Dealing with arteriovenous malformation brain surgery can seem scary. But, thanks to modern medicine and expert care, patients can get great results. Cerebral arteriovenous malformations (AVMs) are tricky blood vessel problems. They can lead to serious issues like bleeding and brain damage.
At Liv Hospital, we use the newest, safest ways to remove AVMs. We make sure our patients get the best care possible. Knowing all about the AVM removal process helps us avoid big problems.
Our team is dedicated to top-notch healthcare for everyone, including international patients. We’ll explain the 7 main steps of AVM removal and recovery. This will help you understand this complex medical process better.
Key Takeaways
- Understanding the risks associated with cerebral AVMs
- The importance of specialized care in AVM treatment
- Overview of the AVM removal process
- The role of advanced surgical techniques in AVM surgery
- Comprehensive support for international patients
Understanding Brain Arteriovenous Malformations (AVMs)

Brain AVMs are complex and need a deep understanding. They are vascular anomalies that can be risky if not handled right.
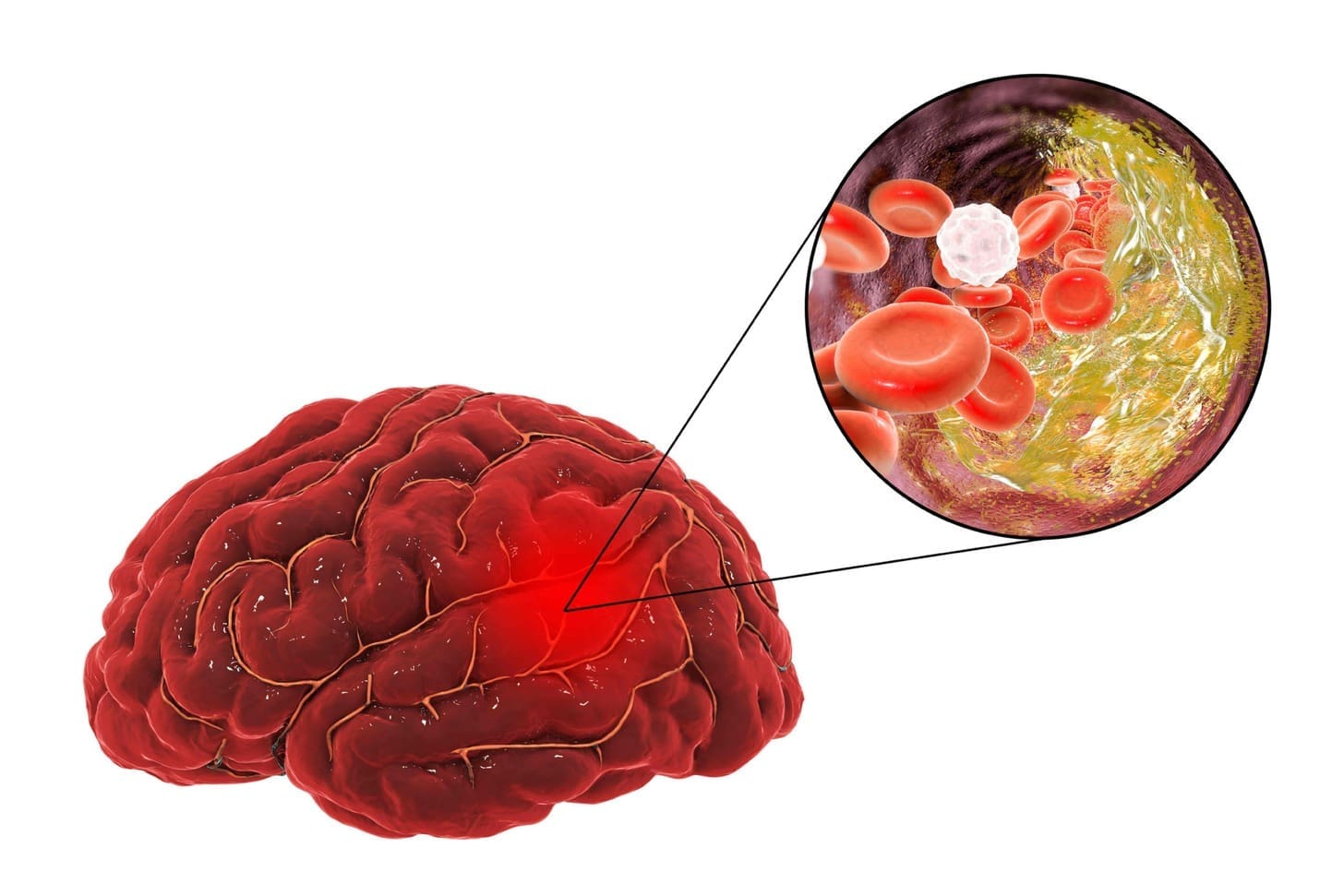
Definition and Structure of AVMs
AVMs in the brain have an abnormal link between arteries and veins. This link skips the usual capillary bed. It can cause neurological problems because of the changed blood flow and pressure.
Key characteristics of AVMs include:
- Abnormal tangles of blood vessels
- Direct connection between arteries and veins
- Absence of a normal capillary bed
- Altered hemodynamics leading to possible neurological deficits
Common Locations in the Brain
AVMs can be found in different parts of the brain. Some spots are more common than others. Knowing where they usually are helps doctors diagnose and treat them.
| Location | Frequency | Clinical Implications |
|---|---|---|
| Cerebral hemispheres | Common | May cause seizures, neurological deficits |
| Basal ganglia | Less common | Higher risk of hemorrhage |
| Brainstem | Rare, but critical | High risk of severe neurological deficits |
Prevalence and Risk Factors
AVMs in the brain are not very common, affecting about 1 in 100,000 people each year. But, some things can make it more likely to get an AVM or face complications.
Risk factors for AVMs include:
- Genetic predisposition
- Family history of vascular malformations
- Certain genetic disorders (e.g., Osler-Weber-Rendu syndrome)
Knowing these risk factors is key for catching AVMs early. This can help avoid the need for complex surgery.
Complications and Symptoms Requiring AVM Removal

Brain arteriovenous malformations (AVMs) are complex vascular anomalies. They need quick medical attention to avoid severe problems. An AVM can cause many complications, affecting a person’s quality of life.
AVMs can lead to hemorrhage, neurological deficits, and seizures. Knowing these risks helps find the best treatment.
Hemorrhage and Bleeding Risks
Hemorrhage is a severe complication of AVMs. The risk of hemorrhage from AVMs is between 2% to 4% each year. Half of these cases start with bleeding. This can cause severe brain damage, disability, or even death.
Things that raise the risk of hemorrhage include:
- Previous history of hemorrhage
- Location of the AVM in deep or critical brain areas
- High-pressure blood flow through the AVM
- Associated aneurysms
Neurological Deficits and Symptoms
AVMs can also cause neurological deficits and symptoms. This is because of abnormal blood flow and pressure on brain tissue. Common symptoms include:
- Headaches
- Seizures
- Weakness or numbness in parts of the body
- Vision problems
- Cognitive difficulties
These symptoms can greatly affect daily life and well-being. This shows the need for quick medical help.
Seizures and Cognitive Impacts
Seizures are a complication of AVMs, happening in about 20-40% of patients. The risk is higher in certain areas like the frontal or temporal lobes. Cognitive impacts, like memory and concentration problems, can also happen. Managing AVMs well is key to prevent these issues and improve outcomes.
Having an AVM can be scary, but with the right treatment, many people see big improvements. Surgery to remove the AVM is often recommended. It helps avoid future problems and improve quality of life.
Modern Arteriovenous Malformation Brain Surgery Techniques
Modern brain surgery for arteriovenous malformations (AVMs) has made big strides. Now, we have many ways to treat AVMs effectively.
Open Surgical Resection
Open surgical resection is a tried and true method for treating AVMs. It involves removing the malformation from the brain. Microsurgical techniques have made this procedure more precise, leading to better results.
Choosing open surgery depends on the AVM’s size, location, and the patient’s health. Our team carefully considers each case to find the best treatment.
Stereotactic Radiosurgery
Stereotactic radiosurgery is a non-invasive treatment that uses precise radiation to target and obliterate the AVM. It’s great for AVMs that are hard to reach surgically or are in sensitive brain areas.
Stereotactic radiosurgery is very accurate, reducing damage to healthy brain tissue. We use advanced imaging to ensure the AVM is targeted precisely.
Endovascular Embolization
Endovascular embolization is a minimally invasive procedure that blocks blood flow to the AVM using embolic materials. It can be used alone or with other treatments.
The use of Onyx, a liquid embolic agent, has made endovascular embolization more effective. Our specialists help decide if this treatment is right for each patient.
Combined Multimodal Approaches
Often, a combined approach is the best way to treat AVMs. This might include open surgery, stereotactic radiosurgery, and endovascular embolization.
Our team creates personalized treatment plans for each patient. By combining different techniques, we can get better results and lower the risk of complications.
Step 1: Comprehensive Diagnostic Evaluation
We start by doing a detailed check-up to plan how to remove the AVM. This step is key to getting the best results. It includes many tests to understand the AVM and how it affects the brain.
Advanced Neuroimaging Protocols
We use top-notch imaging to see the AVM clearly. These include:
- Digital Subtraction Angiography (DSA): Shows the blood vessels and the AVM’s details.
- Magnetic Resonance Imaging (MRI): Gives us clear pictures of the brain and the AVM.
- Computed Tomography Angiography (CTA): Uses CT scans and dye to see the blood vessels.
Cerebral Angiography and Flow Studies
Cerebral angiography is a big part of our check-up. It tells us about the AVM’s blood flow. This involves:
- Catheter Angiography: A catheter is used to inject dye and see the AVM’s blood vessels.
- Flow Studies: Look at how blood moves through the AVM.
This info is key to choosing the right treatment and knowing the risks.
AVM Grading and Risk Stratification
After we get all the info, we grade the AVM. This helps us understand the risks and decide on treatment.
The Spetzler-Martin grading system is often used. It looks at the AVM’s size, location, and how it drains blood. This helps predict surgery risks.
By using advanced imaging, angiography, and grading, we make a treatment plan that fits each patient’s needs.
Step 2: Pre-Surgical Planning and Preparation
Pre-surgical planning is key for AVM patients to get the best results. It involves getting the patient ready for surgery, reducing risks, and planning the surgical team’s strategy.
Multidisciplinary Team Assessment
A team of experts is needed for pre-surgical planning. This team includes neurosurgeons, neuroradiologists, and neurologists. They work together to figure out the best treatment plan. The team’s knowledge helps spot risks and plan how to avoid them.
Pre-Surgical Embolization Benefits
Pre-surgical embolization lowers the risk of bleeding during AVM surgery. It blocks or reduces blood flow to the AVM. This makes the surgery safer and easier.
Patient Optimization and Counseling
Getting the patient ready for surgery is important. This means checking their health, managing any conditions, and talking about their worries. This helps lower the risk of problems and improves surgery results.
Good planning and preparation are essential for AVM surgery success. By working together and being thorough, we can give patients the best care and help them recover well.
Step 3: The AVM Operation Procedure
The surgery to remove an arteriovenous malformation (AVM) is a detailed process. It requires careful planning and precise steps to ensure the best results for patients.
Anesthesia and Neurophysiological Monitoring
Anesthesia and neurophysiological monitoring are key during AVM surgery. Advanced anesthesia keeps patients comfortable and safe. Neurophysiological monitoring checks the brain’s function in real-time, allowing for quick adjustments.
“The use of neurophysiological monitoring in AVM surgery has greatly helped in preserving brain function,” says a leading neurosurgeon.
Craniotomy and Brain Access Techniques
A craniotomy is done to reach the AVM. This involves removing a part of the skull to expose the brain area around the malformation. We use precise techniques to avoid damaging nearby brain tissue.
AVM Isolation and Tissue Preservation Strategies
After gaining access, we isolate the AVM from the surrounding brain. This requires careful dissection and the use of advanced tools to save as much healthy tissue as possible. Tissue preservation strategies are key to keeping brain function after surgery.
Intraoperative Imaging and Navigation
Intraoperative imaging techniques, like angiography, are used during the surgery. They help us see the AVM’s structure and ensure it’s fully removed. Navigation systems help us stay precise in the brain, making the surgery safer and more effective.
By using these advanced methods, we can greatly improve AVM surgery outcomes. This gives patients the best chance of recovery and returning to their normal lives.
Step 4: Immediate Post-Operative Management
The post-operative phase after AVM surgery is key for the best patient results. We focus on a detailed care plan. This includes watching over patients closely, managing risks, and starting them on early movement.
Neurocritical Care Monitoring
Watching over patients closely is vital. We keep them in a special unit for neurocritical care. Here, we use advanced tools to check their brain and blood flow. This helps us catch any issues fast and act quickly.
Managing Possible Complications
It’s important to watch for and handle any problems that might come up. We look out for bleeding, swelling, or other issues. Quick action is key to avoiding lasting brain damage.
Early Mobilization Protocols
Moving patients early is a big part of getting them better. We start them off slow but keep pushing them to move more. This helps them get stronger and move better, and it also lowers the chance of other problems.
| Aspect of Care | Description | Benefits |
|---|---|---|
| Neurocritical Care Monitoring | Close monitoring in a dedicated neurocritical care unit | Early detection of complications, prompt intervention |
| Managing Possible Complications | Vigilance for signs of hemorrhage, vasospasm, or cerebral edema | Prevention of long-term neurological damage |
| Early Mobilization Protocols | Gentle, progressive mobilization to regain strength and mobility | Reduced risk of complications, improved recovery |
We think a detailed plan for after surgery is critical for the best results. By keeping a close eye on patients, managing risks, and starting them on early movement, we aim for the best recovery for our patients.
Step 5: Hospital Discharge and Early Recovery
When patients are ready to leave the hospital after AVM surgery, knowing the discharge criteria and early recovery steps is key. Leaving the hospital is a big step towards getting better. But, it needs careful planning and following doctor’s advice.
Discharge Criteria After AVM Surgery
We check if patients meet certain criteria before they go home. These include being stable neurologically, managing pain well, and doing daily tasks. Our team looks at each patient’s health, wound healing, and any complications.
| Discharge Criteria | Description |
|---|---|
| Stable Neurological Function | Patient shows no significant neurological deterioration or improvement that could impact discharge. |
| Adequate Pain Management | Pain is controlled with oral medications, and the patient understands pain management strategies. |
| Ability to Perform Daily Activities | Patient can carry out basic self-care and daily tasks with or without assistance. |
Medication Management
Managing medications well is key in early recovery. We give patients a detailed plan for their meds, including how much, how often, and possible side effects. Sticking to this plan helps healing and avoids complications.
Warning Signs and When to Seek Help
It’s important to know warning signs of complications in early recovery. These include severe headaches, sudden changes in the brain, fever, or infection signs at the surgery site. We teach patients and their caregivers about these signs and when to get help fast.
Understanding discharge criteria, managing meds well, and knowing warning signs helps patients feel confident in early recovery. Our team is here to help with any questions and support during recovery.
Steps 6-7: Long-Term Recovery and Follow-Up Protocol
Understanding long-term recovery and follow-up after AVM treatment is key. It ensures the best results for patients. This approach covers all aspects of recovery.
Rehabilitation and Therapy Options
Rehabilitation is vital after AVM surgery. We offer physical, occupational, and speech therapy. Each therapy is customized for the patient’s needs.
These therapies help patients regain strength and improve cognitive function. They also work towards achieving independence.
Follow-Up Imaging Schedule
Regular imaging checks are essential. They help monitor for AVM recurrence and track brain healing. We use MRI or angiography, depending on the case.
Neurological Assessment Timeline
Neurological assessments are done at set intervals. They check the patient’s neurological status and catch any issues early. The schedule is based on the patient’s condition and AVM complexity.
AVM Recurrence Monitoring
Watching for AVM recurrence is ongoing. We teach patients about signs and symptoms. We also tell them when to seek medical help right away.
Following this structured recovery and follow-up plan boosts patient outcomes. It also lowers the risk of complications.
Conclusion: Success Rates and Future of AVM Treatment
Advances in arteriovenous malformation (AVM) treatment have greatly improved success rates. High rates of complete obliteration are now possible through combined approaches. This shift focuses on complete care and a team effort.
The future of AVM treatment is bright, with new research and technologies on the horizon. This means better surgery outcomes and a better quality of life for patients. It’s key to choose a top hospital for AVM treatment that offers various options and skilled specialists.
At our institution, we’re dedicated to top-notch healthcare for international patients. Our team aims for the best AVM treatment success rates and a brighter future for AVM treatment. Together, we ensure patients get the best care and outcomes.
What is an arteriovenous malformation (AVM) in the brain?
An arteriovenous malformation (AVM) is a brain issue. It happens when arteries and veins connect in a way they shouldn’t. This skips the usual capillary network.
What are the risks associated with having a brain AVM?
Having a brain AVM can cause serious problems. These include bleeding, brain damage, and seizures. It’s very important to treat it to avoid these risks.
What are the modern techniques used for arteriovenous malformation brain surgery?
Today, there are many ways to treat AVMs. These include open surgery, radiosurgery, and endovascular embolization. Each method is chosen based on the patient’s needs.
How is an AVM diagnosed and evaluated before surgery?
Doctors use special imaging and tests to find out about an AVM. They look at the AVM’s size and location. This helps decide the best treatment.
What is the role of pre-surgical embolization in AVM removal?
Pre-surgical embolization helps make surgery safer. It reduces blood flow to the AVM. This makes it easier to remove without bleeding.
What are the key steps involved in the AVM operation procedure?
The surgery starts with anesthesia and a craniotomy. Then, the AVM is isolated and removed. The whole process is carefully planned and done.
What is the importance of neurocritical care monitoring after AVM surgery?
Watching over patients after surgery is very important. It helps manage any problems and keeps the brain safe. This ensures the best recovery.
What are the discharge criteria after AVM surgery, and what is the early recovery process like?
Patients are ready to go home when they’re stable and can do daily tasks. Early recovery includes managing medicine and watching for signs of trouble.
What rehabilitation and therapy options are available after AVM surgery?
There are many therapies to help patients recover. These include physical, occupational, and speech therapy. They help with any brain problems.
How is AVM recurrence monitored after treatment?
Doctors keep an eye on patients with regular check-ups and tests. This helps catch any problems early and treat them right away.
What is the current state of AVM treatment, and what are the future directions?
AVM treatment has gotten much better. There are more options now. Future improvements will focus on making surgery and treatments even better.
How can I find the best hospital for AVM treatment?
Look for a hospital with lots of experience with AVMs. Make sure the doctors are experts and the hospital offers the latest treatments.
What is the recovery process like after an AVM rupture?
After an AVM rupture, patients need quick medical help. Then, they get a treatment plan that might include surgery and therapy. They also need ongoing care to manage any issues.






















