People with sickle cell disease face a risk of aplastic crisis. This is when the bone marrow stops making red blood cells. It causes a sudden drop in red blood cells, making anemia worse.
At Liv Hospital, we know how to tell apart an aplastic crisis from aplastic anemia. Sickle cell disease is a group of disorders. They happen when a sickle mutation and another harmful variant are inherited together. This reduces normal beta-globin production.
It’s key for families and doctors to understand these conditions. This helps manage the disease better.
Key Takeaways
- Aplastic crisis is a condition where bone marrow temporarily stops producing red blood cells.
- It leads to a sudden and severe worsening of anemia in patients with sickle cell disease.
- Distinguishing between aplastic crisis and aplastic anemia is key to effective management.
- Sickle cell disease is a group of disorders characterized by the inheritance of the sickle mutation and another pathogenic variant.
- Understanding these conditions is vital for families and healthcare providers.
Understanding Aplastic Crisis

Aplastic crisis is a serious condition that affects people with certain blood disorders, like sickle cell disease. It causes a sudden drop in red blood cell production, leading to severe anemia.
Definition and Basic Mechanism
Aplastic crisis is when the bone marrow suddenly stops making red blood cells. It’s often caused by infections like parvovirus B19. This condition is a big problem for people with chronic blood diseases.
The virus attacks the cells that make red blood cells, stopping their production. This leads to a quick drop in hemoglobin levels. If not treated quickly, it can be deadly.
Importance of Hematological Disorders
Aplastic crisis is very important for managing blood disorders, like sickle cell disease. Knowing about it helps doctors diagnose and treat it early. This can greatly improve patient outcomes.
The table below summarizes key aspects of aplastic crisis in the context of hematological disorders:
| Aspect | Description | Clinical Implication |
| Definition | Transient failure of red blood cell production | Severe anemia |
| Common Trigger | Parvovirus B19 infection | Temporary halt in erythropoiesis |
| Impact on Sickle Cell Disease | Rapid decline in hemoglobin levels | Life-threatening if untreated |
It’s important for healthcare providers to know the signs of aplastic crisis and how it works. This helps them give the right care. By doing this, we can better manage patients with blood disorders and lower the risk of complications from aplastic crisis.
Sickle Cell Disease: A Brief Overview

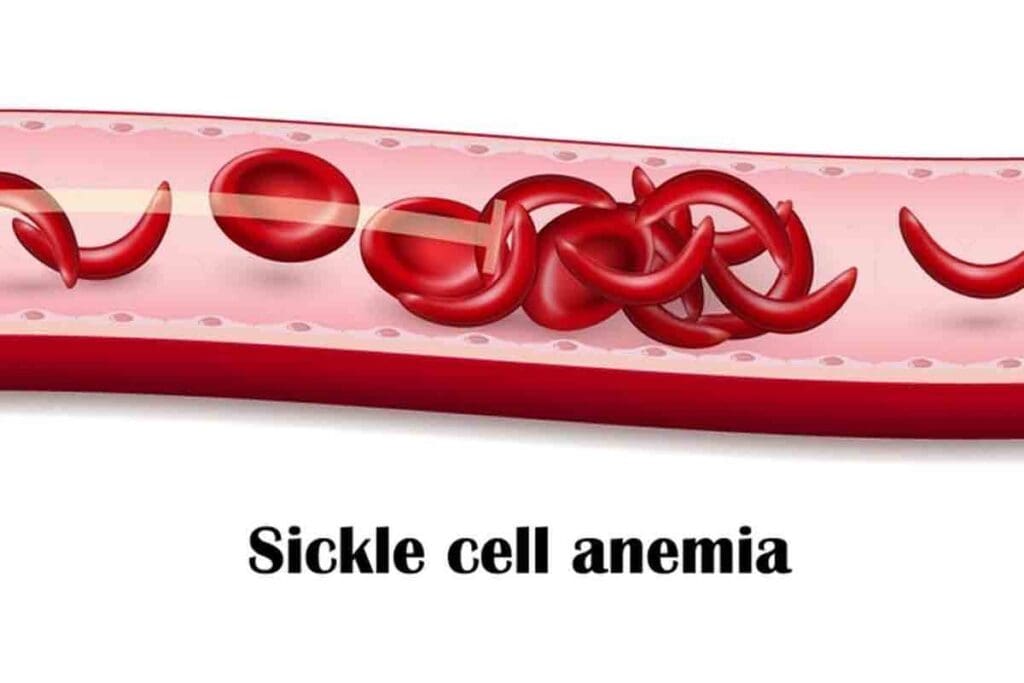
To understand sickle cell disease, we need to look at its pathophysiology and the health challenges it brings. Sickle cell disease (SCD) is a genetic disorder that affects how hemoglobin is made. Hemoglobin is a protein in red blood cells that carries oxygen.
Pathophysiology of Sickle Cell Disease
The disease comes from a mutation in the HBB gene. This mutation changes the beta-globin subunit of hemoglobin into sickle hemoglobin (HbS). When HbS loses oxygen, it forms polymers, causing red blood cells to bend into a sickle shape.
This bending leads to hemolytic anemia and vaso-occlusion. These issues cause pain, tissue damage, and can harm organs.
The sickling of red blood cells is influenced by several factors. These include other hemoglobin variants, fetal hemoglobin levels, and red blood cell dehydration.
Baseline Hematological Challenges
People with SCD face many hematological challenges. These include chronic hemolytic anemia, which can cause jaundice and an enlarged spleen. The disease also increases the risk of vaso-occlusive crises, acute chest syndrome, and other serious issues.
| Hematological Challenge | Description | Clinical Impact |
| Chronic Hemolytic Anemia | Persistent breakdown of red blood cells | Jaundice, fatigue, and shortness of breath |
| Vaso-occlusive Crises | Obstruction of blood vessels by sickled red blood cells | Acute pain episodes, possible organ damage |
| Splenomegaly | Enlargement of the spleen due to sequestration of red blood cells | Higher risk of infections, sequestration crises |
Knowing these challenges is key to managing SCD well. It helps reduce the risk of serious problems like aplastic crisis.
The Mechanism of Aplastic Crisis in Sickle Cell Disease
Aplastic crisis is a big problem for sickle cell disease patients. It happens when a virus called parvovirus B19 attacks the bone marrow. This makes it stop making red blood cells, making anemia worse.
Impact on Sickle Cell Patients
For sickle cell disease patients, an aplastic crisis is very serious. It causes a big drop in red blood cells. This leads to feeling very tired, looking pale, and having trouble breathing.
These patients already have a problem where their red blood cells don’t last long. An aplastic crisis makes this problem even worse. It can lead to very serious health issues.
Incidence and Risk Factors
Many sickle cell disease patients, mostly children, get aplastic crisis. Parvovirus B19 is the main cause. This virus spreads fast among kids. Adults with sickle cell disease can also get it, but it’s less common.
Being young and having sickle cell disease are big risks. The table below shows these risks and what they mean.
| Risk Factor | Implication |
| Parvovirus B19 Infection | Primary trigger for aplastic crisis |
| Younger Age | Increased susceptibility due to a less developed immune system |
| Sickle Cell Disease | An underlying condition that complicates anemia during an aplastic crisis |
It’s important to know about aplastic crisis in sickle cell disease. Knowing the signs and causes helps doctors act fast. This can make the crisis less severe.
Causes of Aplastic Crisis
Knowing what causes aplastic crisis is key to treating sickle cell disease patients. Aplastic crisis is a serious issue that can cause severe anemia. Finding out what triggers it is vital for good care.
Parvovirus B19 Infection
Parvovirus B19 is a major cause of aplastic crisis in sickle cell disease patients. This virus attacks the cells that make red blood cells, stopping their production. It’s very contagious and spreads fast, mainly in crowded places.
Key aspects of parvovirus B19 infection include:
- High contagion rate
- Direct impact on red blood cell production
- Temporary but severe effect on erythropoiesis
Other Triggering Factors
While parvovirus B19 is the main cause, other things can also lead to aplastic crisis. These include:
- Exposure to certain chemicals or toxins
- Use of specific medications that affect bone marrow function
- Other viral infections that impact erythropoiesis
These factors can make the crisis worse. Knowing about them is important for preventing and managing the condition.
Pathophysiological Cascade
The process that happens after the triggers involves many complex steps. When parvovirus B19 infects the cells that make red blood cells, it stops their production. This leads to a quick drop in hemoglobin levels, which is bad for patients with sickle cell disease.
The cascade can be summarized as follows:
| Trigger | Effect on Erythropoiesis | Clinical Outcome |
| Parvovirus B19 Infection | Cessation of red blood cell production | Severe anemia |
| Chemical/Toxin Exposure | Suppression of bone marrow activity | Aplastic crisis |
| Certain Medications | Impact on erythroid progenitor cells | Reduced hemoglobin levels |
Understanding this process is key to finding effective treatments for aplastic crisis.
Clinical Presentation and Symptoms
An aplastic crisis in sickle cell disease starts with clear symptoms that need quick medical help. We’ll cover the main signs and symptoms of this condition.
Early Warning Signs
Early signs of aplastic crisis include looking pale, feeling very tired, and having a fast heartbeat. These happen because the bone marrow stops making red blood cells. This makes the anemia worse.
Key early warning signs also include feeling short of breath and dizzy. This is because the body’s tissues don’t get enough oxygen. Spotting these signs early is key to quick action.
Severe Manifestations
As aplastic crisis gets worse, severe manifestations appear. These include being very pale, extremely tired, and facing serious risks. Tension can cause heart failure if not treated right away.
In some cases, patients’ hemoglobin levels drop a lot. They might need a blood transfusion right away to avoid serious problems.
Complications if Left Untreated
If aplastic crisis isn’t treated, it can cause big problems. These include heart failure, damage to organs from lack of oxygen, and even death. This shows why quick diagnosis and treatment are so important.
We’ve listed the possible complications and how to handle them in the table below:
| Complication | Description | Management |
| Heart Failure | Severe anemia can lead to heart failure due to the heart’s increased workload. | Immediate transfusion, supportive care |
| Organ Damage | Prolonged hypoxia can cause damage to vital organs. | Prompt oxygen therapy, management of the underlying condition |
| Death | An untreated aplastic crisis can be fatal. | Emergency medical intervention, hospitalization |
In summary, aplastic crisis in sickle cell disease shows clear signs that need quick action. Recognizing and treating these signs early can prevent serious problems.
Diagnosis of Aplastic Crisis
Understanding how to diagnose aplastic crisis is key to quick and effective treatment. This diagnosis involves a detailed check-up. It includes lab tests and a clinical assessment.
Laboratory Findings
Laboratory tests are vital in diagnosing aplastic crisis. A complete blood count (CBC) and reticulocyte count are key. They help measure anemia and bone marrow function.
| Laboratory Test | Expected Finding in Aplastic Crisis |
| Complete Blood Count (CBC) | Severe anemia, often with low hemoglobin levels |
| Reticulocyte Count | Low reticulocyte count, indicating reduced bone marrow activity |
Imaging Studies
Imaging studies also have a role in diagnosis, but it’s mainly to support the findings. They help rule out other conditions.
Differential Diagnosis
Differential diagnosis is important. It helps tell aplastic crisis apart from other similar conditions. This includes other anemias or bone marrow failure syndromes.
- Aplastic anemia
- Other bone marrow failure syndromes
- Severe anemia due to other causes
Healthcare providers use lab results, clinical evaluation, and differential diagnoses. This way, they can accurately diagnose aplastic crisis. Then, they can start the right treatment.
Treatment and Management Approaches
Aplastic crisis in sickle cell disease needs quick and supportive care. This helps manage the condition well and stops more problems. We will look at the different treatments and care plans doctors use for patients with this issue.
Immediate Interventions
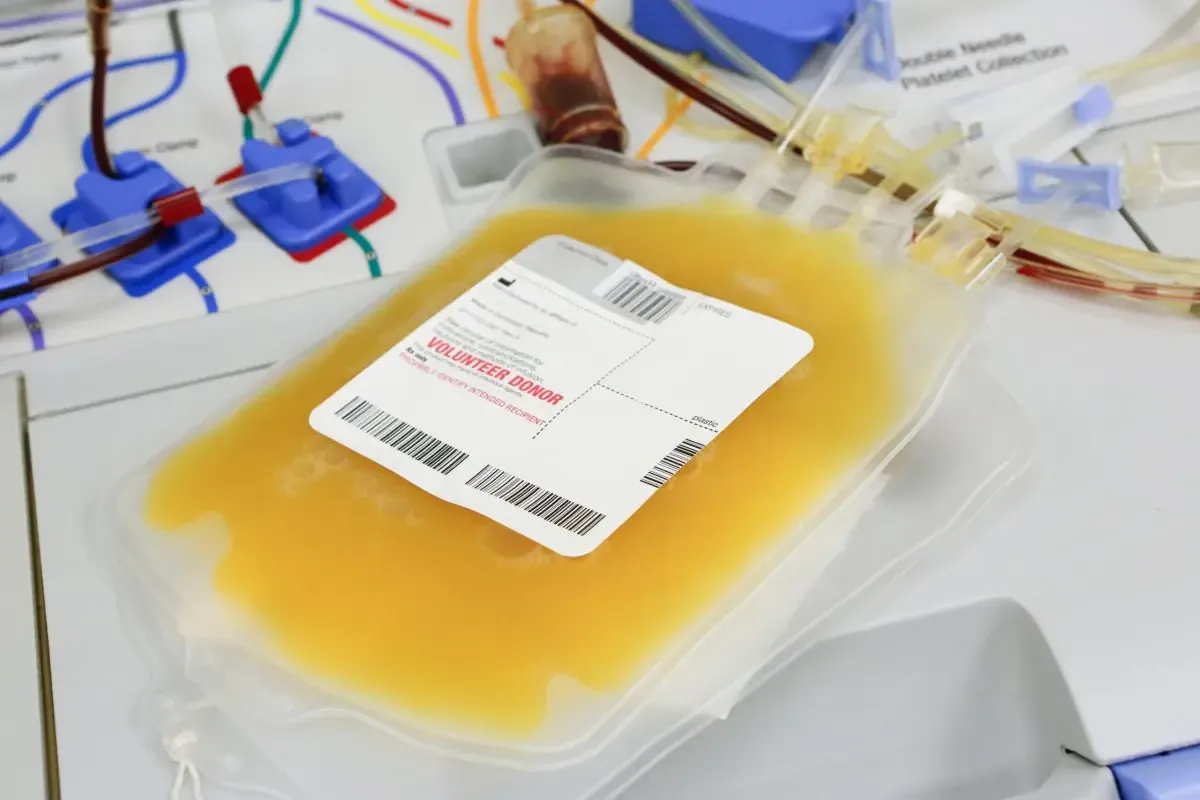
Quick actions are key in handling aplastic crisis. Supportive care, like blood transfusions, is often needed to keep the patient stable. These steps help ease symptoms and stop the condition from getting worse.
“The timely administration of blood transfusions can significantly improve outcomes in patients with aplastic crisis,” as noted by experts in the field.
Supportive Care
Supportive care is very important in managing aplastic crisis. It includes blood transfusions and watching for complications. Keeping a close eye on the patient’s health is vital to change treatment plans if needed.
- Regular blood tests to check hemoglobin levels
- Watching for signs of infection or other issues
- Changing treatment plans based on how the patient responds
Long-term Management Considerations
Long-term care for aplastic crisis focuses on the underlying causes and preventing future episodes. This might mean managing sickle cell disease with medicine and lifestyle changes. Teaching patients about sticking to treatment plans is key to long-term success.
In summary, treating and managing aplastic crisis in sickle cell disease needs a detailed and varied approach. Understanding immediate actions, supportive care, and long-term plans helps doctors improve patient outcomes and life quality.
Aplastic Crisis vs. Aplastic Anemia: Key Differences
It’s important to know the difference between aplastic crisis and aplastic anemia. Both affect blood cell production but have different causes and treatments. Accurate diagnosis is key to proper care.
Differentiating Pathophysiology
Aplastic anemia is a long-term condition where the bone marrow fails to make blood cells. This can happen due to autoimmune diseases, toxins, or infections. An aplastic crisis, on the other hand, is a short-term issue. It’s often caused by Parvovirus B19 infection in people with sickle cell disease.
The main difference is in how long the bone marrow is affected. Aplastic anemia is a long-term problem with many causes. An aplastic crisis is a short-term event.
Clinical Presentation Comparison
Aplastic anemia leads to symptoms like tiredness, infections, and bleeding. This is because the body lacks blood cells for a long time. An aplastic crisis, by contrast, causes sudden, severe anemia. Symptoms include pale skin, tiredness, and heart problems.
Treatment Approach Variations
Treatment for aplastic anemia might include drugs to suppress the immune system, bone marrow transplants, or blood transfusions. For an aplastic crisis, the focus is on treating the cause, like Parvovirus B19, and giving blood transfusions until it passes.
Understanding the specific cause of each condition is essential for effective treatment.
Conclusion
We’ve looked into the details of aplastic crisis in sickle cell disease. It’s different from aplastic anemia. Aplastic crisis can happen when someone with sickle cell disease gets parvovirus B19. This leads to a big drop in red blood cells.
It’s key to know how aplastic crisis works and what it looks like. This helps doctors find it early and treat it right. Aplastic crisis is special because it often happens in people with sickle cell disease.
Doctors can now give better care by knowing the differences between these conditions. It’s vital to watch closely for signs of aplastic crisis in sickle cell patients. Quick action can stop serious problems.
FAQ
What is an aplastic crisis in sickle cell disease?
An aplastic crisis is a sudden drop in red blood cell production in sickle cell disease. It’s often caused by a parvovirus B19 infection.
How is aplastic crisis different from aplastic anemia?
Aplastic crisis is a short-term condition linked to infections. Aplastic anemia, on the other hand, is a long-term bone marrow failure.
What are the symptoms of an aplastic crisis?
Symptoms include severe anemia, fatigue, and shortness of breath. These can be life-threatening if not treated.
How is aplastic crisis diagnosed?
Doctors use lab tests like complete blood counts and reticulocyte counts. These tests show how severe the anemia and bone marrow suppression are.
What is the role of parvovirus B19 in aplastic crisis?
Parvovirus B19 infection is a common cause of aplastic crisis in sickle cell disease. It temporarily stops red blood cell production in the bone marrow.
How is aplastic crisis treated?
Treatment includes blood transfusions to manage severe anemia. This helps prevent complications until the bone marrow recovers.
Can aplastic crisis be prevented?
Preventing aplastic crisis is not guaranteed. But avoiding infections and getting medical care early can help reduce the risk.
What is the prognosis for individuals with aplastic crisis?
The outlook is good with prompt and proper treatment. Some may face recurring episodes or long-term issues, though.
How does aplastic crisis affect patients with hemolytic disorders?
Aplastic crisis can severely affect those with hemolytic disorders like sickle cell disease. It worsens anemia and raises the risk of complications.
What is the difference between a hemolytic crisis and an aplastic crisis?
Hemolytic crisis is the rapid destruction of red blood cells. Aplastic crisis is a sudden drop in red blood cell production. Both can happen in sickle cell disease
References:
- Borhade, M. B. (2024). Aplastic Crisis in Sickle Cell Disease. In Sickle Cell Crisis – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK526064/