Last Updated on November 20, 2025 by Ugurkan Demir

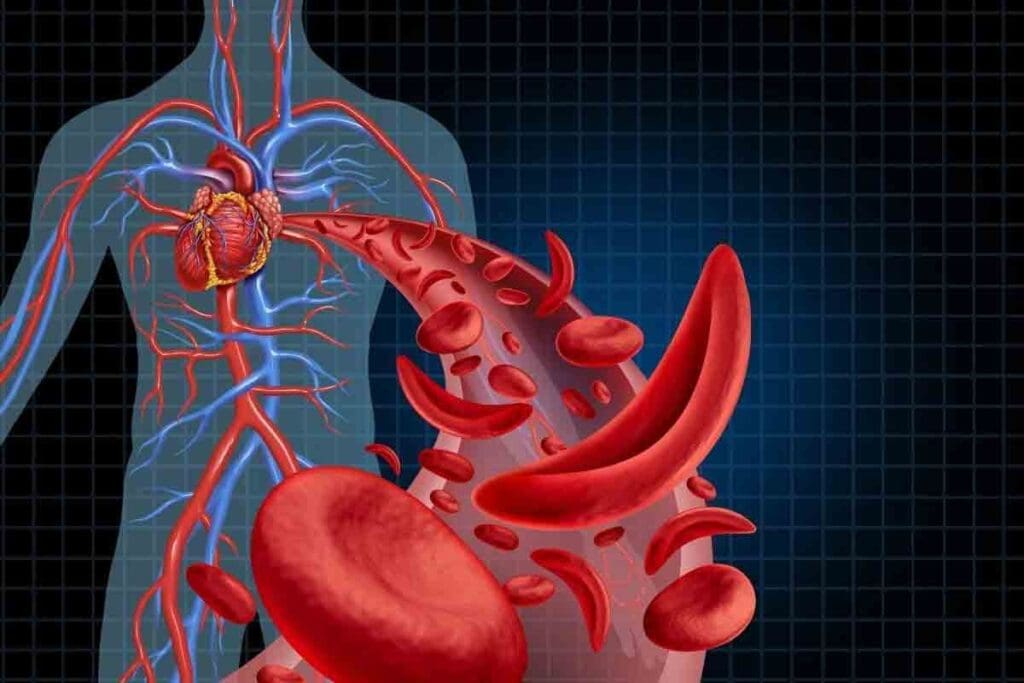
Sickle cell disease is a blood disorder passed down through families. It makes red blood cells look like sickles under certain conditions. An aplastic crisis is a serious episode where the bone marrow stops making red blood cells. This usually happens when someone gets parvovirus B19.
This leads to a quick drop in hemoglobin levels. This causes profound anemia.
At Liv Hospital, we offer top-notch care for patients. We use proven methods to handle severe episodes like aplastic crisis. We follow international standards. Knowing the difference between an aplastic crisis and other sickle cell crises is key to good care.

Understanding Sickle Cell Disease Fundamentals
It’s important to know the basics of sickle cell disease to understand its complications. This disease is a genetic disorder that affects how red blood cells carry oxygen. It happens because of a problem with hemoglobin, a key protein in these cells.
Sickle cell disease happens when someone gets two bad copies of the β-globin gene, one from each parent. This leads to abnormal hemoglobin, called hemoglobin S (HbS).
The disease follows an autosomal recessive pattern. This means a person needs two bad genes to have the disease. Carriers, with one good and one bad gene, usually don’t show symptoms but can pass the bad gene to their kids.
Normal red blood cells are flexible and disk-shaped, making it easy for them to move through blood vessels. But, in sickle cell disease, red blood cells become rigid and crescent-shaped because of HbS.
Sickling happens when these abnormal cells face low oxygen levels. They then lose their shape and flexibility. This can block blood flow and cause many problems.
People with sickle cell disease have certain blood values. They often have lower hemoglobin levels and higher counts of young red blood cells. They might also have more white blood cells.
| Hematological Parameter | Normal Range | Sickle Cell Disease Range |
| Hemoglobin (g/dL) | 13.5-17.5 | 6-9 |
| Reticulocyte Count (%) | 0.5-1.5 | 5-15 |
| White Blood Cell Count (×10^9/L) | 4-11 | Often elevated |
Knowing these blood values is key to diagnosing and managing sickle cell disease complications.
It’s important to know the different crisis types in sickle cell disease for better care. This disease has many crisis types, each needing its own care plan.
Sickle cell crises are divided into several types. Vaso-occlusive crises are the most common. They cause severe pain when blood vessels get blocked by sickled red blood cells.
Aplastic crises happen when the bone marrow stops making red blood cells, often due to infections. Sequestration crises cause severe anemia when red blood cells pool in the spleen. Hemolytic crises speed up the destruction of red blood cells.
How often and how severe sickle cell crises are can vary a lot. Some people have many crises, while others have fewer but more serious ones. Things like genetics, environment, and other health issues can affect this.
Knowing these patterns helps doctors create better care plans for each patient. For example, those with many crises might need more pain treatment and closer watch.
The different crises in sickle cell disease greatly affect health and how much healthcare is used. Often, frequent crises can damage organs, lower the quality of life, and increase costs. Managing these crises well is key to avoiding these problems.
Patients with sickle cell disease often need to go to the hospital a lot, visit emergency rooms, and see doctors regularly. Better crisis management can cut down on these visits. This improves patient health and makes healthcare more efficient.
In sickle cell disease, an aplastic crisis is a serious event. It happens when the bone marrow can’t make enough red blood cells. This is a big problem because red blood cells are already in trouble in sickle cell disease.
An aplastic crisis is mainly caused by parvovirus B19 infection. This virus attacks the bone marrow, stopping it from making red blood cells. This leads to a quick drop in red blood cell count, making anemia worse in sickle cell disease.
It’s key to understand how bone marrow suppression works in aplastic crises. This stop in red blood cell production can cause severe anemia. Sometimes, patients need blood transfusions right away.
In sickle cell disease, red blood cells don’t last as long as they should. Normally, they last about 120 days, but in SCD, they can last only 10-20 days. This short lifespan is part of why SCD patients often have chronic anemia.
Because red blood cells don’t last long, any problem with making new ones is a big deal. An aplastic crisis can quickly lead to severe anemia because there are fewer red blood cells to start with.
When red blood cell production stops during an aplastic crisis, it’s a big deal. This happens because red blood cells already don’t last long in sickle cell disease. In healthy people, stopping red blood cell production might not cause severe anemia right away. But in SCD patients, it can lead to a quick shortage of red blood cells, needing fast medical help.
This shows how important it is to catch and treat aplastic crises early in sickle cell disease. Doctors need to watch closely for this complication to avoid serious problems.
Parvovirus B19 is the main cause of aplastic crises in sickle cell disease patients. We will look at how it affects red blood cell production, how it spreads, and other possible causes of aplastic crises. Knowing these details is key to managing and preventing aplastic crises in those at risk.
Parvovirus B19 attacks red cell precursors in the bone marrow, stopping red blood cell production. This can quickly lower hemoglobin levels, which is a big problem for people with sickle cell disease. The virus’s impact on red blood cell production is the main reason for aplastic crises.
As stated by
“The direct invasion of erythroid progenitor cells by Parvovirus B19 results in a transient but significant suppression of erythropoiesis.”
This shows how important the virus’s effect on red blood cell production is.
Parvovirus B19 is very contagious and spreads through coughing, touching, and blood transfusions. The virus can cause outbreaks in places like schools. People usually get sick within 4 to 14 days after getting infected.
While Parvovirus B19 is the main cause, other things can also lead to aplastic crises in sickle cell disease patients. These include other viruses, certain medicines, and toxins. It’s important to find and manage these triggers for full care.
Knowing how an aplastic crisis presents is key to quick medical help in sickle cell disease patients. This crisis happens when red blood cell making stops, often because of infections like parvovirus B19.
The start of an aplastic crisis can be quiet, with signs like fatigue, pallor, and shortness of breath. These come from the severe lack of red blood cells.
As it gets worse, people might feel dizzy, have headaches, and sometimes fever. Spotting these signs early is important for getting medical help fast.
As the crisis gets worse, the lack of red blood cells becomes more apparent. Symptoms can include:
These symptoms show why quick medical care is needed to avoid serious problems.
Telling an aplastic crisis apart from other sickle cell crises or emergencies is important. Unlike vaso-occlusive crises, which cause pain from blocked blood vessels, an aplastic crisis mainly shows severe anemia without much pain.
| Clinical Feature | Aplastic Crisis | Vaso-Occlusive Crisis |
| Primary Symptom | Severe Anemia | Pain |
| Red Blood Cell Production | Halted | Normal or slightly decreased |
| Pain Characteristics | Minimal or absent | Severe, often requiring opioids |
Vaso-occlusive crises in sickle cell disease are serious. They happen when sickled red blood cells block blood vessels. This causes tissues to not get enough blood.
The cause of vaso-occlusive crises is complex. It involves sickled red blood cells, the blood vessel walls, and inflammation. Sickled red blood cells stick to the blood vessel walls, causing blockages.
Pain from vaso-occlusive crises can differ for each person. It often starts suddenly and is very painful. It usually hits the back, chest, and limbs.
The pain can spread or stay in one place. It depends on where the blockage is.
Vaso-occlusive crises not only cause sudden pain. They also risk harming organs in the long run. Organs like the spleen, kidneys, and lungs can get damaged over time.
“Repeated vaso-occlusive crises can result in chronic organ damage, significantly impacting the quality of life for patients with sickle cell disease.”
This shows why it’s key to manage these crises well and fast.
It’s key for doctors to know the difference between aplastic and vaso-occlusive crises in sickle cell disease. Both are serious, but they show up differently and need different treatments.
Aplastic crises happen when red blood cell production suddenly drops, often because of parvovirus B19. The main symptom is severe anemia, causing fatigue, shortness of breath, and looking pale appearance. On the other hand, vaso-occlusive crises cause severe pain because sickled red blood cells block blood vessels.
The pain from vaso-occlusive crises is very bad and can also cause fever, swelling, and tenderness. Unlike aplastic crises, vaso-occlusive crises usually don’t cause a lot of anemia unless there are other problems.
Managing pain is very important for vaso-occlusive crises. Doctors use strong pain medicines, like opioids, to help. Aplastic crises don’t usually need pain treatment unless there are other issues.
For aplastic crises, the focus is on treating the anemia’s cause, like parvovirus B19. Doctors also give blood transfusions to help tissues get enough oxygen.
Aplastic crises usually get better once the cause is treated and red blood cell production starts again. How long it takes to get better depends on how bad the anemia is and the patient’s health.
Vaso-occlusive crises are harder to predict. Pain can vary a lot in how bad and long it lasts. Doctors use pain relief and ways to prevent future episodes, like staying hydrated and avoiding triggers.
Knowing these differences helps doctors give better care. It improves life quality for people with sickle cell disease.
Understanding the diagnostic markers for sickle cell crises is key to good patient care. Lab tests are vital in diagnosing and differentiating between various types of sickle cell crises. They guide clinical management and treatment decisions.
A complete blood count (CBC) is a basic test for patients with sickle cell disease during a crisis. It gives important info on blood cell parameters like hemoglobin levels, hematocrit, white blood cell count, and platelet count.
In an aplastic crisis, the CBC shows a big drop in hemoglobin levels. This is because red blood cell production stops temporarily. On the other hand, a vaso-occlusive crisis might have different hemoglobin levels. It often has an elevated white blood cell count due to inflammation.
| Parameter | Aplastic Crisis | Vaso-Occlusive Crisis |
| Hemoglobin | Significantly decreased | Variable |
| White Blood Cell Count | Normal or slightly elevated | Often elevated |
| Reticulocyte Count | Low | Elevated |
The reticulocyte count is a key marker for differentiating between sickle cell crisis types. Reticulocytes are young red blood cells, and their count shows how active the bone marrow is.
In an aplastic crisis, the reticulocyte count is low, showing a stop in red blood cell production. But in a vaso-occlusive crisis, the count is high. This is because the bone marrow is working hard to replace destroyed red blood cells.
“The reticulocyte count is a valuable tool in assessing the bone marrow’s response to anemia and differentiating between various types of sickle cell crises.”
– Expert in Hematology
More lab tests might be needed for a full assessment of sickle cell crises. These include:
These tests, along with clinical evaluation, help healthcare providers accurately diagnose and manage sickle cell crises. This improves patient outcomes.
Managing aplastic crises in sickle cell disease patients is key. It involves several strategies to better patient outcomes. Aplastic crisis, caused by parvovirus B19, stops red blood cell production, worsening anemia. Our goal is to act quickly and effectively.
Blood transfusions are vital in aplastic crisis management. They help improve oxygen delivery to tissues. We consider transfusion when hemoglobin levels drop significantly or when anemia is severe.
The decision to transfuse depends on the patient’s condition and anemia severity. We also look for symptoms like dyspnea or tachycardia.
| Transfusion Threshold | Clinical Considerations |
| Hemoglobin < 5 g/dL or a significant drop from baseline | Assess for signs of severe anemia, such as dyspnea, tachycardia, or fatigue |
| Presence of cardiovascular instability | Consider the patient’s overall clinical condition and comorbidities |
Supportive care is vital in aplastic crisis management. It aims to alleviate symptoms and prevent complications. This includes monitoring vital signs, ensuring hydration, and rest.
“Supportive care is critical in aplastic crisis management. It helps alleviate symptoms and improves outcomes.”
— Expert Opinion
It’s important to manage the parvovirus B19 infection. While it’s often self-limiting, supportive care and intravenous immunoglobulin may be needed for severe cases.
Hospital admission is often necessary for aplastic crisis patients. It allows for close monitoring and quick response to complications. Monitoring includes blood counts, reticulocyte counts, and organ function assessment.
Managing vaso-occlusive crises requires a mix of pain relief, staying hydrated, and supportive care. It’s key to ease pain and prevent serious issues in sickle cell disease patients.
Pain control is a big part of managing these crises. We use different pain medicines, from NSAIDs to opioids, based on the pain’s intensity. Prompt pain assessment and individualized pain management plans are vital for proper care.
For severe pain, opioids might be needed. We watch closely to avoid too little or too much medicine. We also use other medicines like acetaminophen or NSAIDs to help with pain.
Drinking enough water is key to managing these crises. It helps blood flow better and lowers sickled red blood cells. We suggest drinking water, but sometimes IV fluids are needed, mainly in serious cases.
We check how well patients are hydrated by looking at urine output and specific gravity. Careful fluid management is important to avoid too much water, which can cause problems like acute chest syndrome.
Oxygen therapy is important, especially if patients show signs of low oxygen or acute chest syndrome. Rest is also key, as too much activity can make things worse.
We also focus on managing any infections or triggers that might have caused the crisis. Good care means looking at the patient’s overall health and any extra challenges they face.
New research is looking into better ways to manage vaso-occlusive crises. This includes new medicines to stop sickling and improve blood flow, and new pain management methods.
We aim to keep up with these new findings to give our patients the best care. As new research comes out, we update our treatment plans to use the latest advice.
Effective prevention and education are key in managing Sickle Cell Disease. By teaching patients and caregivers, we can improve their lives and lower the risk of problems.
Vaccinations against infections like pneumococcus and influenza are important for Sickle Cell patients. Keeping up with vaccinations helps prevent infections that can cause crises. Patients should follow their doctor’s vaccination schedule, which includes shots for pneumococcal disease, influenza, and other infections.
Preventing infections is also vital. This means washing hands often, staying away from sick people, and keeping things clean. Telling patients about these habits can help them avoid infections.
Patients with Sickle Cell Disease must know the signs of different crises. Spotting these signs early helps prevent serious problems. We teach them to look out for symptoms like pale skin, tiredness, or severe pain. If they see these signs, they should get medical help right away.
Having an emergency plan is critical for managing Sickle Cell Disease. This plan should list emergency contacts, the nearest hospital, and what to do in a crisis. Reviewing and updating this plan with doctors is important to keep everyone ready.
By focusing on prevention and education, we can greatly improve the lives of those with Sickle Cell Disease. Teaching them how to manage their condition helps them live healthier lives.
Managing sickle cell disease needs a full plan. This includes knowing the condition, spotting crises early, and taking steps to prevent them. We’ve looked at the different types of crises and how to handle them.
Good management means knowing the signs of a crisis and acting fast. Understanding sickle cell disease helps people with it live better lives. It’s key to have a team approach, with regular doctor visits, shots, and learning about the disease.
Living with sickle cell disease also means having a plan for emergencies and getting support. Using these strategies helps manage the disease and lowers the chance of serious problems. We urge patients to team up with their doctors to make a plan that’s just right for them.
By being aware, taking preventive steps, and getting medical help when needed, we can make life better for those with sickle cell disease. Good management helps patients face the challenges of the disease and reach their health goals.
An aplastic crisis is when the bone marrow stops making red blood cells. This leads to severe anemia. It’s often caused by parvovirus B19 infection.
An aplastic crisis stops red blood cell production, causing severe anemia. A vaso-occlusive crisis blocks blood vessels with sickled red blood cells, causing pain and organ damage.
Symptoms include fatigue, shortness of breath, and pale skin. Severe anemia can occur. Early signs are subtle, so quick medical check-ups are key.
Tests like a complete blood count (CBC) and reticulocyte count are used. These check anemia levels and bone marrow response. More tests may find the cause.
Treatment includes blood transfusions to help tissues get oxygen. Supportive care manages symptoms. Treating the cause, like parvovirus B19, is also important.
While not all can be prevented, steps like parvovirus B19 vaccination help. General infection prevention also reduces risk.
Parvovirus B19 is the main cause of aplastic crises in sickle cell disease. It infects and stops red blood cell production in the bone marrow.
Sickle cell disease shortens red blood cell lifespan. Their abnormal shape leads to early destruction.
Vaso-occlusive crises happen when sickled red blood cells block blood vessels. This causes pain and can damage organs. Treatment includes pain relief, hydration, and oxygen therapy.
Education helps patients recognize early signs of crises. It teaches the importance of preventive measures like vaccinations. It also helps create emergency plans to manage the disease well.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!