Last Updated on November 26, 2025 by Bilal Hasdemir

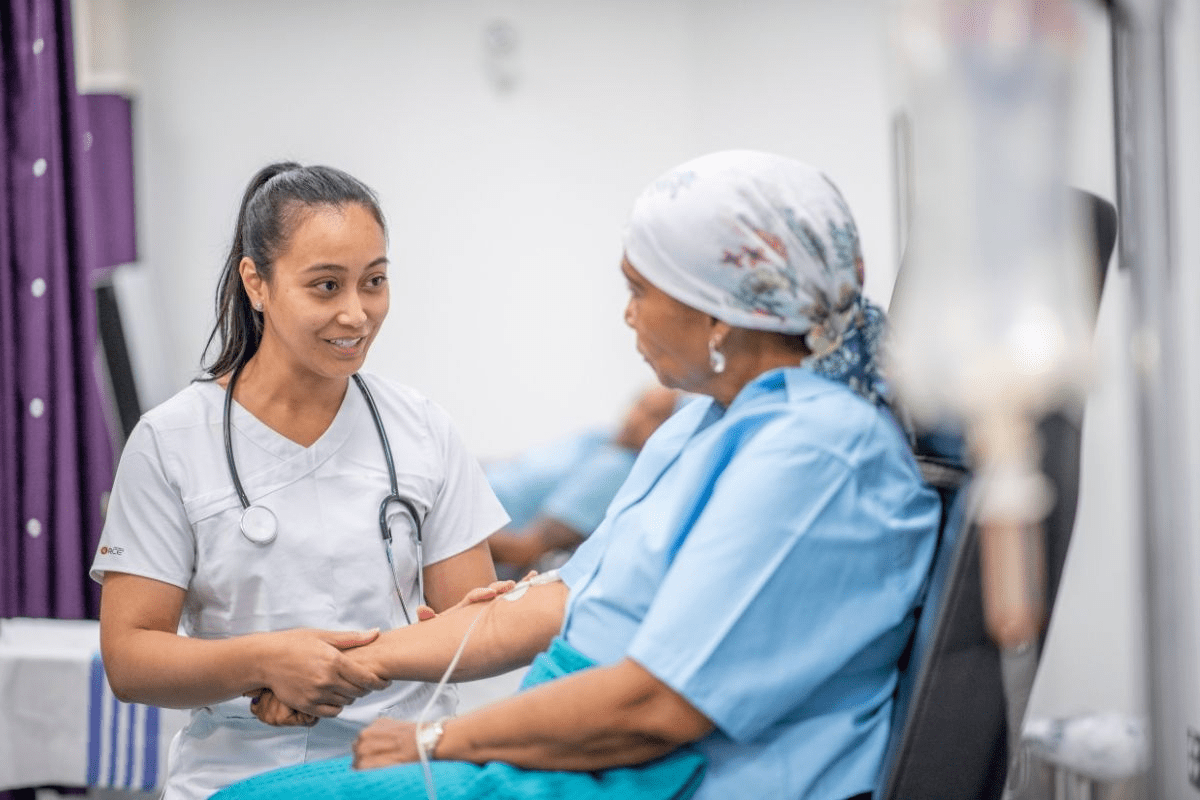
When you face rectal cancer, knowing your treatment options is key. Abdominoperineal resection (APR) is a big surgery for treating low rectal cancers. It’s used when saving the sphincter isn’t possible. Learn 10 key facts about APR surgery. This guide explains abdominoperineal resection for rectal cancer and what patients must know.
This complex surgery removes the sigmoid colon, rectum, and anus. This leads to a permanent colostomy. Liv Hospital is known for its trusted, patient-centered care. They follow global standards and expert protocols, helping patients through rectal cancer surgery.
Key Takeaways
- APR is a major surgical procedure for low rectal cancers.
- The surgery involves removing the sigmoid colon, rectum, and anus.
- A permanent colostomy is a result of the APR procedure.
- Liv Hospital offers patient-focused care for rectal cancer patients.
- Understanding treatment options is key for patients with rectal cancer.
What is APR Surgery: Definition and Clinical Significance

The abdominoperineal resection (APR) is a major surgery for rectal cancer. It removes the anus, rectum, and part of the sigmoid colon. This surgery is for patients with tumors near or in the anal sphincter.
Abdominoperineal Resection Explained
APR surgery is a complex procedure. It combines abdominal and perineal approaches to remove the rectum, anus, and tissues around them. The surgery requires a lot of skill because of the delicate pelvic anatomy.
The surgical team plans carefully to get the best results. They consider the tumor size, the patient’s health, and possible complications.
Key Anatomical Structures Involved
Several important structures are involved in APR surgery:
- The rectum and anus are removed.
- A part of the sigmoid colon is taken out.
- The anal sphincter complex is removed.
- The perineal wound is closed.
Knowing the anatomy is key for surgeons. It helps them navigate the surgery and reduce risks.
Permanent Colostomy as a Surgical Outcome
APR surgery often leads to a permanent colostomy. This means the remaining colon is brought to the abdomen. A stoma is created for stool passage.
Patients need to adjust to life with a permanent colostomy. This includes changes in lifestyle and ongoing stoma care.
Historical Context: From Miles Procedure to Modern Techniques
The Miles procedure was a key step in colorectal surgery’s history. It was named after Sir William Ernest Miles and started in the early 1900s. It was a big leap forward in treating rectal cancer.
Origins of the Miles Procedure
The Miles procedure was a major breakthrough. It removed the rectum and anus through both the belly and the backside. This method was a game-changer back then, as it offered a thorough way to tackle rectal tumors. It was also important because it helped fight local recurrence, a big problem in rectal cancer surgery.
Evolution of Surgical Approaches
Over time, the Miles procedure has seen many changes and upgrades. New surgical methods and a deeper understanding of the body have led to different APR techniques. These new ways aim to make surgery better, cut down on risks, and improve life quality for those with rectal cancer.
Terminology in Contemporary Medical Literature
In today’s medical books, the way we talk about APR surgery has changed. While “Miles procedure” is used, it’s mainly seen as part of APR’s history. Modern texts focus on the technical details and variations of APR, showing the field’s growth. Using the right words is key for doctors to talk clearly and for patients to know their options.
Indications for APR in Rectal Cancer Treatment
APR surgery is often needed for low rectal cancer. This is because the tumor is close to the sphincter complex. The choice to do APR depends on the tumor’s location, how much it affects the sphincter, and if the sphincter can be saved.
Low Rectal Tumors and Sphincter Involvement
APR is usually needed for tumors near or touching the anal sphincter. This makes it hard to keep the sphincter working well.
Preoperative Staging Considerations
Staging before surgery is very important. It helps figure out who will benefit from APR. It looks at the tumor’s size, where it is, and if it’s spreading.
When Sphincter Preservation is Not Feasible
If the tumor is very close to or in the sphincter, saving it might not be possible. In these cases, APR is the best choice. It removes the tumor completely and aims for the best results.
| Indication | Description |
| Low Rectal Tumors | Tumors located in the lower third of the rectum, close to the anal sphincter. |
| Sphincter Involvement | Tumors that abut or involve the anal sphincter complex or levator muscles. |
| Preoperative Staging | Accurate staging to determine tumor size, location, and if it’s spreading. |
Choosing APR for rectal cancer involves looking at many things. These include the tumor’s details, staging before surgery, and if the sphincter can be saved. Understanding these helps doctors decide the best treatment for patients with rectal cancer.
Variations of APR Surgical Procedures
APR surgery has evolved, leading to many different approaches. Each has its own benefits and challenges. These variations help treat rectal cancer better, depending on the tumor’s location and the patient’s condition.
Standard Abdominoperineal Resection
Standard APR is key for treating low rectal cancers. It removes the anus, rectum, and part of the sigmoid colon. This method is chosen for tumors near the anal sphincter or those that have spread to nearby areas.
Anterior Perineal Resection Approach
The anterior perineal resection is a variation of APR. It accesses the tumor from the perineum, reducing the need for big abdominal cuts. This method is good for tumors in the lower rectum, as it’s more precise.
Extralevator and Ischioanal APR Techniques
Extralevator APR dissects more around the levator ani muscles. This might improve cancer treatment results. Ischioanal APR removes ischiorectal fat, helping with tumors in this area. Both show the effort to customize APR surgery for each patient.
APR surgery has many variations, like anterior perineal resection and others. Choosing the right approach based on the tumor and patient factors is key. This helps surgeons improve outcomes and enhance patients’ quality of life after APR surgery.
Preoperative Assessment and Patient Preparation
The success of APR surgery depends a lot on careful preoperative assessment and preparation. A thorough evaluation makes sure patients are ready for surgery. This reduces the chance of complications and improves results.
Diagnostic Imaging Requirements
Diagnostic imaging is key in checking patients before APR surgery. MRI is very helpful in seeing how big the tumor is. It helps decide if the sphincter can be saved and if treatment before surgery is needed.
Multidisciplinary Team Evaluation
A multidisciplinary team is vital for the best care. This team includes surgeons, radiologists, oncologists, and more. They work together to create a treatment plan that fits the patient’s needs.
Neoadjuvant Therapy Considerations
Neoadjuvant therapy, like chemotherapy and radiation, might be suggested. It aims to make tumors smaller and lower the chance of them coming back. The choice to use it depends on the tumor’s stage and where it is.
Stoma Site Marking and Patient Education
Marking the stoma site before surgery is very important. It helps place the stoma in the best spot for comfort and quality of life after surgery. Teaching patients about stoma care is also key in getting them ready for surgery.
A well-prepared patient can better face the challenges of APR surgery and recovery. By focusing on preoperative assessment and preparation, healthcare providers can improve patient outcomes and quality of life.
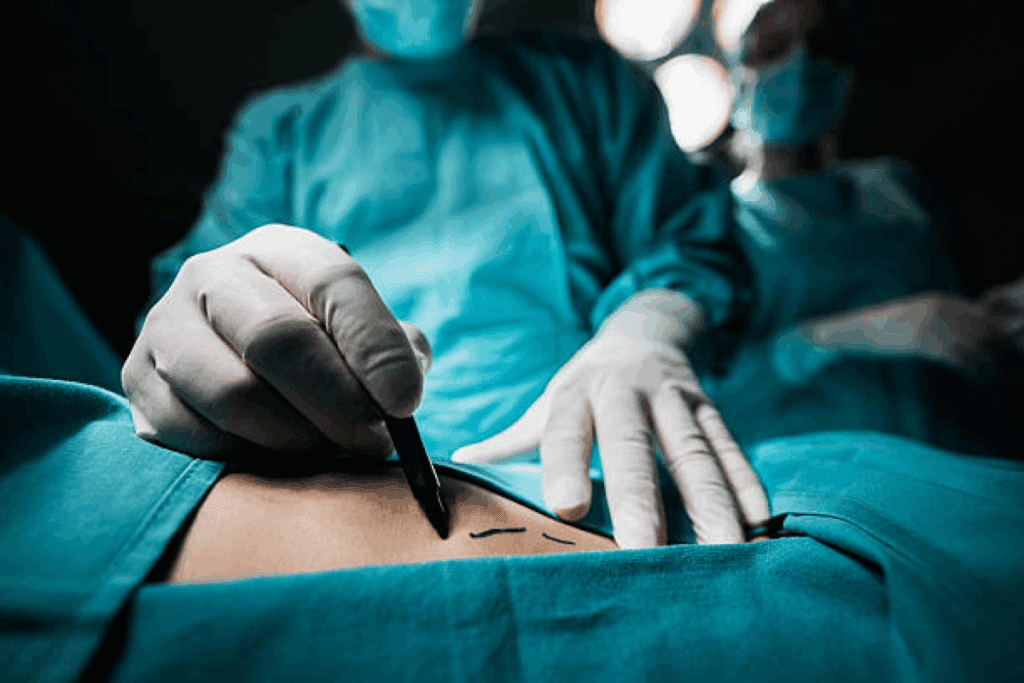
The APR Surgery Procedure: Technical Aspects
APR surgery involves many important steps. It includes the abdominal and perineal phases. This complex process needs a lot of skill and precision for success.
Abdominal Phase of the Operation
The first part of APR surgery is the abdominal phase. Here, the surgeon enters the abdominal cavity. They move the rectum and sigmoid colon carefully.
Key steps in the abdominal phase include:
- Making a midline incision to access the abdominal cavity
- Mobilizing the rectum and sigmoid colon
- Ligating the inferior mesenteric artery
Perineal Phase Techniques
The perineal phase is when the anus and surrounding tissues are removed. The surgeon must be very careful to avoid damaging nearby areas.
The perineal phase requires meticulous technique, as it involves:
- Dissection of the perineal skin and underlying tissues
- Removal of the anus and surrounding tissues
- Closure of the perineal wound
Colostomy Formation and Management
After removing the rectum and anus, a permanent colostomy is made. The surgeon brings the sigmoid colon to the abdomen’s surface. It is then sutured in place.
Effective colostomy management is key for recovery. It includes:
- Proper stoma care and hygiene
- Management of colostomy bags
- Dietary adjustments to manage bowel movements
Understanding APR surgery’s technical aspects helps surgeons improve patient care. It reduces the risk of complications.
Postoperative Recovery and Possible Complications
Recovering after APR surgery is a detailed process. It aims to manage possible issues. Good care during this time is key to better outcomes and a better life.
Immediate Postoperative Care
Right after surgery, we focus on pain, watch for problems, and check the colostomy. Managing pain well is very important. We use medicines and other ways to help.
A colorectal surgeon said, “A team effort is vital. We meet the patient’s physical and emotional needs.”
“Pain management is not just about medication; it’s about creating a supportive environment that fosters recovery.”
Common Complications
After APR surgery, some common issues are infection, bowel blockage, and problems with the perineal wound. Spotting and treating these early is key to handling them well.
| Complication | Prevalence | Management Strategy |
| Infection | 15-20% | Antibiotics, drainage |
| Bowel Obstruction | 10-15% | Conservative management, surgery |
| Perineal Wound Complications | 20-30% | Wound care, flap reconstruction |
Long-term Quality of Life Considerations
Long-term life quality after APR surgery depends on managing the colostomy, body image, and sexual function. Supportive care and counseling play a big role in improving life for patients.
As APR colorectal surgery gets better, we focus more on better recovery and fewer complications.
Understanding recovery and complications helps healthcare providers give better care. This improves life for those having APR surgery.
Advances in APR Colorectal Surgery and Modern Approaches
APR surgery has seen big improvements, leading to better patient results and a better life quality. The field of colorectal surgery has made big strides, with a focus on Abdominoperineal Resection (APR) for rectal cancer.
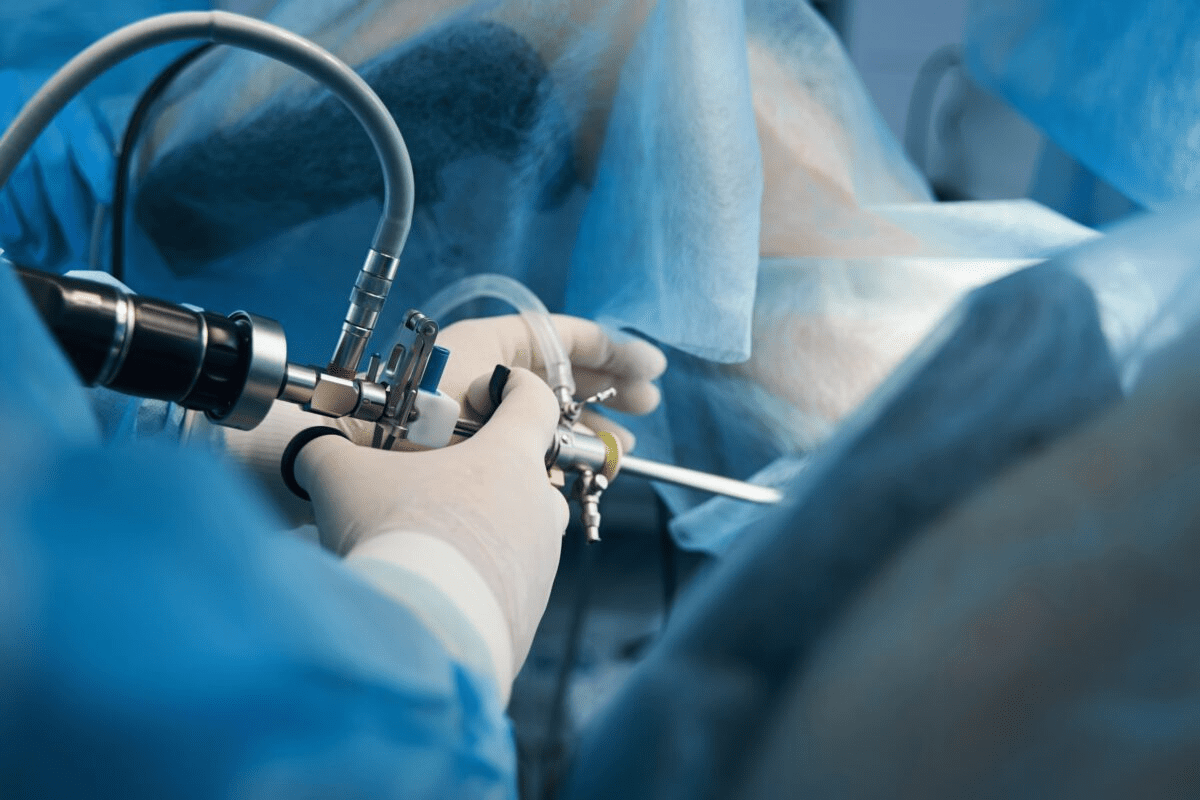
Minimally Invasive Techniques
One big step forward is the use of minimally invasive techniques. These include laparoscopic and robotic-assisted surgery. They cut down on pain, shorten recovery time, and reduce scars. Minimally invasive APR is now a top choice for many surgeons, aiming to better patient results.
Enhanced Recovery After Surgery (ERAS) Protocols
The use of Enhanced Recovery After Surgery (ERAS) protocols is also key in modern APR surgery. ERAS protocols are based on solid evidence to improve care before, during, and after surgery. They help reduce complications and shorten hospital stays.
“The integration of ERAS protocols into our surgical practice has significantly improved patient outcomes and reduced healthcare costs.” – Medical Expert, Colorectal Surgeon
Improvements in Oncological Outcomes
APR surgery has also seen better oncological outcomes. Neoadjuvant therapies, precise surgery, and better care after surgery have all helped. These efforts have led to better survival rates and fewer cancer comebacks.
| Outcome | Traditional APR | Modern APR Approaches |
| Recovery Time | 6-8 weeks | 3-5 weeks |
| Complication Rate | 20-30% | 10-20% |
| 5-Year Survival Rate | 60-70% | 70-80% |
In conclusion, APR colorectal surgery has greatly improved patient outcomes and life quality. As the field keeps growing, we can expect even more advancements in surgery and care.
Conclusion: Current Trends and Future Directions in Rectal Cancer Surgery
APR surgery is key in treating rectal cancer. It keeps getting better with new surgical methods and care before and after surgery. The future will see even more improvements in these areas.
Right now, we’re working hard to make patients’ lives better after surgery. We’re looking into making treatments more tailored to each person. This might use new imaging tech and team work.
APR surgery is very important for treating rectal cancer. As doctors and healthcare teams keep improving, patients will get even better care. This will help make life after surgery better for everyone.
FAQ
What is APR surgery?
APR (Abdominoperineal Resection) surgery is a major operation. It removes the anus, rectum, and part of the sigmoid colon. This results in a permanent colostomy. It’s used for low rectal cancers where saving the sphincter isn’t possible.
What is the historical context of APR surgery?
APR surgery started with the Miles procedure in the early 20th century. Over time, the method has changed. Now, there are modern techniques to help patients recover better.
What are the indications for APR surgery in rectal cancer treatment?
APR surgery is for patients with low rectal tumors. It’s when saving the sphincter isn’t an option. Choosing the right patient for this surgery is key.
What are the different variations of APR surgical procedures?
There are many APR procedures, like standard and anterior perineal resections. There’s also extralevator and ischioanal APR. The choice depends on the tumor’s location and the patient’s health.
What is involved in the preoperative assessment and patient preparation for APR surgery?
Before surgery, doctors use imaging and team reviews. They also consider neoadjuvant therapy. Teaching the patient and marking the stoma site are also important steps.
What are the technical aspects of APR surgery?
APR surgery has two parts: the abdominal and perineal phases. The team must be skilled in these techniques, including making and managing the colostomy.
References
Sauer, R., Liersch, T., Merkel, S., Fietkau, R., Hohenberger, W., Hess, C., Becker, H., Raab, H. R., Villanueva, M. T., Witzigmann, H., Wittekind, C., Beissbarth, T., & Rödel, C. (2012). Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. Journal of Clinical Oncology, 30(16), 1926–1933. https://pubmed.ncbi.nlm.nih.gov/22529259/