Last Updated on November 25, 2025 by Ugurkan Demir

Discover artherosclerotic calcification causes, risks, and its role in heart and artery disease.
Atherosclerotic calcification is when calcium builds up in the artery walls. It’s often linked to atherosclerosis. This is a disease where cholesterol, fats, and other substances build up in the arteries.
At Liv Hospital, we know how important it is to find and manage this condition. The amount of calcium in arteries shows how bad coronary artery disease is. It also tells us if someone might have heart problems in the future.
Knowing about atherosclerotic calcification helps keep our hearts healthy. We use the newest tests to find this problem early. This way, we can stop heart problems before they start.
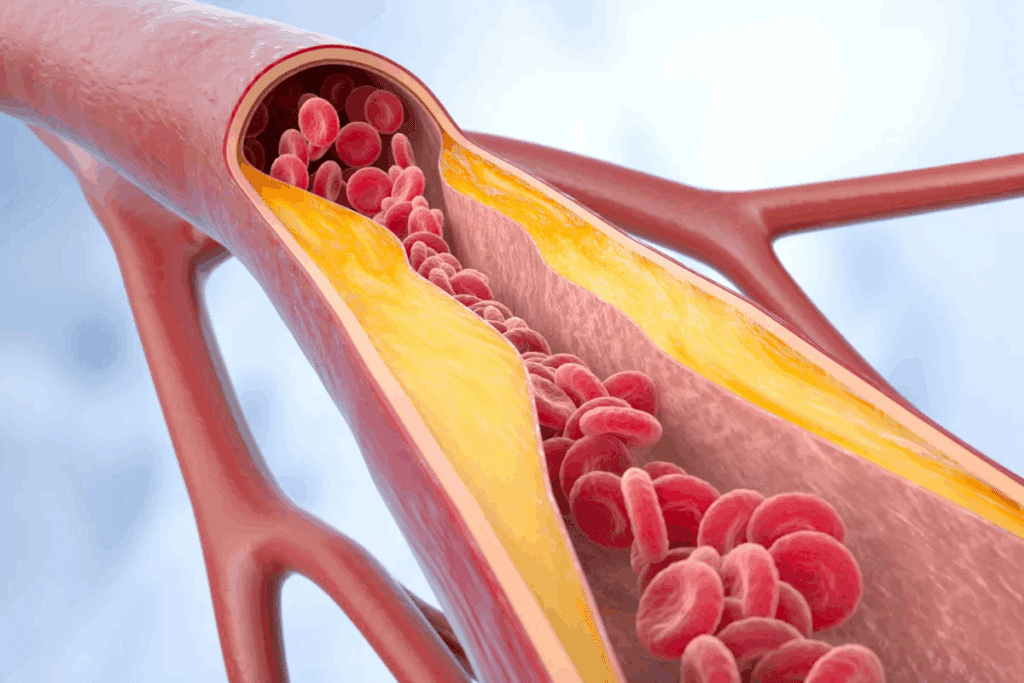
Atherosclerotic calcification is when calcium builds up in the artery walls. It’s a key sign of atherosclerosis. This buildup is not just random calcium; it’s a complex process involving cells and molecules.
Calcification happens when calcium phosphate forms in artery walls, often with atherosclerotic plaques. It’s a common part of atherosclerosis, a disease where plaque builds up in arteries. Doctors use CT scans to see how much calcium is in the coronary arteries.
| Age Group | Prevalence of Calcification |
| 40-49 years | Moderate |
| 50-59 years | High |
| 60+ years | Very High |
The table shows that calcification gets more common with age, really taking off after 40. By age 60, almost everyone has it, showing a clear link between age and calcification.
Atherosclerotic calcification is different from normal calcium buildup. Normal calcification is more controlled, but this type is linked to inflammation and plaque formation. This can cause serious heart problems.
Also, atherosclerotic calcification is a complex process, like bone formation. It’s not like normal calcium buildup, which is simpler.
Atherosclerotic calcification starts with plaque forming in the arterial intima. This process involves many cellular and molecular steps.
The journey to atherosclerotic calcification begins with endothelial dysfunction. This is when the inner lining of blood vessels gets damaged. This damage lets lipids get in and build up.
This buildup causes inflammation, drawing immune cells to the area. As it goes on, smooth muscle cells in the arterial wall get active. They help form a fibrous cap around the lipid core.
Over time, these smooth muscle cells start to act like bone-forming cells. They start depositing calcium, leading to calcification.
The calcification process is complex, involving many cellular and molecular mechanisms. Important players include inflammatory cytokines, growth factors, and signaling pathways. These regulate genes involved in calcification.
The Wnt/β-catenin signaling pathway is key in making vascular smooth muscle cells act like bone cells. Also, matrix vesicles in the arterial wall help start calcium deposition.
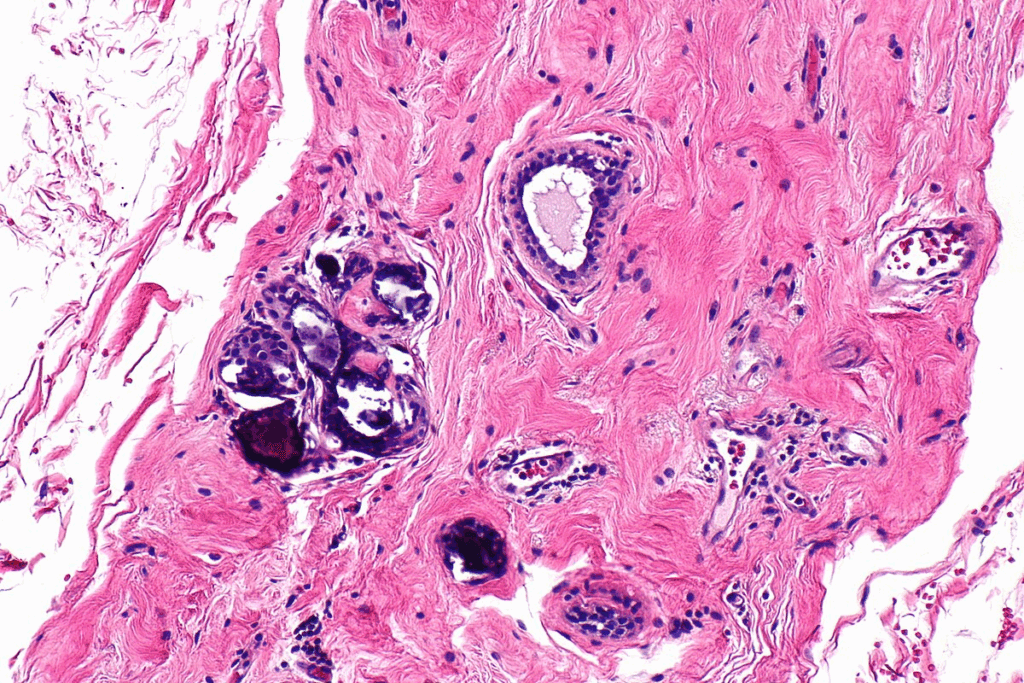
It’s important to know about the different types of arterial calcification. This knowledge helps doctors diagnose and treat heart diseases better. Arterial calcification is not the same for everyone. It comes in different types and stages, each affecting health in its own way.
Arterial calcification falls into two main categories: intimal and medial. Each has its own reasons and effects on health.
The growth of arterial calcification from tiny deposits to large calcifications is complex. It involves many cellular and molecular steps.
| Stage | Characteristics | Clinical Implications |
| Microscopic Deposits | Initial calcium and phosphate buildup | Early sign of calcification |
| Early Macroscopic Calcification | Calcification is visible on scans | Higher risk of heart problems |
| Advanced Macroscopic Calcification | Big calcification affecting artery function | Big risk of heart disease and death |
As atheromatous calcifications and arteriosclerotic calcificationsget worse, they can cause a lot of heart problems. Knowing about these processes is key to finding good ways to prevent and treat them.
Finding atherosclerotic calcification is key to knowing your heart health. This condition shows up as plaque in the arteries, which can lead to heart problems. We’ll look at how to spot it and what it means.
Several ways are used to find atherosclerotic calcification. The most common is the computed tomography (CT) scan. This includes noncontrast, electrocardiographic (ECG)-gated cardiac electron beam computed tomography (EBCT) or multislice detector computed tomography (MDCT). These scans show calcium in the heart’s arteries clearly.
Table: Comparison of Imaging Techniques for Detecting Atherosclerotic Calcification
| Imaging Technique | Description | Advantages |
| EBCT | Uses electron beam technology to image the heart | High sensitivity for detecting coronary artery calcium |
| MDCT | Multislice detector CT for detailed heart imaging | High resolution, widely available |
The Coronary Artery Calcium (CAC) score shows how much calcium is in the heart’s arteries. It’s from CT scans and predicts heart risk. A higher score means more calcium and a higher risk of heart attack and stroke.
A leading cardiology expert says,
“The CAC score is a powerful tool in the assessment of cardiovascular risk, providing a direct measure of atherosclerotic plaque burden.”
The CAC score has different risk levels. Knowing these helps doctors and patients decide on prevention and treatment.
Table: CAC Score Categories and Associated Risk
| CAC Score | Risk Category |
| 0 | Very Low Risk |
| 1-100 | Mild Risk |
| 101-400 | Moderate Risk |
| >400 | High Risk |
Knowing the risk factors for atherosclerotic calcification is key. It helps spot people at high risk and take steps to prevent it. This condition is a big sign of heart disease risk. It’s caused by many factors, some we can change and some we can’t.
Getting older increases the risk of atherosclerotic calcification. As we age, calcium builds up in our arteries. Studies show that more people get coronary artery calcium (CAC) as they get older. Men start seeing more CAC after 45, and women after 55.
Men are generally at higher risk than women, but the gap closes with age. After menopause, women’s risk goes up due to hormonal changes.
Lifestyle choices play a big role in atherosclerotic calcification risk. Smoking harms blood vessels and speeds up plaque buildup. Eating too much saturated fat, cholesterol, and sodium also increases risk. On the other hand, eating fruits, veggies, and whole grains can help.
Being inactive also raises the risk. Exercise keeps blood vessels healthy and the heart strong.
A recent study emphasizes the need for lifestyle changes:
“Lifestyle changes, including dietary modifications and increased physical activity, can significantly reduce the risk of cardiovascular events in individuals with atherosclerotic calcification.”
Some medical conditions speed up atherosclerotic calcification. Diabetes and hypertension damage blood vessels and cause inflammation. Dyslipidemia, or abnormal blood lipids, also contributes. Plus, conditions that cause hyperphosphatemia, like chronic kidney disease, raise vascular calcification risk.
Having these conditions highlights the need to manage them well. This can lower the risk of atherosclerotic calcification. Healthcare providers can use this knowledge to create plans to prevent or slow this condition.
It’s key to understand the importance of atheromatous calcification in heart health. This condition is more than just a sign of aging or heart disease. It’s a clear warning of heart risk.
Calcified atherosclerosis is linked to a higher chance of heart problems. Research shows that the more calcium in the heart’s arteries, the higher the risk of heart attacks, strokes, and death from heart disease.
“The coronary artery calcium score is a powerful predictor of cardiovascular events, providing prognostic information beyond traditional risk factors.” This shows why checking for CAC is vital in doctors’ offices. It helps doctors know who’s at higher risk.
Atheromatous calcification shows atherosclerosis and harms arterial function. It makes arteries stiff, which hurts their ability to adjust to the heart’s pulse. This stiffness raises blood pressure and puts more stress on the heart.
In summary, atherosclerotic calcification is a big deal for heart health. It affects heart event risk and arterial function. Knowing its importance helps doctors manage heart risk better and tailor care for each patient.
To prevent atherosclerotic calcification, it’s important to adopt heart-healthy habits. Managing risk factors well is key. Making smart lifestyle choices can greatly lower your risk of getting this condition.
Eating a diet full of fruits, vegetables, whole grains, and lean proteins is good. Adding foods rich in omega-3s, like salmon and walnuts, is also beneficial. It’s important to cut down on saturated fats, trans fats, and cholesterol. Also, watch your sodium intake to avoid high blood pressure, a risk factor.
Regular exercise is vital in preventing atherosclerotic calcification. Do at least 150 minutes of moderate aerobic exercise, or 75 minutes of vigorous aerobic exercise, or a mix of both, each week. Adding strength training can also boost your heart health.
For some, just lifestyle changes might not be enough. Statins, which lower cholesterol, might be prescribed. Medications for high blood pressure and diabetes can also help. Always talk to a doctor before starting any new medication or supplement.
By using these prevention strategies together, you can lower your risk of atherosclerotic calcification. This helps keep your heart healthy.
Managing atherosclerotic calcification needs a full plan. This includes current treatments, procedures, and new therapies. Knowing the early signs and tackling risk factors helps keep arteries healthy and lowers heart disease risk.
Statins are key in preventing and managing arterial calcification. They slow atherosclerosis growth, though their direct impact on calcification is being studied. We also use other drugs for high blood pressure and high cholesterol as part of a complete plan.
Statins help control cholesterol and improve plaque stability. But their role in reducing or reversing calcification is an area of ongoing research.
| Medication | Primary Use | Effect on Calcification |
| Statins | Cholesterol management | May slow progression |
| Antihypertensives | Blood pressure control | Indirectly beneficial |
| Phosphorus binders | Managing hyperphosphatemia | Directly reduces calcification risk |
For severe calcified atherosclerotic disease, we may need to use interventional procedures. These include angioplasty, stenting, or surgery to improve blood flow through blocked arteries.
New technologies are being developed to better handle calcified lesions. For example, atherectomy devices can remove plaque.
Research on reversing atherosclerotic calcifications is ongoing. It’s looking into the molecular mechanisms. New targets include calcium metabolism and inflammation pathways.
New therapies might help manage calcification better. This could reduce the heart disease burden. We keep up with research to offer the best treatments to our patients.
Understanding current and new treatments helps us manage calcified atherosclerotic disease better. This improves patient outcomes.
We are learning more about atherosclerotic calcification and its link to heart health. This condition, marked by calcified plaques, affects blood flow and heart function. It’s key to managing it well.
Research is uncovering the details of arterial calcification. It’s showing how it leads to heart problems. Knowing this helps us find better ways to prevent and treat it.
With new studies, we can improve how we handle atherosclerotic calcification. This will help patients and lower heart disease risks. As we learn more, we’ll be able to care for those with this condition better.
Atherosclerotic calcification is when calcium builds up in the arteries. This happens because of atherosclerosis, a condition where plaque forms in artery walls. It can make arteries hard and affect their function, leading to heart problems.
Unlike normal calcium, atherosclerotic calcification happens in the artery walls. It’s linked to inflammation and plaque. It’s a complex process involving many cells and molecules.
The CAC score measures calcium in the coronary arteries. It’s found through CT scans. A high score means more calcium and a higher risk of heart problems.
Risk factors include age, gender, and lifestyle choices like smoking and diet. Medical conditions like high blood pressure and diabetes also play a role. Knowing these risks helps prevent and manage the condition.
Yes, prevention is possible. Eating right, exercising, and managing health conditions are key. Some supplements may help, but always talk to a doctor first.
Treatment includes managing risk factors and slowing disease growth. For severe cases, procedures like angioplasty and stenting are used. New treatments and ways to reverse calcification are being researched.
It increases the risk of heart attacks and strokes. It can also lead to poor blood flow and ischemia. This affects heart health significantly.
Intimal calcification happens in the inner artery layer and is linked to plaque. Medial calcification affects the middle layer and isn’t always related to plaque. Both can harm arteries, but in different ways.
Yes, new treatments and strategies are being explored. This includes finding ways to reverse calcification and new procedures. Keeping up with research is important for both doctors and patients.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!