Last Updated on November 17, 2025 by Ugurkan Demir

When a blood clot forms inside an artery, it can block blood flow. This can lead to serious medical events like heart attack, stroke, and peripheral arterial disease. At LivHospital, we know how important arterial thrombosis is for global health. Understand arterial thrombosis, its causes, symptoms, and how blood clots form in arteries.
We aim to give top-notch healthcare and support to international patients. Our team works hard to treat blood clots in arteries with great care and accuracy.
It’s key to understand the causes and symptoms of thrombosis in artery. This helps us treat it quickly and effectively. We’re here to help you through this process and provide the care you need.
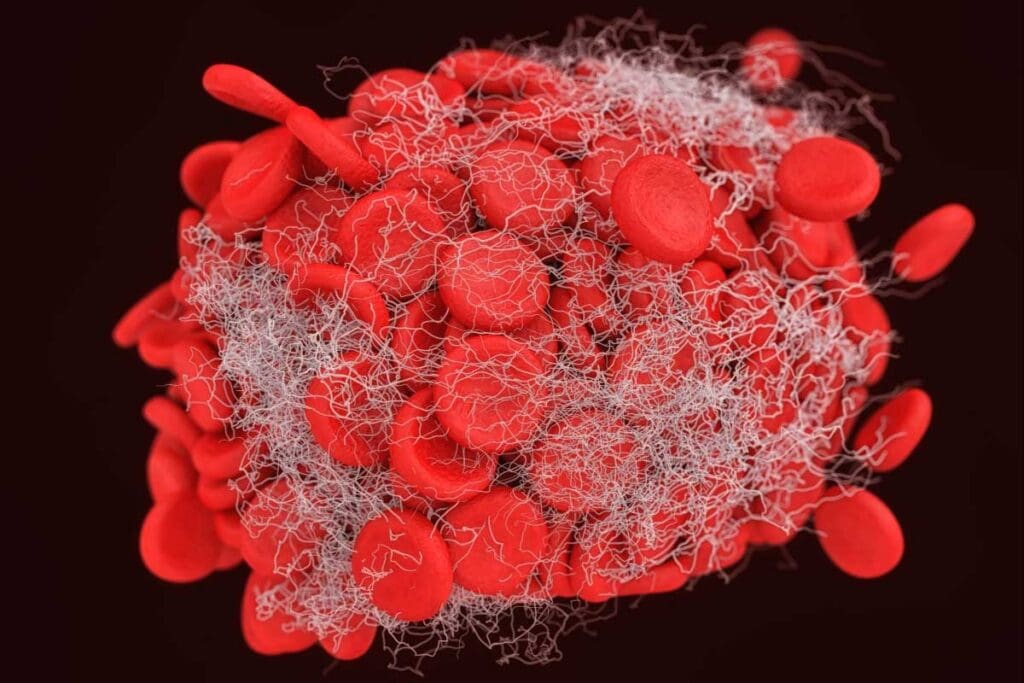
Arterial blood clots form quickly and can cause serious health problems. When a blood clot blocks an artery, it stops oxygen-rich blood from reaching important organs and tissues.
An arterial blood clot forms when an artery’s inner lining gets damaged, usually because of atherosclerosis. This damage exposes collagen and tissue factor, starting a chain of events that leads to clotting.
This process is fast, often happening in just minutes. It can cause severe symptoms to appear suddenly.
Arterial thrombi and venous clots are different in many ways. Arterial clots form in high-pressure vessels with oxygen-rich blood. Venous clots form in low-pressure veins with less oxygen.
| Characteristics | Arterial Thrombi | Venous Clots |
| Blood Flow | High pressure, oxygen-rich | Low pressure, oxygen-poor |
| Formation Speed | Rapid, often minutes | Slower, often hours or days |
| Common Causes | Atherosclerosis, injury | Stasis, hypercoagulability |
Knowing these differences is key to diagnosing and treating arterial thrombosis right.
Arterial thrombosis is a serious condition where a blood clot forms in an artery. This can block blood flow to vital organs. It’s important to know about it because it can have severe effects on the body.
When a clot forms in an artery, it can block blood flow. This blockage can damage tissue or even cause organ failure. For example, a clot in a heart artery can cause a heart attack. A clot in a brain artery can lead to a stroke.
The effects of arterial thrombosis can be severe. A clot can block the artery, stopping blood flow. This can lead to tissue death if not treated quickly.
Arterial thrombosis can happen suddenly or over time. Sudden cases have severe symptoms like pain and breathing trouble. Slow cases have milder symptoms that get worse over time.
Knowing if it’s acute or chronic helps decide how to treat it. Quick cases need fast action like clot-busting drugs or surgery. Slow cases might need ongoing treatment and lifestyle changes.
“The timely diagnosis and treatment of arterial thrombosis are critical to preventing long-term damage and improving patient outcomes.”
— Cardiologist
| Manifestation | Characteristics | Treatment Approach |
| Acute | Sudden onset, severe symptoms | Immediate medical intervention (thrombolytic therapy, surgery) |
| Chronic | Gradual onset, milder symptoms | Long-term management (anticoagulant medication, lifestyle changes) |
In conclusion, knowing about arterial thrombosis and its effects is key. Recognizing its signs can help get timely treatment. This can save lives and prevent serious health problems.
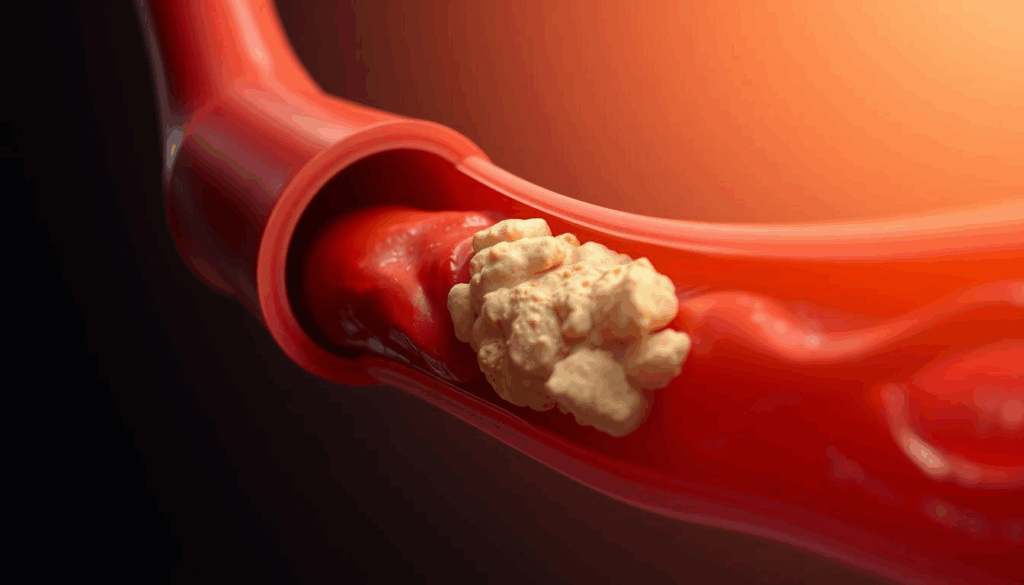
Atherosclerosis is the main cause of arterial thrombosis. It involves the buildup and rupture of plaques. These plaques are made of fat, cholesterol, and other substances.
Over time, this buildup narrows the arteries. This narrowing can lead to arterial thrombosis.
Atherosclerosis starts early in life. Plaque buildup happens when there’s an imbalance in lipid metabolism. This imbalance leads to lipids accumulating in the arterial walls.
Risk factors like hypertension, diabetes, and smoking make this worse.
As plaques grow, they narrow the arteries. This narrowing, or stenosis, reduces blood flow to vital organs. Symptoms vary based on where the artery is affected.
Plaque rupture is a key event that can cause an arterial thrombus. When a plaque ruptures, the lipid core is exposed. This triggers a quick clotting response.
This clot can block the artery. It can cause acute ischemic events like myocardial infarction or stroke.
The process of plaque rupture and clot formation is complex. It involves the plaque’s composition and inflammation. Understanding these mechanisms is key to preventing and treating arterial thrombosis.
Arterial thrombotic disease is influenced by several key risk factors. These can be divided into modifiable and non-modifiable factors. Knowing these risk factors is key to preventing and managing the disease.
Several risk factors for arterial thrombotic disease can be changed. Hypertension, or high blood pressure, damages blood vessel linings. This makes them more likely to form clots.
Diabetes also increases the risk of arterial thrombosis. It causes inflammation and damage to blood vessels. This can lead to plaque buildup and thrombosis.
Smoking is a major risk factor that damages the cardiovascular system. It also increases the risk of arterial thrombosis. Quitting smoking is a critical step in reducing this risk.
| Modifiable Risk Factor | Impact on Arterial Thrombosis |
| Hypertension | Damages blood vessel lining, increasing clot risk |
| Diabetes | Causes inflammation and vascular damage |
| Smoking | Damages cardiovascular system, increases thrombosis risk |
Some risk factors can’t be changed, but knowing them helps manage risk. Age is a significant risk factor. The risk of arterial thrombosis increases with age due to plaque buildup.
Gender also plays a role. Men are generally at higher risk at younger ages than women. But, women’s risk increases after menopause.
Genetic predisposition is another non-modifiable risk factor. People with a family history of arterial thrombotic disease are at higher risk. They should be closely monitored.
Understanding both modifiable and non-modifiable risk factors helps individuals take proactive steps. Managing modifiable risk factors through lifestyle changes and medical treatment can significantly lower risk.
It’s key to know the signs of artery thrombosis to get help fast. We’ll look at how symptoms change based on where the clot is in the body.
A blood clot in the heart’s arteries can cause a heart attack. Look out for these symptoms:
If you have these symptoms, get medical help right away. Quick action can greatly improve your chances of recovery.
A clot in the brain’s arteries can lead to a stroke. Watch for these signs:
Spotting these symptoms early and getting medical help fast can save your life.
Peripheral arterial disease (PAD) is a blockage in leg arteries. Look out for these symptoms:
Knowing these symptoms can help you get medical help quickly. This can prevent serious problems like losing a limb.
We stress the importance of recognizing these symptoms and getting medical help right away. Early treatment can greatly improve outcomes for those with artery thrombosis.
Diagnosing arterial thrombosis is a detailed process. It uses non-invasive imaging and lab tests. Accurate diagnosis is key for quick treatment and management.
Non-invasive imaging is vital for spotting arterial blood clots. Ultrasound and CT scans are top choices. They help see the arteries and find clots or blockages.
Laboratory tests are key for checking thrombosis risk and finding arterial clots. They look at blood clotting factors and find possible causes of thrombosis.
Some important tests are:
Arterial thrombosis treatment needs a mix of medical strategies. These aim to open up blocked blood flow and stop more clots. The right treatment depends on the clot’s size, location, and the patient’s health.
Antiplatelet and anticoagulant drugs are key in treating arterial thrombosis. Antiplatelet drugs like aspirin and clopidogrel stop platelets from sticking together. Anticoagulants, including warfarin and NOACs like rivaroxaban, slow down blood clotting. This reduces the chance of more clots forming.
Doctors often mix these medicines. They pick the best ones based on the patient’s risk factors and the clot’s details.
Thrombolytic therapy quickly dissolves acute clots. It uses drugs to activate the body’s clot-dissolving system. This treatment is urgent, used in emergencies like stroke or severe limb ischemia.
Sometimes, surgical or endovascular interventions are needed. Surgery might include removing the clot or bypassing the blocked area. Endovascular methods, like angioplasty and stenting, use small tools to open the artery.
| Treatment Option | Description | Indications |
| Antiplatelet Medications | Prevent platelet aggregation | Primary and secondary prevention of arterial thrombosis |
| Anticoagulant Medications | Inhibit coagulation cascade | Prevention of clot growth and recurrence |
| Thrombolytic Therapy | Dissolve acute clots | Acute ischemic stroke, severe limb ischemia |
| Surgical/Endovascular Interventions | Restore blood flow | Significant arterial occlusion, failed medical therapy |
Choosing the right treatment depends on many factors. These include the patient’s symptoms, the clot’s location and size, and any other health issues. A mix of treatments often works best to manage arterial thrombosis.
The COVID-19 pandemic has shown a link between the virus and a higher risk of arterial thrombosis. Understanding how COVID-19 affects our heart health is key. The virus can change how our blood clots, raising the risk of blood clots.
People with COVID-19 often have a higher chance of blood clotting. This is because the virus causes a strong inflammatory response. This response starts the blood clotting process, making arterial thrombosis more likely.
Why does this happen? It’s because of damaged blood vessels, more clotting factors, and less ability to break down clots. Knowing this helps us find ways to lower the risk of blood clots in COVID-19 patients.
To stop and manage blood clots in COVID-19 patients, we need a few steps. Anticoagulant therapy is used to prevent blood clots. But, we must adjust the treatment based on each patient’s risk.
| Strategy | Description | Benefits |
| Anticoagulant Therapy | Use of medications to prevent blood clot formation | Reduces risk of arterial thrombosis |
| Monitoring Coagulation Parameters | Regular assessment of blood clotting factors | Enables early detection of hypercoagulability |
| Lifestyle Modifications | Promoting healthy lifestyle choices | Supports overall cardiovascular health |
By using these methods, doctors can lower the risk of blood clots in COVID-19 patients. This helps improve their health outcomes.
Preventing arterial thrombosis is a mix of healthy living, medical care, and new ways to prevent it. Knowing and using these methods can lower your risk of artery blockages.
Keeping a healthy lifestyle is key to avoiding artery blockages. Eat a balanced diet with lots of fruits, veggies, and whole grains. Cut down on fats and cholesterol.
Also, physical activity like walking boosts heart health and lowers thrombosis risk.
Quitting smoking is also essential, as it greatly increases artery blockage risk. Staying away from secondhand smoke and keeping a healthy weight also help your arteries.
Managing medical risks is vital to prevent artery blockages. This means controlling high blood pressure with meds and lifestyle changes. It also means keeping diabetes under control and treating high cholesterol with statins.
People with heart disease or at high risk might get antiplatelet or anticoagulant medications. Regular check-ups with doctors are key to adjusting treatments.
New ways to prevent artery blockages are being researched. This includes novel anticoagulants that are safer and studying genetic factors that might increase risk.
Understanding arterial thrombosis and its prevention is key. We’ve looked into its causes, symptoms, and how to treat it. This knowledge helps people take action against it.
Knowing the risks, like atherosclerosis and smoking, helps make better choices. We stress the need to manage these risks with treatment and lifestyle changes.
At LivHospital, we offer top-notch care for those with arterial thrombosis. Our team creates custom plans for each patient. This ensures they get the best support.
Combining healthcare and personal effort is vital in fighting arterial thrombosis. Together, we can lower its occurrence and better outcomes for patients.
Arterial thrombosis is when a blood clot forms in an artery. This can block blood flow to important organs and tissues.
The main cause is atherosclerosis, where plaque builds up in arteries. Hypertension, diabetes, and smoking also increase the risk.
Arterial thrombosis happens in arteries and often leads to heart attacks or strokes. Venous thrombosis is in veins and can cause deep vein thrombosis.
Symptoms depend on where the clot is. Chest pain is common in heart attacks. Stroke symptoms can occur in the brain. Limb pain or numbness can happen in the limbs.
Doctors use ultrasound and CT scans to see clots. Blood tests check for clotting factors.
Doctors use medicines to stop clots. For big clots, they might use surgery or special procedures to open up the artery.
Yes, COVID-19 can make blood clot more easily. People with COVID-19 need careful medical care to avoid this.
Eating well, exercising, and not smoking helps. Managing blood pressure and diabetes is also key.
Atherosclerosis is the main cause. It leads to plaque buildup and can cause clots when the plaque ruptures.
Yes, age, gender, and genetics are non-modifiable risks. People with these risks need to stay alert and get regular check-ups.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!