When a blood clot forms in an artery, it can block critical blood flow. This can lead to severe complications like heart attack or stroke. At Liv Hospital, we focus on patient-centered care. We follow international standards for diagnosing and treating blood clots in arteries.
Understanding arterial thrombosis is key for good healthcare. Symptoms like chest pain, abnormal pulsations, and heart pain can mean an arterial clot. The CDC says these symptoms could be linked to arterial clots. They provide more information in their health statistics.
Key Takeaways
- Arterial clots can cause life-threatening conditions like heart attacks and strokes.
- Understanding the symptoms is key for timely medical help.
- Liv Hospital offers top-notch care for diagnosing and treating arterial clots.
- Symptoms can include chest pain, abnormal pulsations, and heart pain.
- Good healthcare means knowing about arterial thrombosis and its effects.
What Is an Arterial Clot? Understanding the Basics
An arterial clot, also known as arterial thrombosis, is a blood clot in an artery. It can cause serious health problems. We’ll look at what arterial clots are, how they’re different from venous clots, and why they’re so dangerous.
Definition of Arterial Thrombosis
Arterial thrombosis is when a blood clot forms in an artery. This clot can block blood flow, causing damage or organ problems. It can happen for many reasons, like injury, abnormal blood flow, or clotting issues.
How Arterial Clots Differ from Venous Clots
Arterial clots are different from venous clots in many ways. Venous clots are in veins and linked to deep vein thrombosis. Arterial clots are in arteries and can cause heart attacks or strokes.
The Serious Nature of Blood Clots in Arteries
Blood clots in arteries are very serious. They can suddenly block an artery, cutting off blood to vital organs. This can lead to heart attacks or strokes, which are very dangerous.
| Characteristics | Arterial Clots | Venous Clots |
|---|---|---|
| Location | Form in arteries | Form in veins |
| Composition | Typically contain more platelets | Contain more fibrin and red blood cells |
| Clinical Implications | Can cause heart attacks, strokes | Often associated with deep vein thrombosis |
Fact 1: Arterial Clots Can Lead to Life-Threatening Conditions

Arterial clots are a big risk for heart health. They can cause heart attacks, strokes, and other serious problems. These clots can block blood flow to important organs, leading to damage or failure.
Heart Attacks: When Clots Block Coronary Arteries
A heart attack happens when a clot blocks a coronary artery. This stops blood from getting to the heart muscle. It can harm the heart tissue, leading to a heart attack. Prompt medical attention is key to reduce damage and improve chances of recovery.
Strokes: The Impact of Cerebral Arterial Clots
Arterial clots in cerebral arteries can cause strokes by blocking brain blood flow. The stroke’s severity depends on the clot’s location and size. Immediate medical help is needed to restore blood flow and prevent brain damage.
Peripheral Artery Disease and Limb Ischemia
Arterial clots can also harm peripheral arteries. This leads to peripheral artery disease (PAD) or limb ischemia. PAD causes leg pain and cramping, while limb ischemia can cause severe damage if not treated quickly. Managing risk factors and getting medical care can prevent these issues.
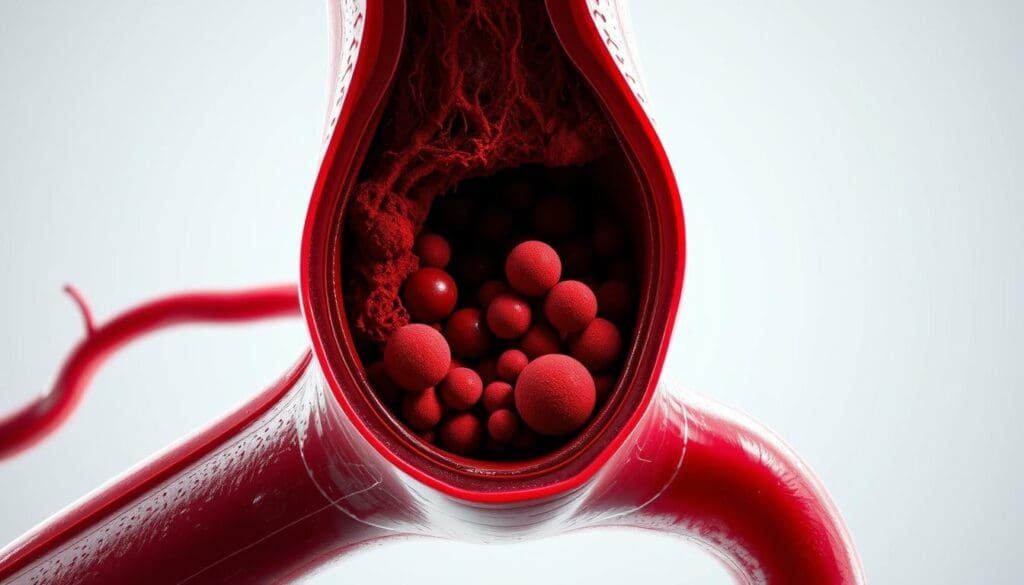
Fact 2: The Formation Process of Arterial Thrombi
The formation of arterial thrombi is a complex process. It involves many factors and pathways. Knowing this helps us understand the risks of arterial thrombosis.
The Blood Clotting Mechanism
The blood clotting mechanism stops bleeding when a blood vessel is injured. It’s a series of reactions that form a fibrin clot. Clotting factors, proteins in the blood, start this process.
When an artery is damaged, these factors are activated. This leads to the formation of a thrombus.
Role of Platelets in Arterial Clot Formation
Platelets are key in starting arterial thrombus formation. When an artery is injured, platelets stick to the injury site. They form a platelet plug.
This plug is a base for a fibrin clot to form. Activating platelets is a critical step in arterial thrombosis. It helps assemble clotting factor complexes.
How Atherosclerosis Triggers Thrombus in Artery
Atherosclerosis is a buildup of plaque in arterial walls. It’s a big risk factor for arterial thrombosis. When plaque ruptures, it exposes blood to thrombogenic material.
This triggers thrombus formation. The ruptured plaque’s surface is perfect for platelet adhesion and aggregation. This starts the clotting cascade.
| Factor | Role in Arterial Thrombosis |
|---|---|
| Platelets | Adhere to injury site, aggregate, and form a platelet plug |
| Clotting Factors | Mediate the coagulation cascade, leading to fibrin clot formation |
| Atherosclerosis | Provides a trigger for thrombosis through plaque rupture |
Understanding how arterial thrombi form is key. It shows why managing atherosclerosis and thrombosis risks is important. By tackling these risks, we can lower the chance of heart events linked to arterial thrombosis.
Fact 3: Major Causes of Arterial Thrombosis
Knowing what causes arterial thrombosis is key to preventing it. This condition happens when a blood clot blocks an artery. This can stop blood from reaching important organs. We’ll look at the main reasons why this happens.
Atherosclerosis: The Primary Culprit
Atherosclerosis is the main cause of arterial thrombosis. It’s when plaque builds up in artery walls, making them narrow and hard. If this plaque bursts, it can cause a blood clot to form.
High Blood Pressure and Diabetes Impact
High blood pressure and diabetes are big risks for arterial thrombosis. High blood pressure can harm artery walls, making them more likely to clot. Diabetes speeds up atherosclerosis and makes clotting worse.
Smoking, Age, and Family History Factors
Smoking is a big risk because it damages blood vessel linings and promotes clotting. Being older and having a family history of heart disease also raises the risk of arterial thrombosis.
High Cholesterol and Other Risk Factors
High cholesterol leads to plaque buildup in arteries, raising the risk of thrombosis. Other risks include being overweight, not being active, and certain genetic conditions that affect blood clotting.
By knowing these causes, people can take steps to lower their risk of arterial thrombosis. This can help avoid its serious effects.
Fact 4: Common Locations Where Arterial Clots Form
It’s important to know where arterial clots usually form. This helps doctors diagnose and treat health problems. Clots can form in different parts of the body, causing various heart and blood vessel issues.
Blood Clot of the Heart: Coronary Arteries
Arterial clots often form in the coronary arteries. These arteries carry blood to the heart muscle. A clot here can cause a heart attack, damaging the heart muscle and posing serious risks.
The severity of a heart attack depends on the size and location of the clot.
Cerebral Arteries: Leading to Stroke
Clots can also form in the cerebral arteries. These arteries supply blood to the brain. A clot here can lead to a stroke, causing brain damage or even death.
The impact of a stroke varies depending on the area of the brain affected.
Arterial Blood Clot in Legs: Peripheral Artery Disease
Peripheral arteries in the legs are another common site for clots. This can cause peripheral artery disease (PAD). Symptoms include leg pain when walking and can lead to serious problems if not treated.
Other Critical Locations for Arterial Thrombi
Arterial clots can also form in other important areas. This includes the aorta and renal arteries. Each location has its own risks and challenges for treatment.
Fact 5: Recognizing Symptoms of Arterial Clots
It’s important to know the signs of arterial clots to get help fast. These clots can cause different symptoms based on where they are and which organ they affect.
General Warning Signs of Artery Thrombosis
There are common signs that something might be wrong. Look out for sudden pain, numbness, or weakness in your body.
Heart Attack Symptoms from Coronary Arterial Clots
Arterial clots in the heart’s arteries can cause a heart attack. You might feel chest pain or discomfort, have trouble breathing, or feel pain in your arms, back, neck, jaw, or stomach.
| Symptom | Description |
|---|---|
| Chest Pain | Pressure, tightness, or discomfort in the chest |
| Shortness of Breath | Difficulty breathing or feeling winded |
| Arm or Jaw Pain | Pain or discomfort radiating to the arms or jaw |
Stroke Symptoms from Cerebral Arterial Clots
Clots in the brain’s arteries can lead to a stroke. Look out for sudden numbness or weakness in your face, arm, or leg. You might also feel confused, have trouble speaking, or see things differently in one or both eyes.
“Time is brain” when it comes to stroke treatment, stressing the need for quick medical help if you see these signs.
Artery Thrombosis Symptoms in Legs and Extremities
Clots in the legs can cause pain or cramping when walking. You might also feel coldness or numbness in your legs or feet. Weak or absent pulses in these areas are another sign.
Knowing these symptoms can help you get medical help fast. This could prevent serious problems.
Fact 6: Diagnosing Blocking of an Artery by a Blood Clot
Diagnosing arterial thrombotic disease needs a mix of physical checks and advanced tests. Getting the diagnosis right is key for quick treatment.
Physical Examination Techniques
A detailed physical check is the first step. Doctors look for signs like weak pulses, pale skin, and low blood pressure in the affected limb.
Imaging Tests for Arterial Thrombotic Disease
Imaging tests are vital for diagnosing this disease. Here are some tests used:
- Angiography: Gives clear images of arteries and spots blockages.
- Ultrasound: Uses sound waves to see blood flow and find clots.
- CT scans: Shows cross-sections of arteries, helping find clots’ location and size.
| Imaging Test | Purpose | Benefits |
|---|---|---|
| Angiography | Detailed imaging of arteries | Identifies blockages and clots accurately |
| Ultrasound | Visualizes blood flow | Non-invasive, quick results |
| CT scans | Cross-sectional imaging | Provides a full view of artery health |
Blood Tests and Other Diagnostic Procedures
Blood tests are key in diagnosing this disease. They check for clotting and inflammation markers, like D-dimer levels. Other tests, like electrocardiograms (ECGs), check the heart’s function.
Emergency Diagnosis Protocols
In emergencies, fast diagnosis is essential. Quick symptom checks, immediate imaging, and fast treatment are used to reduce damage.
Fact 7: Treatment Approaches for Arterial Blood Clots
Managing arterial thrombosis needs a detailed plan. Treating arterial blood clots involves emergency care and long-term strategies. These are to stop further problems.
Emergency Interventions for Acute Arterial Thrombosis
Emergency steps are key for acute arterial thrombosis. They help restore blood flow and avoid tissue damage. Thrombolytic therapy breaks down the clot. Mechanical thrombectomy removes it mechanically.
Medications for Dissolving and Preventing Clots
Medicines are vital in managing arterial blood clots. Anticoagulants stop new clots from forming. Antiplatelet agents prevent platelet clumping. Thrombolytics dissolve existing clots.
Surgical and Minimally Invasive Procedures
Surgical and minimally invasive methods are used to treat arterial blood clots. Angioplasty and stenting open blocked arteries. Surgical thrombectomy is needed in some cases.
Rehabilitation After Treatment
Rehabilitation is key after treating arterial blood clots. We create a personalized plan for each patient. It includes lifestyle changes, physical therapy, and monitoring to prevent future clots.
Fact 8: Preventing Arterial Clots and Reducing Risk
We can lower the risk of arterial thrombosis by taking proactive steps. Preventing arterial clots requires a mix of lifestyle changes, medical care, and preventive drugs.
Lifestyle Modifications to Prevent Thrombosis in Artery
Healthy lifestyle choices are key to avoiding arterial clots. Quitting smoking, keeping a healthy weight, and exercising regularly are important. Eating a diet full of fruits, veggies, and whole grains also helps.
Medical Management of Risk Factors
Managing health conditions well is vital to prevent arterial clots. This means controlling high blood pressure, managing diabetes, and treating high cholesterol. Regular doctor visits help keep these risks in check.
Preventive Medications and Monitoring
Preventive drugs might be needed for some to lower clot risk. Antiplatelet drugs and anticoagulants are often used. It’s important to have regular check-ups to adjust medications and watch for side effects.
When to Consult a Healthcare Provider
Knowing when to see a doctor is important. People with heart disease or at high risk should talk to their doctor about prevention. If you have symptoms like chest pain or sudden weakness, get help right away.
Fact 9: Long-term Outlook After an Arterial Clot
The long-term outlook after an arterial clot depends on several factors. These include the clot’s severity and how well treatment works. We’ll guide you through the recovery process and beyond.
Recovery Expectations and Timeline
Recovery from an arterial clot varies greatly among individuals. The first few weeks are critical, and patients are closely watched for complications. Recovery can take anywhere from a few weeks to several months. This depends on the person’s health and any underlying conditions.
Potential Complications and Recurrence Risks
There’s a chance of complications and clot recurrence after an arterial clot. We identify these risks and use management strategies to reduce them. Patients learn to recognize signs of complications to get timely medical help.
Follow-up Care and Ongoing Management
Regular follow-up care is key for managing long-term effects of an arterial clot. This includes regular check-ups and monitoring of risk factors. We also adjust treatment plans as needed. It’s important to stick to prescribed medications and make lifestyle changes.
Quality of Life Considerations
Improving quality of life after an arterial clot requires big lifestyle changes. We help patients create personalized plans. These plans include dietary changes, exercise, and stress management to enhance well-being.
Conclusion: Taking Action Against Arterial Clots
Understanding arterial clots is key to preventing and managing health issues. We’ve looked at the causes, symptoms, and treatments for arterial thrombosis. It’s clear that quick action is vital.
Preventing and treating arterial clots requires a mix of strategies. Managing risks like high blood pressure, diabetes, and high cholesterol helps. This can lower the chance of getting arterial clots.
Arterial thrombosis comes from many factors, like atherosclerosis, lifestyle, and genetics. Being proactive in prevention and getting medical help on time can help. This way, we can lessen the risks of arterial clots.
We urge readers to talk to healthcare experts for a plan to prevent and manage arterial clots. Together, we can lower the number of arterial thrombosis cases. This will improve our heart health overall.
What is an arterial clot?
An arterial clot, also known as arterial thrombosis, is a blood clot in an artery. It blocks blood flow to vital organs and tissues. This can lead to serious health issues.
How does an arterial clot differ from a venous clot?
Arterial clots form in arteries, carrying oxygenated blood away from the heart. Venous clots form in veins, carrying deoxygenated blood back to the heart. Arterial clots cause more immediate and severe damage because of the arteries they block.
What are the symptoms of an arterial clot in the heart?
Symptoms of a heart artery clot include chest pain or discomfort, shortness of breath, nausea, and fatigue. These are signs of a heart attack.
Can arterial clots cause a stroke?
Yes, a clot in the cerebral arteries can cause a stroke. It blocks blood flow to the brain. Symptoms include sudden weakness, confusion, difficulty speaking, and vision changes.
What are the risk factors for developing arterial thrombosis?
Risk factors include atherosclerosis, high blood pressure, diabetes, smoking, age, and family history of heart disease. High cholesterol is also a risk factor.
How is arterial thrombotic disease diagnosed?
Diagnosis involves physical exams, imaging tests like ultrasound and angiography, and blood tests. These tests check clotting factors and biomarkers. Emergency diagnosis is used to quickly treat acute cases.
What are the treatment options for arterial blood clots?
Treatments include emergency interventions like thrombolysis and medications to dissolve clots. Surgical and minimally invasive procedures like angioplasty and stenting are also used. Rehabilitation helps restore function and prevent recurrence.
How can arterial clots be prevented?
Prevention involves a healthy diet, regular exercise, quitting smoking, and managing stress. Medical management of risk factors and preventive medications are also key. Monitoring for early signs of disease is important.
What is the long-term outlook after experiencing an arterial clot?
The outlook depends on the clot’s location and severity, and the treatment’s success. Patients may need ongoing care, lifestyle changes, and medication to prevent recurrence and manage complications.
What are the common locations where arterial clots form?
Clots can form in coronary, cerebral, and peripheral arteries. This leads to heart attacks, strokes, and peripheral artery disease.
How does atherosclerosis contribute to arterial thrombosis?
Atherosclerosis, or plaque buildup in arteries, damages the inner lining. This makes arteries more prone to clot formation.
References
- World Thrombosis Day (Arterial Thrombosis) : https://www.worldthrombosisday.org/know-thrombosis/what-is-thrombosis/arterial-thrombosis
- NCBI Bookshelf (Thrombosis) : https://www.ncbi.nlm.nih.gov/books/NBK538430
- AHA Journals (Arteriosclerosis, Thrombosis, and Vascular Biology) : https://www.ahajournals.org/doi/10.1161/ATVBAHA.124.320151
- Penn Medicine (Arterial Embolism) : https://www.pennmedicine.org/conditions/arterial-embolism
- CDC (Blood Clots Facts & Stats) : https://www.cdc.gov/blood-clots/data-research/facts-stats/index.html























