Last Updated on November 27, 2025 by Bilal Hasdemir
In the United States, over 120,000 people are waiting for a heart transplant. Sadly, many won’t get a new heart in time. That’s where robotic heart technology comes in, giving hope to those in need.
We’re on the edge of a big change in heart care, thanks to artificial heart tech. These new devices help or replace a failing heart. They offer a lifeline until a transplant is possible or even a permanent fix.
The journey of artificial hearts is filled with innovation and hard work. From the first experiments to today’s advanced devices, it’s been a long path.
In the 1980s, Robert Jarvik created the Jarvik-7, a major breakthrough in artificial hearts. It was a big step forward, helping patients wait for heart transplants.
The Jarvik-7 was a total artificial heart (TAH). It replaced the heart’s ventricles. This marked the start of a new chapter in heart therapy.
Artificial heart tech has grown a lot over the years. Better materials, designs, and electronics have made devices more reliable and easier for patients.
| Decade | Advancements | Notable Devices |
| 1980s | Introduction of the first artificial hearts | Jarvik-7 |
| 1990s | Improvements in durability and battery life | HeartMate I |
| 2000s | Advances in miniaturization and control systems | HeartMate II |
| 2010s | Development of continuous-flow devices and wireless technology | HeartMate 3, Carmat TAH |
The journey of artificial hearts has seen big tech leaps. These advancements have greatly improved patient lives. We can look forward to even more advanced devices as research continues.
An artificial heart is a medical device that helps a failing heart. It gives patients with severe heart problems a second chance. This device is a big step forward in treating heart failure, helping those waiting for a transplant or not eligible for one.
An artificial heart, or mechanical heart, works like a real heart. It has a pump, valves, and a power source. The pump moves blood, the valves keep it flowing right, and the power source runs the pump.
The parts work together to support or replace the heart’s function. Thanks to technology, these hearts are getting better, lasting longer, and working better.
Artificial hearts are made to act like a real heart, but they’re different. They need a power source, which can make moving harder. They also face issues like infections and breakdowns.
Even with these challenges, artificial hearts are a key option for severe heart failure. New tech is making these hearts better, aiming for better results for patients.
Artificial hearts come in different types to meet various patient needs. They are developed to tackle the complex nature of heart failure. We’ll look at Total Artificial Hearts (TAHs), Ventricular Assist Devices (VADs), and Biventricular Assist Devices (BiVADs).
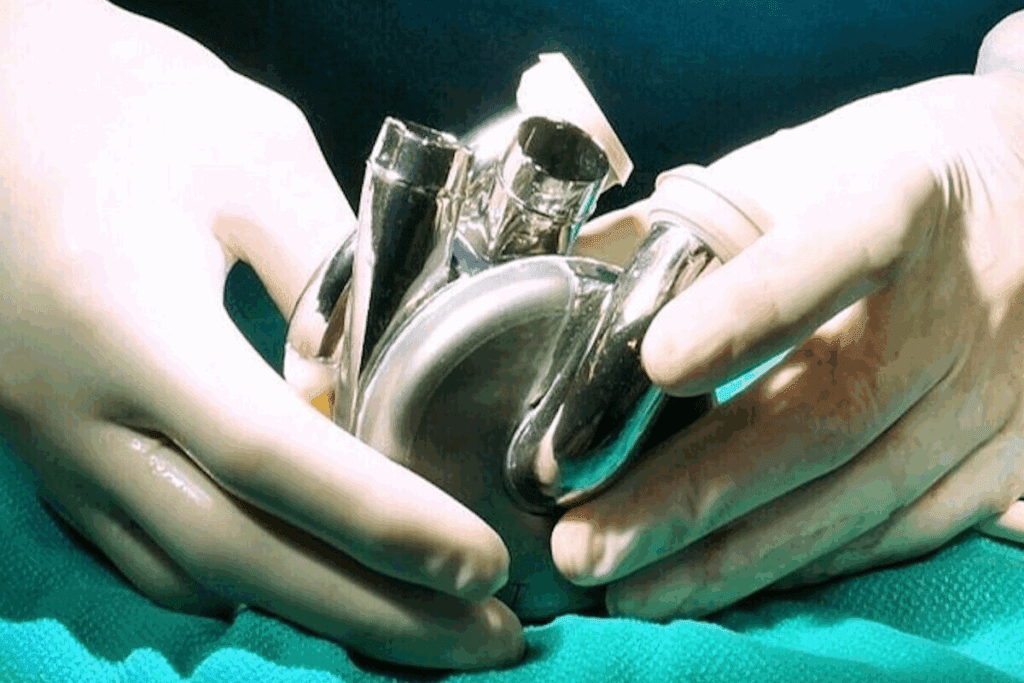
Total Artificial Hearts replace the whole heart, including both ventricles and atria. They’re for patients with severe heart failure who can’t get a transplant or are waiting. The SynCardia Total Artificial Heart is a well-known model. It’s been used for decades and works by being pneumatically driven.
Ventricular Assist Devices are pumps that help the ventricles pump blood better. They’re for patients with left, right, or both ventricular failures. Left Ventricular Assist Devices (LVADs) are the most common, supporting the left ventricle.
They’re often used in patients waiting for a transplant or as a long-term solution for those not eligible for a transplant.
Biventricular Assist Devices support both the left and right ventricles. They’re for patients with biventricular failure, where both sides of the heart aren’t working well. These devices are key for patients needing full cardiac support.
By helping both ventricles, BiVADs ensure proper blood flow. They’re a vital step towards heart transplantation.
Each artificial heart type has its own use, benefits, and challenges. The right device depends on the patient’s heart condition and other factors. As technology improves, we’ll see more advanced artificial hearts.
The field of artificial hearts is growing fast. Many models are being made by key players. These devices are getting better, giving hope to those needing heart replacements.
The SynCardia Total Artificial Heart is a well-known device for patients waiting for a transplant. It replaces the heart’s main parts, acting as a temporary fix until a donor heart is found.
Key Features of SynCardia Total Artificial Heart:
The Abbott HeartMate3 Left Ventricular Assist Device (LVAD) is a big step forward. It helps patients with severe heart failure by supporting the heart’s pumping action.
Advantages of Abbott HeartMate3 LVAD:
Here’s a comparison of the SynCardia Total Artificial Heart and Abbott HeartMate3 LVAD:
| Feature | SynCardia Total Artificial Heart | Abbott HeartMate3 LVAD |
| Device Type | Total Artificial Heart | Left Ventricular Assist Device |
| Primary Use | Bridge to transplantation | Bridge to transplantation or destination therapy |
| Key Technology | Pneumatic pumping | Magnetic levitation |
The CARMAT Total Artificial Heart is a new type of artificial heart. It uses biomimetic materials and a unique self-regulation system. It aims to work like a real heart more closely than before.
Innovative Features of CARMAT Total Artificial Heart:
These leading artificial heart models show the fast progress in cardiac replacement therapy. As technology keeps improving, we can look forward to better devices and outcomes for patients.
It’s important to understand how robotic hearts work. They are advanced medical devices designed to help patients with severe heart failure. These devices can replace or support the natural heart’s function.
Robotic hearts use advanced engineering to mimic the heart’s natural pumping action. They have sensors and control systems to monitor and adjust the pumping. This ensures the body gets the blood it needs efficiently.
There are different types of robotic hearts, like Total Artificial Hearts (TAHs) and Ventricular Assist Devices (VADs). Each type is used based on the patient’s condition and how severe their heart failure is.
The power sources for robotic hearts are key to their design. They affect how independent and mobile the patient can be. Most are powered by batteries that patients wear, allowing for freedom of movement.
The energy needs of robotic hearts vary. New technologies have made them more energy-efficient. This means smaller power sources and better comfort for patients. Researchers are also looking into wireless charging to make these devices even more convenient and safe.
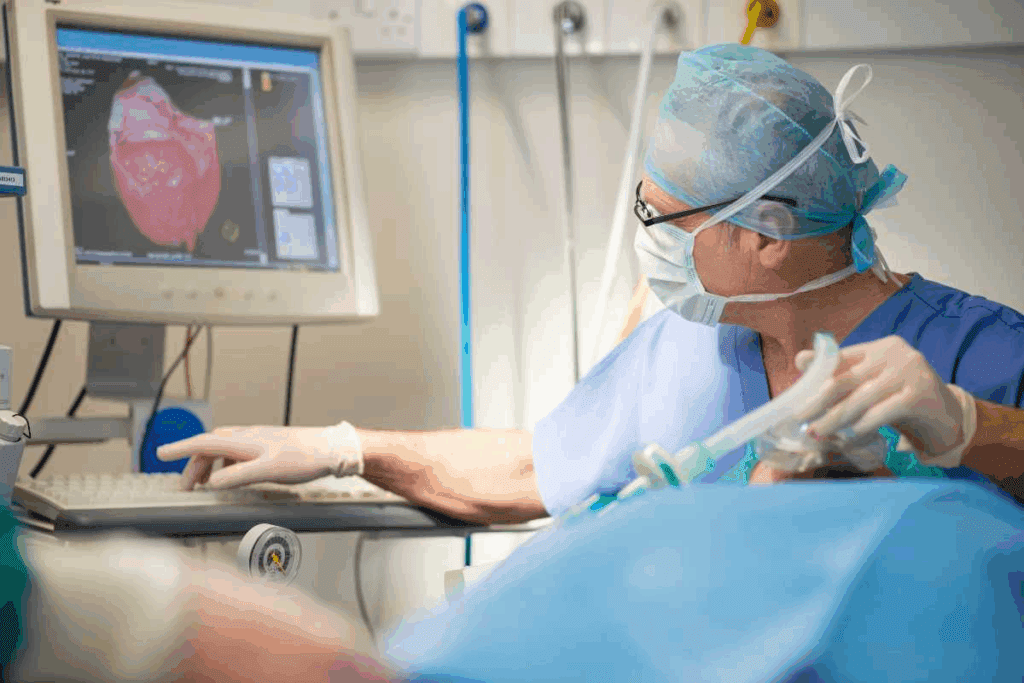
Putting in an artificial heart is a complex surgery that has gotten better over time. It needs a team of experts, like heart surgeons, anesthesiologists, and perfusionists. They work together to help patients get better.
Choosing the right patients for this surgery is very important. Doctors look at the patient’s health history, current condition, and how well they might recover. They check how bad the heart failure is, if there are other serious health issues, and the patient’s overall health and mental state. They use tools like echocardiography and cardiac catheterization to check the patient’s health and decide if they can have the surgery.
The surgery to put in an artificial heart is long and detailed. First, the patient is put on a machine that keeps blood flowing and oxygen levels up while the heart is stopped. Then, the team removes the patient’s heart, being careful to keep the blood vessels and tissue for the artificial heart. The artificial heart is then put in, and the blood vessels are connected to it. The team must be very careful to make sure the device fits and works right.
After surgery, patients go to the ICU for close watch and care. The first days are very important for managing pain, stopping infections, and making sure the artificial heart works well. The team keeps a close eye on the patient’s health and adjusts the device as needed. They also help the patient and their family with any worries and support them through recovery.
As patients get better, they start to breathe on their own and start their recovery. The medical team keeps checking on them and makes changes to their care as needed to help them get the best results.
The survival rates of artificial heart technology are key for patients with severe heart failure. As we improve this field, knowing these stats is vital for doctors and patients.
In the first two years after getting an artificial heart, survival rates have greatly improved. Most patients make it past the initial period, with some studies showing up to 90% survival at one year.
For example, a study on the SynCardia Total Artificial Heart found a one-year survival rate of about 86%. These numbers are encouraging, showing how far we’ve come in device tech and care.
Looking at two to five years, we see that artificial hearts are effective for longer. While survival rates drop over time, many patients keep benefiting from these devices.
A review showed that at three years, survival rates were between 50% and 70%. This range highlights the need for personalized care and device choice.
Surviving five years or more with an artificial heart is a growing area of interest. Early signs suggest some patients can live for many years with these devices.
Some studies have reported patients living up to seven years or more. These long-term outcomes depend on device quality, patient health, and post-implant care.
To better understand survival rates, let’s look at a comparative table:
| Time Frame | Survival Rate Range | Device Examples |
| 1 Year | 80% – 90% | SynCardia Total Artificial Heart, Abbott HeartMate3 LVAD |
| 3 Years | 50% – 70% | CARMAT Total Artificial Heart, Ventricular Assist Devices (VADs) |
| 5+ Years | 30% – 50% | Long-term VADs, Advanced Total Artificial Hearts |
As we keep improving artificial heart tech, we’ll see better survival rates. The data here shows the current state of artificial heart tech and its promise for severe heart failure patients.
Many factors affect how long someone can live with a mechanical heart. It’s important for patients and doctors to know these to manage hopes and improve care.
Things about the patient greatly influence artificial heart longevity. These include:
The type and quality of the artificial heart device also matter a lot. Important device factors include:
Here’s a look at survival rates for patients with different artificial hearts:
| Device Type | 1-Year Survival Rate | 5-Year Survival Rate |
| Total Artificial Heart (TAH) | 80% | 40% |
| Left Ventricular Assist Device (LVAD) | 85% | 50% |
| Biventricular Assist Device (BiVAD) | 75% | 35% |
In summary, both patient and device factors greatly affect artificial heart longevity. Understanding and managing these can help doctors provide better care. This can lead to better outcomes and a better life for patients.
A mechanical heart changes a person’s life a lot. It affects how active they can be, how they feel emotionally, and how often they see doctors. We’ll look at what it’s like to live with a mechanical heart. This includes physical limits, emotional changes, and the need for regular doctor visits.
Having a mechanical heart means you have to adjust to new limits. These devices help people live longer, but also limit what they can do. Doctors usually tell patients to avoid heavy lifting and hard exercise.
Even with these limits, many people can do daily tasks like walking and light exercise. They might also be able to work, depending on their health and the type of heart device they have. The goal is to stay healthy without risking the heart device.
Adjusting to a mechanical heart is tough on the mind and heart. People feel many emotions, from relief to worry about their device and health.
It’s important to have support from loved ones and mental health experts. Many find help in counseling or support groups. These places let people share their feelings and learn how to cope.
Regular doctor visits are key for mechanical heart patients. These visits help make sure the device is working right and check the patient’s health.
Doctors might do blood tests, imaging, and check the device during these visits. Patients also learn to watch for signs of trouble at home. This way, they know when to get help fast.
| Aspect of Daily Life | Adjustments Required | Benefits |
| Physical Activities | Avoid heavy lifting and strenuous exercises | Can resume walking and light exercises |
| Psychological Well-being | Coping with anxiety and emotional changes | Support from family, friends, and professionals |
| Medical Compliance | Regular medical check-ups and monitoring | Early detection of possible problems |
Having a titanium heart can save lives, but it comes with risks. We need to know about the challenges of artificial heart technology. It’s important to understand these details.
One big risk with titanium hearts is mechanical failure. These can be small problems or serious issues that need quick medical help.
Infections are a big worry for those with artificial hearts. The risk of infection is higher because of the implantation process and the device in the body.
Biocompatibility is key. The materials of the artificial heart must not harm the body’s tissues to avoid bad reactions.
People with titanium hearts face risks of stroke and blood clots. The artificial heart’s surfaces can trigger clotting in the body.
Knowing about these risks is key for patients and doctors. By understanding these challenges, we can work to improve life for those with titanium hearts.
Artificial hearts and heart transplants are two lifesaving options for severe heart failure patients. Each has its own benefits and challenges. We’ll look at survival rates, quality of life, and when each is recommended.
Survival rates differ between artificial hearts and heart transplants. Heart transplants often have better long-term survival. But artificial heart technology has improved, making them a good option too.
A study in a Journal shows one-year survival rates. Heart transplant patients have an 85-90% rate, while artificial heart patients have about 80%. The five-year survival rate for transplants is 75%, versus 60% for artificial hearts.
Quality of life is key when comparing these treatments. Heart transplant patients often see a big improvement in their lives. Artificial heart patients also see improvements, but face device maintenance challenges.
Artificial heart patients must follow a strict maintenance routine. Heart transplant patients have fewer device-related tasks but must take medication to prevent rejection.
The choice between artificial hearts and heart transplants depends on several factors. These include the patient’s health, heart failure severity, and transplant eligibility.
Heart transplants are for patients who are good candidates. Artificial hearts are for those not immediately eligible for a transplant or waiting for one.
Here’s a comparison of the two:
| Criteria | Artificial Hearts | Heart Transplants |
| Survival Rate (1 year) | 80% | 85-90% |
| Survival Rate (5 years) | 60% | 75% |
| Device Maintenance | High | Low |
| Quality of Life Improvements | Significant | Significant |
In conclusion, both artificial hearts and heart transplants offer hope for advanced heart failure patients. Heart transplants may have better long-term survival. But artificial hearts are a good alternative, mainly for those waiting for a transplant or not eligible.
Artificial heart technology is getting better, but it comes with big costs. Patients and healthcare systems face many expenses. These include the cost of the device, care, and insurance.
Patients have to pay for ongoing care after getting an artificial heart. This includes batteries and regular doctor visits. They also might need to replace parts or deal with complications.
Key ongoing expenses include:
Getting insurance for artificial hearts in the U.S. can be hard. Many insurers cover the costs, but how much varies. Medicare, Medicaid, and private insurance have different rules.
Patients need to talk to their doctors and insurers to know what they’ll pay.
In summary, the cost of artificial heart technology is a big deal. Patients and doctors must understand these costs and insurance to get this life-saving tech.
Artificial hearts are living longer thanks to new technologies. These advances are key to better patient care and quality of life for those with artificial hearts.
Research focuses on new materials and surfaces that are safe for the body. These help lower the chance of infections and device failures. Biocompatible materials aim to reduce bad reactions and boost the artificial heart’s performance.
Power systems and wireless charging have seen big improvements. Wireless charging means no cables, cutting down on infections and boosting mobility. New power systems also make energy transfer more efficient, leading to longer battery life and less recharging.
Control algorithms and pumping systems are getting smarter. They let the artificial heart adjust to the body’s changing needs. This means better blood flow and pressure control, leading to better heart function and fewer complications.
These new technologies are changing artificial heart care. They bring hope and better lives to patients.
Artificial heart technology has come a long way, changing lives for the better. Robotic hearts have not only saved lives but also made them better. This is true for many people around the world.
We’re looking forward to even more progress in the future. We expect to see stronger, more efficient, and more compatible artificial hearts. These improvements will help people live longer and healthier lives with robotic hearts.
The outlook for living with robotic hearts is bright. Scientists and engineers are working hard to solve the challenges we face today. As technology gets better, more people will benefit from these amazing devices.
The lifespan varies based on the artificial heart type, patient health, and care after surgery. Some have lived for years with an artificial heart.
An artificial heart is a mechanical device that replaces or supports a biological heart. A biological heart is a natural, muscular organ that pumps blood.
There are several types, including Total Artificial Hearts (TAHs), Ventricular Assist Devices (VADs), and Biventricular Assist Devices (BiVADs). Each serves different purposes and patient needs.
Yes, many patients with mechanical hearts can lead normal lives. They need to make some adjustments and get regular medical checks to ensure the device works well.
Risks include mechanical failures, infection, stroke, and blood clotting. Advances in technology and care have reduced some of these risks.
The surgery is complex and can take several hours. The exact time depends on the patient’s condition and the device type.
Yes, research is ongoing to improve device durability, reduce power needs, and enhance patient quality of life. Innovations include wireless charging and advanced control algorithms.
Both artificial hearts and heart transplants can extend life significantly. The choice depends on the patient’s health and donor heart availability.
Costs include the procedure, device, and maintenance. Insurance coverage varies, and financial help may be available to manage costs.
Yes, artificial hearts can act as a bridge to heart transplantation. They support patients until a donor heart is available.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!