
- Discovering how Liv Hospital’s expertise can support your care journey
- Gaining insights into what to expect from your chosen treatment path
Understanding Aortic Valve Stenosis
It’s important for patients to understand aortic valve stenosis. This helps them see how serious it is and why they need the right treatment. We’ll explain what the aortic valve is and how stenosis affects the heart.
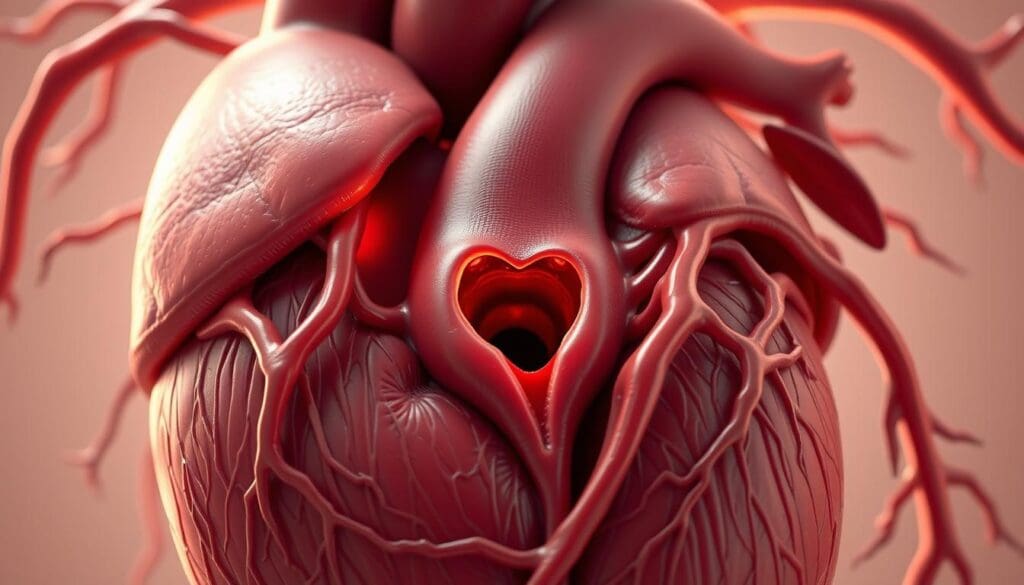
Definition and Anatomy
Aortic valve stenosis happens when the aortic valve opening gets smaller. This blocks blood flow from the left ventricle to the aorta. The aortic valve is key to the heart, with three cusps that control blood flow.
Most often, stenosis is caused by age-related thickening and calcification of the valve. But, congenital defects or rheumatic fever can also play a role. Knowing the cause helps doctors choose the best treatment.
How Stenosis Affects Heart Function
When the aortic valve narrows, it makes it hard for the heart to pump blood into the aorta. This raises pressure in the left ventricle. Symptoms can include chest pain, shortness of breath, and feeling tired.
In severe cases, stenosis can cause heart failure if not treated. It can also lead to hemoptysis, or coughing up blood, though this is rare.
| Impact on Heart Function | Description |
|---|---|
| Increased Pressure | The heart works harder to pump blood through the narrowed valve. |
| Reduced Blood Flow | Less blood is pumped into the aorta, potentially leading to inadequate blood supply to vital organs. |
| Potential Complications | Untreated severe stenosis can lead to heart failure and other serious complications. |
Causes and Risk Factors
It’s important to know the causes and risk factors of aortic valve stenosis. This knowledge helps in early detection and treatment. Aortic valve stenosis can come from different sources, and knowing these helps tailor treatments.
Age-Related Calcification
Calcification with age is a common cause of aortic valve stenosis. As we get older, calcium builds up on the aortic valve, narrowing it. This is similar to how atherosclerosis forms in arteries.
Early stages may show mild aortic valve stenosis with few symptoms. But, as it gets worse, it can cause serious heart problems.
Congenital Heart Defects
Congenital heart defects are a big risk for aortic valve stenosis. Some people are born with a bicuspid aortic valve, which has only two cusps. This can lead to valve problems over time.
Regular monitoring is key for those with congenital heart defects to spot issues early.
Rheumatic Fever and Other Causes
Rheumatic fever, caused by streptococcal infection, can also lead to aortic valve stenosis. Though rare in developed countries, it’s a big problem worldwide. Other causes include radiation to the chest and certain metabolic conditions.
Knowing these risk factors helps in early diagnosis and treatment of aortic valve stenosis.
In severe cases, heart transplantation might be needed. The choice between donation after brain death (DBD) and donation after circulatory death (DCD) affects graft success. This shows how critical it is to manage aortic valve stenosis well to avoid such extreme measures.
Recognizing the Symptoms
It’s important to know the symptoms of aortic valve stenosis to get help quickly. This condition might not show symptoms at first. But as it gets worse, you’ll start to notice them.
Early Warning Signs
In the beginning, aortic valve stenosis might not show obvious signs. But there are early warning signs to watch for:
- Fatigue or feeling weak
- Mild shortness of breath during routine activities
- Palpitations or irregular heartbeats
Knowing these signs is key. They can mean more serious problems are coming.
Advanced Symptoms
As aortic valve stenosis gets worse, symptoms get more serious. Advanced symptoms include:
- Chest pain (angina) or discomfort, often triggered by physical activity
- Severe shortness of breath (dyspnea) even at rest
- Fainting or dizziness (syncope)
- Swollen ankles and feet due to fluid buildup
These signs mean the condition has worsened. You need to see a doctor right away.
When to Seek Medical Attention
If you’re showing symptoms of aortic valve stenosis, get help fast. Severe heart stenosis is a major risk factor for congestive heart failure. The heart has trouble pumping blood because of the narrowed valve.
Recent studies show that
“Patients with severe aortic stenosis who are symptomatic have a poor prognosis without intervention, with a significant risk of mortality within the first year.”
So, it’s important to catch symptoms early and see a doctor.
Being overweight increases the risk of heart problems like heart failure and coronary artery disease. Eating right and exercising can help lower these risks.
| Symptom | Description | Action |
|---|---|---|
| Chest Pain | Discomfort or pain in the chest, often during physical activity | Seek immediate medical attention |
| Shortness of Breath | Difficulty breathing, even at rest | Consult a healthcare professional |
| Fainting or Dizziness | Feeling lightheaded or passing out | Seek immediate medical attention |
Diagnosis and Evaluation Process
To accurately diagnose aortic valve stenosis, we use several methods. These include physical exams, imaging tests, and sometimes cardiac catheterization. These tools help us understand how severe the condition is and plan the best treatment.
Physical Examination
A physical exam is the first step in diagnosing aortic valve stenosis. We listen to the heart with a stethoscope to find any unusual sounds. A specific murmur can suggest aortic stenosis, heard best at the right second intercostal space.
We also look for other signs like a weak pulse or low blood pressure. These signs help us decide what to do next in the diagnosis.
Imaging Tests
Imaging tests are key in confirming the diagnosis and understanding the severity of aortic valve stenosis. The main tests used are:
- Echocardiography: This test gives detailed images of the heart. It helps measure the valve area and assess the degree of stenosis.
- Electrocardiogram (ECG): An ECG can show signs of heart problems, even if it’s not diagnostic for aortic stenosis.
- Chest X-ray: This test can show heart enlargement or calcium deposits on the valve.
- Cardiac MRI or CT scan: These tests provide more detailed information on the valve anatomy, helping in planning treatments.
Cardiac Catheterization
Cardiac catheterization is an invasive test that directly measures heart pressures. It’s useful when non-invasive tests don’t match clinical findings.
During the test, we can measure the pressure gradient across the valve and check for coronary artery disease. This helps us plan the best treatment, whether surgery or other options.
By combining physical exams, imaging tests, and cardiac catheterization, we can accurately diagnose and evaluate aortic valve stenosis. This guides us to the most suitable treatment for each patient.
Stages of Aortic Valve Stenosis
Knowing the stages of aortic valve stenosis is key to picking the right treatment. This condition gets worse over time. It has different stages, each with its own signs and what it means for care.
Mild to Moderate Stenosis
In the early stages, people might not feel much pain. Mild to moderate stenosis means the valve opening gets smaller. This puts more strain on the heart.
It’s important to see a doctor regularly to watch the disease. They might suggest changes in lifestyle or medicine to help manage symptoms.
Severe Symptomatic Stenosis
When it gets to severe symptomatic stenosis, symptoms get worse. People might feel chest pain, have trouble breathing, or get tired easily. The risk of heart failure goes up a lot.
At this point, doctors often need to take action. They might suggest surgery or a new valve through a catheter, based on the patient’s health.
Impact on Heart Function
As aortic valve stenosis gets worse, it can hurt the heart’s function. The heart has to work harder, which can make it thicker and lead to heart failure.
| Stage | Characteristics | Symptoms | Typical Treatment Approach |
|---|---|---|---|
| Mild to Moderate | Gradual narrowing of the aortic valve | Often asymptomatic or mild symptoms | Monitoring, lifestyle modifications |
| Severe Symptomatic | Significant narrowing, high risk of complications | Chest pain, shortness of breath, fatigue | Surgical or transcatheter valve replacement |
Heart failure can lead to serious problems and even death. Knowing the stages helps doctors and patients choose the best treatment.
Comprehensive Aortic Valve Stenosis Treatment Options
There are many ways to treat aortic valve stenosis, aiming for the best results. The treatment depends on how severe the stenosis is, the patient’s health, and other factors.
Treatment Selection Criteria
Choosing the right treatment for aortic valve stenosis is important. It looks at symptoms, how narrow the valve is, other heart issues, and the patient’s health.
Key considerations in treatment selection include:
- Severity of aortic valve stenosis
- Presence of symptoms and their impact on quality of life
- Patient’s age and overall health status
- Presence of comorbid conditions
Risk Assessment
Assessing the risk is key to picking the best treatment. It looks at the patient’s risk for complications with each option.
Risk assessment considers factors such as:
- Cardiac function and overall heart health
- Presence of other medical conditions that may impact treatment
- Previous cardiac interventions or surgeries
The Heart Team Approach
Managing aortic valve stenosis now often involves a Heart Team. This team includes cardiologists, surgeons, and imaging experts. They work together to create a treatment plan that fits the patient’s needs.
The Heart Team approach has many benefits, including:
- Comprehensive evaluation of the patient’s condition
- Discussion of various treatment options and their outcomes
- Development of a personalized treatment plan
- Improved coordination of care throughout the treatment process
By using a Heart Team and looking at all treatment options, doctors can give patients the best care. This includes watchful waiting, medication, balloon valvuloplasty, Surgical Aortic Valve Replacement (SAVR), and Transcatheter Aortic Valve Implantation (TAVI/TAVR).
Option 1: Watchful Waiting and Monitoring
For those with mild or no symptoms of aortic valve stenosis, watchful waiting and monitoring is often advised. This means regular check-ups to track the condition’s progress, without immediate treatment.
Candidates for Conservative Management
Not every patient with aortic valve stenosis needs immediate treatment. Those who are asymptomatic or have mild symptoms might be good candidates for watchful waiting. We look at the stenosis’s severity, the patient’s overall health, and other heart conditions to decide.
Follow-up Protocol
Regular check-ups are key for patients on watchful waiting. This includes:
- Regular echocardiograms to check valve function
- Clinical assessments to watch for symptoms
- Lifestyle advice to keep the heart healthy
We customize the follow-up plan for each patient, adjusting as needed.
When to Consider Intervention
Watchful waiting is effective, but sometimes, intervention is needed. We look at symptom development, stenosis progression, and health changes to decide when to act. Research shows monitoring can manage asymptomatic severe aortic stenosis well, but timely action is key to avoid complications.
Option 2: Medication Management
Medication management is key for aortic valve stenosis, even if it’s not a cure. We use different drugs to help control symptoms and slow the disease’s progress. This helps patients with aortic valve stenosis feel better.
Types of Medications Used
There are several medications for aortic valve stenosis. These include:
- Diuretics: To reduce fluid buildup and alleviate symptoms of heart failure.
- ACE inhibitors: To manage high blood pressure and reduce the heart’s workload.
- Beta-blockers: To control heart rate and reduce the force of contraction.
- Anti-arrhythmic medications: To manage irregular heart rhythms.
These drugs help manage symptoms and improve life quality for patients.
Symptom Control Strategies
Controlling symptoms is vital for aortic valve stenosis management. Our approach includes:
- Monitoring and adjusting medications based on symptom severity.
- Lifestyle modifications, such as diet and exercise, to manage related conditions.
- Regular follow-up appointments to assess disease progression and adjust treatment plans.
By using these strategies, we can greatly improve patient outcomes.
Limitations of Medical Therapy
While medication management is helpful, it has its limits. It can’t fix or replace a damaged valve; it only manages symptoms. So, patients with severe aortic valve stenosis might need more serious treatments like surgery or a new valve.
In summary, medication management is a critical part of treating aortic valve stenosis. It offers symptom relief and improves life quality. Yet, it’s not a replacement for more definitive treatments when needed.
Option 3: Balloon Valvuloplasty
Balloon valvuloplasty is a treatment for aortic valve stenosis. It widens the narrowed valve. This option is for some patients who can’t have more serious treatments like surgery.
Procedure Details and Preparation
The procedure starts with a catheter with a balloon inserted into a blood vessel in the groin. It’s then guided to the aortic valve. The balloon is inflated to open the valve wider. This is done under general anesthesia or sedation to reduce pain. Before the procedure, patients get checked with tests and health assessments.
Recovery and Effectiveness
Patients are watched closely after the procedure for any issues. How well it works can vary; some see big improvements, others not so much. Recovery includes a short hospital stay and rest at home. Following a care plan is key for a smooth recovery.
Long-term Outcomes
While it helps with symptoms, balloon valvuloplasty’s long-term success is limited in adults. The valve might narrow again, needing more treatment. Yet, it’s a good choice for some, like those avoiding surgery or needing a temporary fix.
Every patient is different, and talking to a doctor is essential. Discussing the pros and cons helps patients make the best choice for their treatment.
Option 4: Surgical Aortic Valve Replacement (SAVR)
SAVR, or Surgical Aortic Valve Replacement, is a key treatment for aortic valve stenosis. It replaces the old valve with a new one, improving blood flow and easing symptoms.
Traditional vs. Minimally Invasive Approaches
SAVR can be done in two ways: open-heart surgery or minimally invasive methods. Traditional open-heart surgery uses a big chest incision for direct heart access. It’s effective but can lead to longer recovery times.
Minimally invasive SAVR uses smaller cuts, causing less damage, less pain, and faster healing. We choose the best method based on the patient’s health and condition.
Mechanical vs. Biological Valves
During SAVR, a new valve is put in place. Mechanical valves are strong and made of materials like titanium. They need lifelong blood thinner treatment to avoid clots.
Biological valves are made from animal tissue and work more like a natural valve. They usually don’t need blood thinners but might need to be replaced later. We help patients weigh the benefits and drawbacks of each type.
| Valve Type | Durability | Anticoagulation Therapy |
|---|---|---|
| Mechanical | High | Lifelong |
| Biological | Limited | Typically not required long-term |
Recovery Timeline and Rehabilitation
Recovery from SAVR depends on the surgery type and patient health. Patients usually stay in the hospital for a few days. Full recovery can take weeks to months.
We offer a detailed rehabilitation program. It includes physical therapy, diet advice, and follow-up visits to check on progress.
Potential Complications
SAVR, like any surgery, has risks such as bleeding, infection, stroke, and anesthesia reactions. We do everything we can to reduce these risks and watch patients closely before and after surgery.
Understanding SAVR, including its methods, valve choices, recovery, and risks, helps patients make informed choices. We aim to provide personalized care and support throughout the SAVR process.
Option 5: Transcatheter Aortic Valve Implantation (TAVI/TAVR)
TAVI/TAVR is a key treatment for aortic valve stenosis, mainly for those at high risk for surgery. It replaces the diseased valve with a new one through a catheter. This method avoids open-heart surgery.
Procedure Overview and Preparation
The TAVI/TAVR process starts with detailed tests to check the valve and nearby areas. Patients are then ready for the procedure, often under sedation or anesthesia. The catheter is inserted through a small incision, usually in the groin or chest, and guided to the heart.
A leading cardiologist says, “TAVI/TAVR is a big change in treating aortic valve stenosis. It’s a good option for those too risky for surgery.”
“The future of aortic valve replacement is here, and it’s less invasive, safer, and highly effective.”
Ideal Candidates for TAVI
Those with severe aortic valve stenosis and high or intermediate risk for surgery are best for TAVI/TAVR. This includes patients with many health issues or are older. A team of doctors decides the best treatment for each patient.
Recovery and Post-Procedure Care
Recovery from TAVI/TAVR is quicker than traditional surgery, with most going home in a few days. After, they watch for complications, manage symptoms, and have follow-ups. They also learn about lifestyle changes to keep their heart healthy.
Recent Advancements and Success Rates
New studies show TAVI/TAVR is safe and effective, even for lower-risk patients. Better technology has improved valve designs and delivery systems. This makes TAVI/TAVR a top choice for many.
As we keep improving TAVI/TAVR, we’re seeing more uses and better results for aortic valve stenosis patients. This shows the value of a team approach to care, making sure patients get the best treatment.
Conclusion: Living With Aortic Valve Stenosis
Managing aortic valve stenosis well means making lifestyle changes and sticking to treatment plans. It’s key to have a team of doctors working together to create a plan just for you.
Dealing with aortic valve stenosis means keeping an eye on your health and possibly trying different treatments. These can include medicines, balloon procedures, or even surgery. For more on how 4D flow CMR helps, check out this resource.
With the right mix of medical care, lifestyle changes, and regular check-ups, we can help patients with aortic valve stenosis live better. Managing this condition is a long-term effort. It needs careful planning and teaching patients to live well with it.
What is aortic valve stenosis?
Aortic valve stenosis is a serious heart condition. It happens when the aortic valve gets narrower, blocking blood flow. This can cause symptoms like chest pain, shortness of breath, and feeling very tired.
What are the causes and risk factors of aortic valve stenosis?
Causes include age-related calcification, congenital heart defects, and rheumatic fever. Risk factors include being older, having a history of heart conditions, and certain genetic predispositions.
What are the symptoms of aortic valve stenosis?
Symptoms range from mild shortness of breath to severe chest pain, dizziness, and fainting. It’s important to recognize these symptoms early for timely medical help.
How is aortic valve stenosis diagnosed?
Diagnosis involves physical exams, imaging tests like echocardiography, and cardiac catheterization. Accurate diagnosis is key to choosing the right treatment.
What are the treatment options for aortic valve stenosis?
Treatments include watchful waiting, medication, balloon valvuloplasty, surgical aortic valve replacement (SAVR), and transcatheter aortic valve implantation (TAVI/TAVR). The choice depends on the condition’s severity, overall health, and other factors.
What is the difference between SAVR and TAVI/TAVR?
SAVR is traditional open-heart surgery to replace the aortic valve. TAVI/TAVR is a minimally invasive procedure to implant a new valve through a catheter, avoiding open-heart surgery.
What is balloon valvuloplasty?
Balloon valvuloplasty uses a balloon to widen the narrowed aortic valve. It’s used in specific cases, like in younger patients or as a bridge to more definitive treatments.
Can aortic valve stenosis be managed with medication?
Medication can’t cure aortic valve stenosis but can manage symptoms and slow disease progression. It helps control symptoms like high blood pressure and heart failure.
What is the role of a heart team in treating aortic valve stenosis?
A heart team, including cardiologists and surgeons, assesses the condition and decides the best treatment plan for each patient.
What are the benefits of TAVI/TAVR compared to SAVR?
TAVI/TAVR is minimally invasive, has a shorter recovery time, and fewer complications. It’s a good option for those at high risk for open-heart surgery.
How can I prepare for aortic valve stenosis treatment?
Preparation involves understanding your diagnosis, discussing treatment options, and following pre-procedure instructions. Having a support system is also important for recovery.
References
American Heart Association (AHA): Managing Aortic Stenosis Symptoms
AHA Journals (Circulation Research): Aortic Valve Disease Research (Specific DOI)


































