Last Updated on November 27, 2025 by Ugurkan Demir

What is a safe apnea apneic time for breathing pauses? Learn about the acceptable duration of apnea in both children and adults.
At Liv Hospital, we know that safe apnea time is key in both kids and adults. Apnea, or when breathing stops, is very important for safety during airway care.
Safe apnea time is how long a person can go without breathing before their blood oxygen drops too low. Healthy adults can usually go about 8 minutes without breathing before it’s dangerous. But, adults who are sick or obese might only have 2.7 minutes before it’s critical.
It’s very important for doctors to know these differences. This helps them manage apnea-related risks better in kids and adults. We make sure to use the right rules for each age group to keep everyone safe.
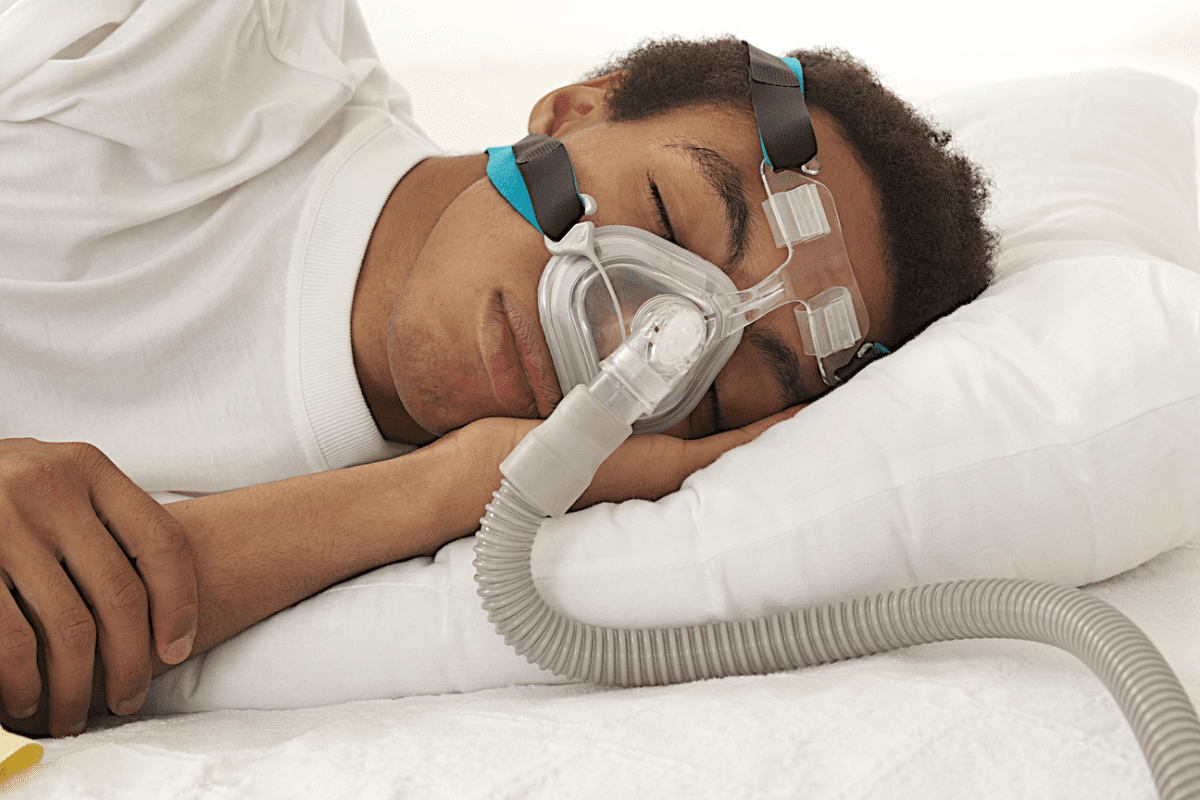
Apnea, or the pause in breathing, is a big challenge in healthcare. It’s important to know about safe apnea time. This is key for doctors and nurses.
Apnea is when someone stops breathing for 20 seconds or more. It can also happen if there are signs like slow heart rate, blue skin, or floppy muscles. This shows how serious apnea can be.
Key characteristics of apnea include:
Safe apnea time is how long a person can stop breathing without getting too low on oxygen. This is very important in places like the operating room or intensive care.
The factors influencing safe apnea time include:
In places like the operating room, knowing about safe apnea time is very important. Doctors and nurses need to know this to keep patients safe.
“The ability to predict and manage safe apnea time is critical in preventing adverse outcomes in patients undergoing anesthesia and critical care.” –
Expert in Anesthesiology
Understanding apnea and safe apnea time helps doctors and nurses take better care of patients. This can lead to better health outcomes for everyone.

The body’s response to apnea is shaped by several key physiological mechanisms. Understanding these mechanisms is key to knowing the safe apnea time for different groups. This is true for both kids and adults.
Oxygen reserve capacity is vital in figuring out safe apnea time. This reserve is mainly in the lungs’ functional residual capacity (FRC) and in the blood and muscles. Children have a smaller FRC compared to adults, affecting their oxygen during apneic episodes.
Metabolic rate greatly affects oxygen use. Children use oxygen faster per body weight than adults during apnea. This fast use of oxygen leads to hypoxemia in kids quickly.
The respiratory system’s development impacts safe apnea time. In kids, lungs and airways are growing, affecting gas exchange. The smaller airways in kids are more prone to blockage, making apneic episodes harder.
Healthcare providers need to understand these mechanisms to manage apnea well across ages. By knowing what affects safe apnea time, they can tailor care to meet patient needs.
In healthy adults, knowing the safe apnea time is key for doctors during medical procedures. This time changes based on how well the patient is preoxygenated and their health.
For healthy adults, the safe apnea time is about 8 minutes with good preoxygenation. Preoxygenation is very important. It builds up the body’s oxygen stores, making it safer for longer without breathing.
Studies show that with the right preoxygenation, healthy adults can safely hold their breath for about 8 minutes. This 8-minute mark is a key goal for safe apnea during medical procedures. But, it can change based on the patient’s health.
Several things help make healthy adults more tolerant of not breathing. These include:
By focusing on these areas, doctors can make procedures safer for patients who need to hold their breath.
Adults with health issues have a shorter safe apnea time. This means they need careful management. Health conditions can greatly affect how well an adult can handle apnea. It’s key for doctors to know these factors.
Moderately ill adults can usually handle apnea for about 5 minutes. Their health is not as strong, leading to less oxygen and more need for energy.
When dealing with apnea in these patients, we must be careful. This helps avoid bad outcomes.
Obese adults can only handle apnea for about 2.7 minutes. This is because they have less room in their lungs and use more oxygen.
It’s important to understand these risks. This helps us give the right care to obese patients during procedures that might involve apnea.
Other things can also shorten safe apnea time in adults. These include:
Knowing these risk factors helps doctors take steps to manage apnea risks better.
Pediatric apnea is when a child stops breathing for a while. It’s important to understand this condition well. Apnea in kids is when they stop breathing for 20 seconds or more. Or, it’s a shorter pause if it’s with other signs that worry doctors.
The 20-second threshold is key in spotting apnea in children. It shows a big pause in breathing that doctors watch closely. Studies and guidelines often use this time to figure out and treat apnea in kids.
Other signs are important too when looking at apnea in kids. These include bradycardia (a slow heart rate), cyanosis (skin turning blue because of not enough oxygen), and hypotonia (muscles feeling weak). Even if the pause is short, these signs mean something serious might be happening.
Doctors use a detailed check-up to diagnose apnea in kids. They look at how long the breathing stops and any other signs. They also think about the child’s age, past health, and current health. This careful look helps find the cause of apnea and how to treat it.
In short, knowing about pediatric apnea is complex. It involves understanding the official definitions and how serious it is. By focusing on the 20-second mark and other symptoms, doctors can spot and treat this serious issue in children better.
It’s important to know why kids quickly lose oxygen during apneic periods. Their bodies are different from adults, making them more at risk. This is why managing apnea in kids is so critical.
Kids’ lungs and airways are smaller and more flexible. This makes it harder for them to keep oxygen levels up during apnea. Developmental respiratory physiology is key here. Their lungs and airways are not as big or efficient as adults’, leading to faster oxygen use.
Several factors lead to quick oxygen loss in kids:
Kids use more oxygen compared to their size. This means their oxygen stores run out faster during apnea. So, kids are more likely to quickly lose oxygen.
The functional residual capacity (FRC) is the air left in lungs after a normal breath. Kids have less FRC than adults, which means less oxygen reserve. When they stop breathing, this small reserve is used up fast, causing quick oxygen loss.
Healthcare providers need to understand these differences to better manage apnea in kids. Knowing why kids lose oxygen quickly helps doctors find ways to reduce these risks.
The safe apnea time in children is greatly affected by their physical traits. These include age, weight, and height. Knowing these connections is key for healthcare workers to handle apnea risks well in kids.
As kids grow, how well they can handle apnea changes. Infants and younger kids have a shorter safe apnea time than older kids and adults. This is because of differences in how fast they metabolize, their lung size, and how their breathing system develops.
A study on pediatric anesthesia found that neonates and infants can’t handle apnea as well. They need to be watched closely during medical procedures. As kids get older, their safe apnea time gets longer. But it’s always important to keep an eye on it, mainly in medical settings.
Body weight also plays a big role in safe apnea time in kids. Lighter kids tend to have a shorter safe apnea time. This is because they have smaller oxygen stores and a faster metabolism compared to their body size.
Weight Category | Average Safe Apnea Time |
Less than 10 kg | 1.5 minutes |
10-20 kg | 2.5 minutes |
More than 20 kg | 3.5 minutes |
The height of a child and their lung size are linked to their safe apnea time. Taller kids usually have bigger lungs, which can make their safe apnea time longer. This is something doctors need to know when checking on kids.
“The relationship between height, lung capacity, and safe apnea time in children shows why we need to assess each child differently in pediatric care.”
Medical Expert, Pediatric Pulmonologist
When dealing with apnea in kids, we must think about their physical traits. By knowing how age, weight, height, and safe apnea time are connected, doctors can take better care of their young patients. This helps manage risks and improve health outcomes for kids.
Managing apnea well means understanding the risks in different age groups. We need to know how kids and adults are different to help them better.
Preoxygenation is key before risky procedures. Using a high-flow nasal cannula (HFNC) helps keep oxygen levels up. It’s great for patients at high risk.
Preoxygenation works differently for kids and adults. Kids use more oxygen and have less lung space. So, HFNC is extra helpful for them.
Keeping an eye on patients during risky procedures is vital. We watch with pulse oximetry, capnography, and electrocardiography. This helps us see how their heart and lungs are doing.
We also watch closely with extra tools like invasive blood pressure monitoring. This helps us catch any problems fast.
Even with precautions, apnea can last too long. We’re ready to act fast with bag-valve-mask ventilation and advanced airway methods.
Kids need special emergency plans because of their unique needs. We act quickly to avoid big problems.
Knowing about safe apnea time is key for healthcare workers. It helps them manage risks and give the best care to patients of all ages. We’ve looked at how apnea works, the differences in safe apnea time for kids and adults, and what affects how long someone can go without breathing.
Healthcare providers need to know these differences, mainly when giving anesthesia or in critical care. Good apnea management means using preoxygenation, watching the patient closely, and being ready for emergencies. This is based on the patient’s age and body type.
By using this knowledge, healthcare workers can lower the risk of problems related to apnea. This leads to better results for patients. As medical care gets better, understanding safe apnea time will keep being important for top-notch patient care.
Understanding safe apnea time has big benefits. It makes patients safer during sedation, improves monitoring in risky procedures, and gets healthcare workers ready for emergencies. By using these insights every day, healthcare providers can improve apnea care and help patients get better.
Safe apnea time is how long a patient can stay without breathing without serious harm. It’s key in places like hospitals, where doctors need to handle breathing stops well.
Kids and adults have different safe apnea times because of how their bodies work. Kids can’t hold their breath as long as grown-ups.
Healthy adults’ safe apnea time changes based on how well they breathe before stopping, how much oxygen they have, and their metabolism. Studies say adults can usually hold their breath for about 8 minutes.
Being overweight can make it harder for adults to hold their breath. People who are obese can only hold their breath for about 2.7 minutes.
In kids, apnea means stopping breathing for 20 seconds or more, or if they turn blue or their heart beats slow. Knowing this helps doctors treat it right.
Kids lose oxygen fast when they stop breathing because their lungs are smaller and they breathe faster. This makes it harder for them to keep enough oxygen.
Doctors can handle apnea risks in kids by knowing how age, weight, and height affect breathing. They also use special breathing techniques and watch closely during risky procedures.
Knowing about safe apnea time helps doctors take care of patients better. It lets them make smart choices and be ready for emergencies when breathing stops for a long time.
Preoxygenation helps by building up oxygen in the body. This makes it safer for patients to hold their breath longer.
Watching closely during risky procedures helps catch breathing stops early. This lets doctors act fast and avoid serious problems.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!