Last Updated on November 27, 2025 by Bilal Hasdemir
In the United States, over 3,500 people get a heart transplant every year. But, there are not enough donor hearts to meet the need. This problem has led to the creation of artificial heart technology. It gives hope to those with severe heart failure.
We are on the edge of a big change in heart care. Mechanical hearts and titanium hearts are being made to help or replace the human heart. These new options are not just saving lives. They are also making life better for many patients.
Looking into the future of living with a robotic heart, we learn more about this technology. We see how it affects patients and healthcare workers.
The human heart is truly amazing, but when it stops working, mechanical hearts can save lives. Our heart pumps blood all over our body, giving us oxygen and nutrients. Knowing how it works helps us understand the role of mechanical hearts.
The heart has a complex system of chambers and valves. It has four main parts: the right and left atria, and the right and left ventricles. The atria take in blood, while the ventricles push it out into our body.
The heart’s electrical system controls the beat. It includes the sinoatrial node, atrioventricular node, and bundle of His. This system makes sure the heart muscle contracts in sync.
The heart must pump blood well to keep us alive. If it can’t, we get heart failure. Heart failure can happen for many reasons, like heart disease or high blood pressure.
Heart failure means the heart can’t pump enough blood. It can’t pump well (systolic failure) or fill up properly (diastolic failure). Symptoms include shortness of breath and swelling in the legs.
A famous heart surgeon, said,
“The heart is a muscular organ that is not always able to repair itself, and when it fails, we need to find alternative solutions.”
When this happens, mechanical hearts or cardiac devices can be lifesavers. They help the heart pump or even replace it. The choice depends on how bad the heart failure is and the patient’s health.

The journey of artificial heart technology has been truly groundbreaking. From its early beginnings to today’s advanced devices, it’s a major leap forward. This technology is a key part of treating heart failure.
The idea of an artificial heart has been around for decades. Early trials and models set the stage for today’s devices. The Jarvik-7, created in the 1980s, was a major step forward.
This total artificial heart (TAH) aimed to replace a failing heart. It marked the start of a new chapter in mechanical heart support. Even with its challenges, it opened doors for future improvements.
After the Jarvik-7, artificial heart tech has seen big strides. Today’s devices are more advanced, with better performance and results. Ventricular assist devices (VADs) and total artificial hearts (TAHs) now offer real hope for those needing a heart transplant.
These updates have boosted survival rates and improved life quality for heart failure patients. The field keeps evolving, with research aiming for even better, more reliable devices.
The field of artificial heart technology has grown a lot. Now, there are many devices to help or replace the heart. These are key for those with heart failure, giving them a better chance at life.
Total Artificial Hearts replace the whole heart. They are for those with severe heart failure. These devices pump blood all over the body.
Key Features of TAHs:
Ventricular Assist Devices are mechanical pumps that help the heart. They can support one or both ventricles. VADs are used as a bridge to heart transplant or for long-term support.
Types of VADs:
| Type | Description | Usage |
| LVAD (Left Ventricular Assist Device) | Assists the left ventricle | Commonly used for left ventricular failure |
| RVAD (Right Ventricular Assist Device) | Assists the right ventricle | Used for right ventricular failure |
| BiVAD (Biventricular Assist Device) | Assists both ventricles | Used for biventricular failure |
Artificial hearts can be temporary or permanent. Temporary ones help until a transplant is possible. Permanent ones are for long-term use, providing lasting support.
Comparison of Temporary and Permanent Artificial Hearts:
| Feature | Temporary Solutions | Permanent Solutions |
| Purpose | Bridge to transplantation | Destination therapy |
| Duration of Use | Short to medium term | Long term |
| Patient Needs | Support until transplant | Long-term heart support |
A mechanical heart works through its design, power, and control systems. It’s made to help or replace the heart, improving life quality. This device is a key part of modern heart care.
The materials for a mechanical heart are key for its durability and safety. Titanium and advanced polymers are used for their strength and how well they fit with the body. These materials help avoid rejection and ensure the device lasts.
Building a mechanical heart requires precise engineering. It’s made to mimic the natural heart’s structure and function. This includes creating parts that work well with the body’s heart system.
| Material | Properties | Benefits in Mechanical Hearts |
| Titanium | Strong, lightweight, corrosion-resistant | Durable, long-lasting |
| Advanced Polymers | Flexible, biocompatible | Reduces risk of rejection, adaptable |
A mechanical heart needs a steady power source. Most use rechargeable batteries, either worn or implanted. Advancements in battery technology have made these devices safer and longer-lasting.
The power source connects to the heart through a driveline or wirelessly. Wireless tech is gaining ground, as it lowers infection risks from drivelines.
The control system of a mechanical heart is advanced. It allows for real-time monitoring and adjustments. Healthcare professionals can fine-tune the device to meet patient needs.
Monitoring tracks heart rate, blood pressure, and device performance. This data is vital for managing the patient’s health and adjusting the device as needed.
Understanding mechanical hearts’ materials, power, and control systems shows their complexity and innovation. As technology advances, we can expect better performance and outcomes for these devices.
Implanting an artificial heart is a detailed process. It involves choosing the right patient and using precise techniques. This surgery is a lifeline for those with severe heart failure, helping them wait for a transplant or live longer with the device.
Before the surgery, patients go through a detailed check-up. This check-up looks at their medical history, current health, and surgery risks. We consider their overall health, heart failure severity, and recovery chances.
A team of doctors, including cardiologists and surgeons, work together. They decide the best treatment for the patient, weighing the benefits and risks of the artificial heart.
| Evaluation Criteria | Description | Importance |
| Medical History | Review of previous illnesses, surgeries, and treatments | High |
| Current Health Status | Assessment of current health, including heart function | High |
| Risk Assessment | Evaluation of possible surgical risks and complications | High |
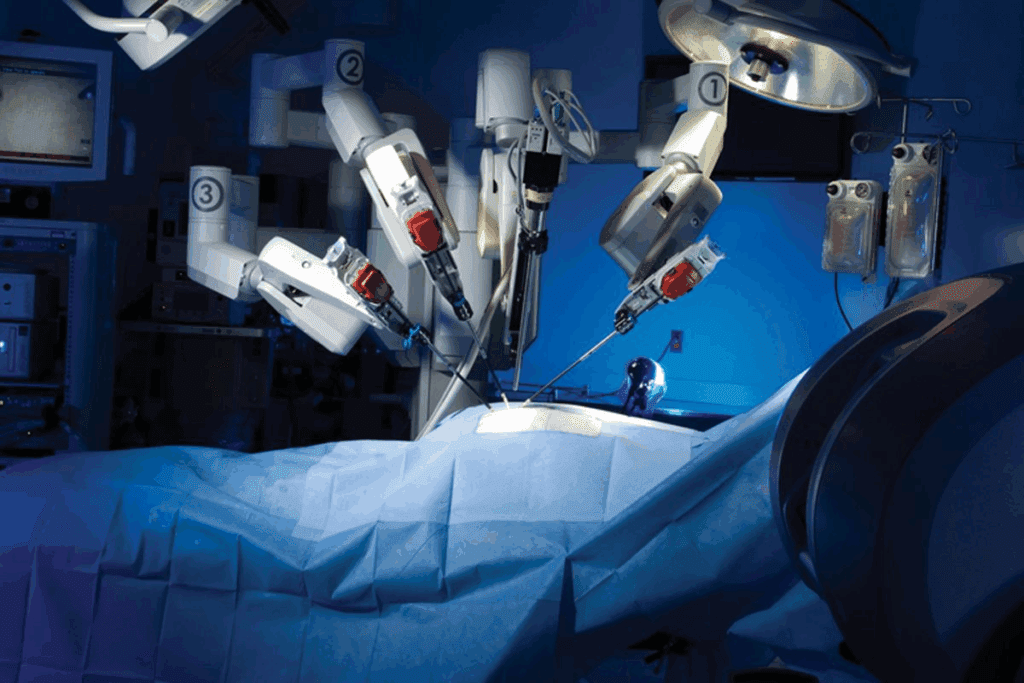
The surgery to implant an artificial heart is very complex. It needs a skilled team. The failing heart is removed, and the artificial heart is put in its place.
We use the latest technologies to make the surgery precise and safe. The artificial heart is connected to blood vessels. Its function is watched closely during the surgery.
After surgery, patients are watched closely in the ICU. We manage pain, prevent infection, and check the artificial heart’s function. This care is vital for recovery.
We also support patients and their families. We teach them how to care for the artificial heart. This support is key for recovery and long-term health.
Understanding the artificial heart implantation process shows the care and complexity involved. As technology improves, we expect better outcomes for patients worldwide.
Many patients worldwide live with artificial hearts. This brings both challenges and chances for a better life. Their days are filled with managing their health, keeping their device in good shape, and adjusting to new things.
People with artificial hearts face special physical challenges. These devices help or replace the heart but limit what they can do. For example, they might not be able to play contact sports or lift heavy things.
Capabilities: Yet, many can do everyday tasks and even some exercise. This makes their lives better.
Limitations: But, they must avoid hard activities and sports to keep their device safe.
| Activity | Allowed | Not Allowed |
| Walking | Yes | No |
| Contact Sports | No | Yes |
| Light Exercise | Yes | No |
Keeping an artificial heart working right means regular checks. You need to watch the power, look for infection signs, and take your medicine as told. Patients and their helpers must stay alert to avoid problems.
Some key maintenance tasks are:
Adapting to life with an artificial heart is tough. Patients must accept their new situation and the device in their body. They also face lifestyle changes. Support from doctors, family, and groups helps a lot.
Helping with the mental side includes:
Artificial heart transplants save lives but come with big medical challenges. Patients face many issues that can affect their life quality and survival chances.
Infections are a big worry with artificial heart transplants. The surgery site and the device can get infected. This can be very serious and even deadly.
We watch patients closely for signs of infection. We act fast to stop serious problems.
Infection prevention strategies include antibiotics, careful wound care, and teaching patients to spot early infection signs. Even with these steps, infections are a big risk, mainly right after surgery.
Mechanical failures are another big challenge. The device’s parts can wear out and fail. This can lead to serious problems.
We stress the need for regular check-ups and device monitoring. This helps catch issues before they get worse. New technology has made artificial hearts more reliable, but we must stay vigilant.
Blood clots and stroke are serious risks with artificial heart transplants. The device’s surface can cause clots, leading to stroke or device failure. Patients need anticoagulation therapy to lower this risk, but it also has its own dangers, like bleeding.
It’s a tricky balance to prevent clots without causing too much bleeding. We work closely with patients to keep their treatment right. This helps reduce these risks.
Stories of people living with robotic hearts are truly inspiring. They show how artificial heart technology has changed lives for the better. It brings hope and improves the quality of life for many.
Many patients have lived with artificial hearts for a long time. They have beaten the odds and shown what’s possible with this technology. For example, Robert Tools got a SynCardia total artificial heart and lived 414 days before getting a transplant.
These long-term survivors prove that artificial hearts can be a bridge to a transplant or even a permanent solution. Their stories highlight the progress in medical technology and the hard work of healthcare teams.
| Patient Name | Device Type | Duration with Device |
| Robert Tools | SynCardia TAH | 414 days |
| John Smith | HeartMate 3 | 720 days |
| Jane Doe | CardioWest TAH | 180 days |
Patients with robotic hearts share their experiences, giving us a glimpse into their lives. They talk about better health and a new sense of purpose.
“I was given a second chance at life with my artificial heart. It’s been a journey, but I’m grateful for every day I get to spend with my loved ones.”
— John Smith, HeartMate 3 recipient
These stories inspire hope for others facing similar challenges. They highlight the benefits of artificial heart technology, like longer lives and better quality of life.
Artificial heart technology is getting better, but the cost is a big deal for patients. The cost includes the surgery, the device, and ongoing care. Insurance and financial help can also play a role.
The first cost is the surgery and the device. A team of experts does the surgery, adding to the cost. The device itself is also very expensive.
Several things affect the cost:
The initial cost can be between $100,000 and over $300,000, depending on the case.
Patients with artificial hearts need ongoing care. This includes regular check-ups, battery replacements, and possible repairs or upgrades.
These costs can add up over time. Annual costs can range from $10,000 to $50,000 or more, based on the device and patient’s health.
Getting insurance and financial help for artificial hearts can be tough. Insurance coverage varies a lot. Some cover all costs, while others cover less.
Patients should:
Knowing the costs and available help can help patients make better choices.
As artificial heart tech gets better, we face more ethical questions. We’re exploring new ways to treat heart failure. But we must also think about the tough ethical issues that come with it.
How we use resources for synthetic hearts is a big ethical issue. These devices are expensive. So, we wonder who gets them and how they’re shared in healthcare.
Deciding how to care for patients with synthetic hearts at the end of life is tough. It’s a big ethical challenge.
Key issues include:
Using synthetic hearts makes us think about quality versus quantity of life. These devices can extend life but also affect quality of life.
Factors to consider include:
As we advance synthetic heart tech, we must keep looking at these ethical questions. This way, we can give our patients the best care. And we’ll think about how it affects society too.
Patients and doctors must think carefully about artificial hearts and heart transplants for advanced heart failure. Both have changed how we treat heart disease, giving hope to those with few choices.
An artificial heart is a mechanical device that can replace or support a failing heart. It’s a lifesaver for those waiting for a transplant or not eligible. But, it needs power, which can limit movement, and there’s a chance it could fail.
A heart transplant means swapping a sick heart with a healthy one from a donor. It’s a lasting fix, but donor hearts are rare. Patients also risk their body rejecting the new heart.
Choosing between an artificial heart and a transplant depends on many things. This includes the patient’s health, how bad their heart disease is, and if they can get a transplant. For example, those waiting for a transplant might get an artificial heart as a temporary fix.
Those not eligible for a transplant might see an artificial heart as a long-term option. The right choice depends on a detailed look at each patient’s situation by a healthcare team.
New trends in artificial heart tech are changing lives. They’re making treatments better and life quality higher. We’re entering a new age in fighting heart failure.
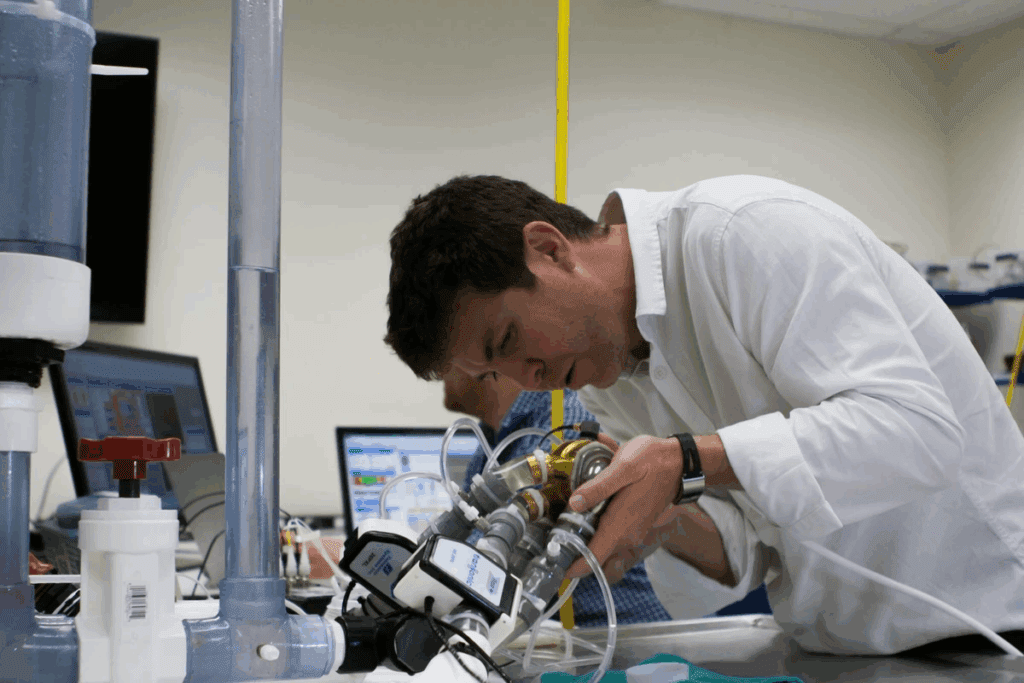
The field of artificial heart tech is growing fast. Research on new materials and ways to make them is creating stronger, better devices.
One exciting area is using biocompatible materials. These materials blend well with the body, cutting down on risks and improving results.
Technology is making artificial heart parts smaller. This makes them less invasive and more comfortable for patients. At the same time, new materials are being made to last longer and withstand wear and tear.
These advanced materials help devices work better with the body. This could lead to fewer problems and a better life for patients.
Biocompatibility is key for artificial heart success. New breakthroughs aim to lower the risk of blood clots and infections. These are big issues with artificial hearts.
“The development of biocompatible materials is vital for artificial heart tech. It affects patient safety and how long the device lasts.”
A Cardiothoracic Surgeon
Improving biocompatibility means safer, more effective artificial hearts. This makes them a better choice for more patients.
Looking at the world of artificial heart tech, we see a big issue: getting to it. How easy it is to get a titanium heart varies a lot around the globe.
How well a country’s healthcare system works is key. In places like the U.S. and many European countries, getting a titanium heart is easier.
In the U.S., for example, there are top-notch hospitals and doctors ready to help. But in poorer countries, not having the right medical setup makes it hard to get these treatments.
Getting a titanium heart isn’t just about where you live. It also depends on how much money you have. People with less money often struggle to get these treatments.
Also, how well a patient does after getting a titanium heart can change a lot. Countries with strong healthcare systems usually see better results because of better care.
We need to make sure everyone has a fair shot at these life-saving treatments. We should work on getting better healthcare to more places and help those who can’t afford it.
By tackling these problems together, we can make titanium heart tech more available. This will help improve health outcomes for people all over the world.
Artificial hearts are key in treating heart failure. They act as a bridge to transplant and as a long-term solution. Medical technology keeps getting better, making artificial hearts even more important for patient care.
Artificial hearts help patients waiting for a transplant. They keep blood flowing and organs working. This support boosts the patient’s chances of making it until a donor heart is found.
Key benefits of using artificial hearts as a bridge to transplant include:
For those not getting a transplant, artificial hearts offer long-term support. This therapy has greatly improved life quality and survival rates for those with severe heart failure.
“The use of artificial hearts as destination therapy has revolutionized the treatment of heart failure, providing patients a viable alternative when transplant is not an option.”
Artificial hearts have greatly changed how we manage heart failure. They offer both short-term and long-term solutions. This has opened up more treatment options for patients and doctors.
The overall impact on heart failure management includes:
As we keep improving artificial heart technology, we’ll see more ways to treat heart failure. This will lead to better care and outcomes for patients.
Artificial heart technology has made big steps forward. It now offers hope to those with heart failure. Many are now living with a robotic heart, enjoying a better quality of life.
This technology has changed lives for many. It’s a real option for those who can’t get a heart transplant. While it comes with its own set of challenges, the benefits are clear. And the tech keeps getting better.
Thanks to total artificial hearts and ventricular assist devices, more patients have options. These devices are not just a quick fix. They’re a long-term solution, helping people live active lives.
The future of artificial heart tech looks bright. Researchers are working hard to make these devices last longer and work better. As this tech improves, we’ll see even more positive changes in the lives of those with robotic hearts.
An artificial heart is a device that replaces or supports a failing heart. It uses mechanical or synthetic parts to pump blood.
It uses a mechanical pump to move blood. This pump is often powered by batteries or an external source. It’s controlled to act like a real heart.
There are Total Artificial Hearts (TAHs) and Ventricular Assist Devices (VADs). They can be temporary or permanent, depending on the patient’s needs.
A TAH replaces the whole heart. A VAD helps one or both ventricles pump better. The choice depends on the heart failure’s extent and the patient’s needs.
Lifespan varies. It depends on the device’s quality, the patient’s health, and post-op care. Some live for years.
Risks include infections, mechanical failure, blood clots, and stroke. Proper care and monitoring can reduce these risks.
An artificial heart can greatly improve life. But, patients may face physical limits and need to follow a specific care routine.
Costs include surgery, device, and ongoing care. Prices vary by device, location, and insurance.
Yes, there are financial help programs and insurance options. We can guide you on finding these resources.
Future advancements include smaller sizes, better materials, and biocompatibility. These changes promise better results and wider access for patients.
Sometimes, it’s a long-term solution. Other times, it’s a bridge to a transplant. It depends on the patient’s condition and medical advice.
Artificial hearts are key in managing heart failure. They provide support, improve circulation, and enhance life quality for those with severe heart disease.
Yes, they can be used with medications and lifestyle changes. This combination can improve heart failure management and patient outcomes.
Age is considered, but not the only factor. Health status, medical history, and other factors also play a role.
Benefits include better survival rates, improved life quality, and increased mobility for those with severe heart failure.
It involves selecting the right patient, a complex surgery, and detailed post-op care. This ensures a successful outcome.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!