Last Updated on November 27, 2025 by Bilal Hasdemir
For those with prosthetic heart valves, artificial valve endocarditis is a serious threat. It can affect both mechanical and bioprosthetic valves. This makes life harder for those who have had valve replacement surgery.
At Liv Hospital, we know how vital expert care is for managing and stopping this infection. We focus on giving full support. We want to teach patients and doctors about the dangers of prosthetic valve endocarditis. We also want to show them how to avoid these risks.
Knowing the causes, signs, and ways to prevent endocarditis of prosthetic valve can greatly lower the risk. Our aim is to give the right info and care. We want to help keep people with prosthetic heart valves healthy and happy.
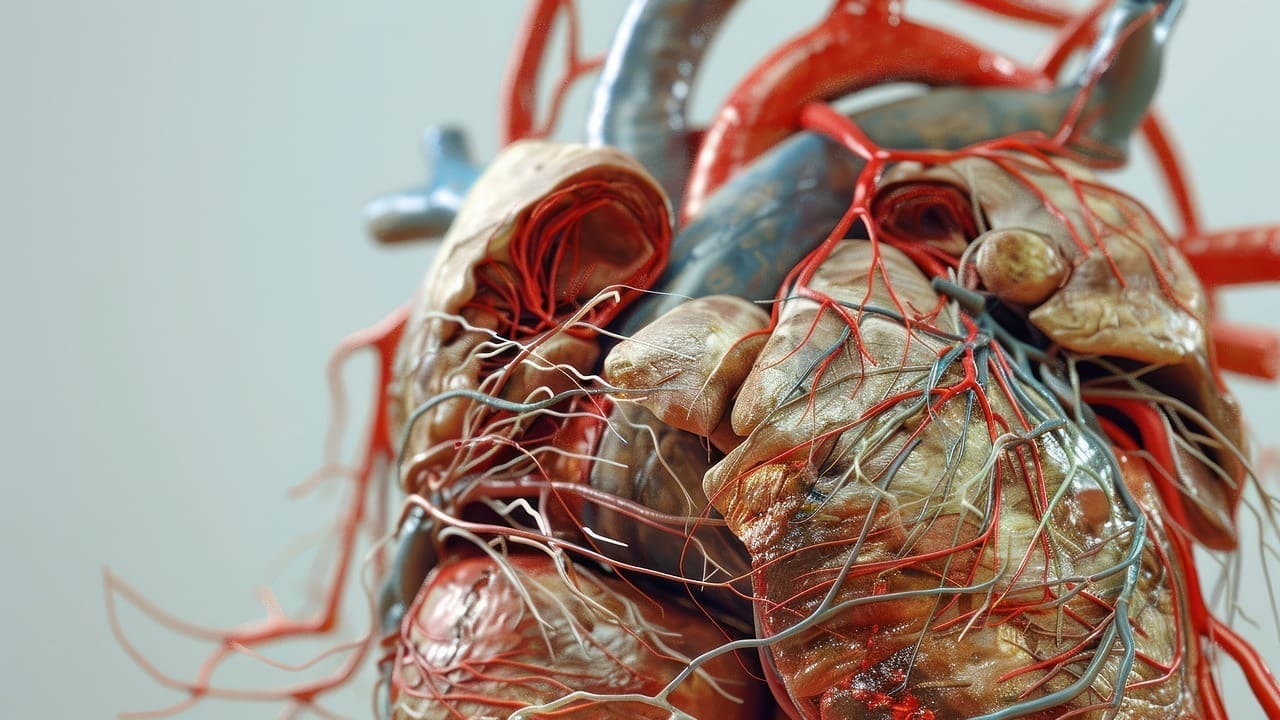
Prosthetic valve endocarditis (PVE) is a big worry for those who have had heart valve surgery. It’s a serious infection of the artificial valve in the heart. Both patients and doctors need to pay close attention to it.
Artificial valve endocarditis is when an artificial heart valve gets infected. It’s a big deal because it can cause serious problems like heart failure and blood clots. The infection can come from bacteria, fungi, or other germs.
The medical community takes PVE seriously because it can be very dangerous. Quick diagnosis and treatment are key to managing it well.
There are two main types of artificial heart valves: mechanical and bioprosthetic. Mechanical valves are made of synthetic materials. Bioprosthetic valves come from animal tissue.
| Valve Type | Material | Risk Factor |
|---|---|---|
| Mechanical | Synthetic materials | Higher risk of infection in the first few months post-surgery |
| Bioprosthetic | Animal tissue | Lower risk initially, but may increase over time due to valve degeneration |
The term PVE stands for Prosthetic Valve Endocarditis. It’s what doctors call an infection of an artificial heart valve. Knowing this term helps patients talk better with their doctors.
“Early detection and treatment of prosthetic valve endocarditis are critical to preventing serious complications and improving patient outcomes.”
Prosthetic valve endocarditis, or PVE, is a serious issue that can happen after heart valve replacement surgery. It has big implications for patient health. Knowing the risks and consequences of PVE is key.
About 6 percent of patients get prosthetic valve endocarditis after valve replacement surgeries. This shows why it’s important to watch patients closely after surgery.
PVE can happen early or late after surgery. Early PVE is within the first year, and late PVE is after that. Knowing when PVE happens helps doctors manage it better.
The main bacteria causing PVE are Staphylococcus aureus, coagulase-negative staphylococci, and streptococci. Finding these bacteria is key for the right treatment.
Some things increase the chance of getting PVE. These include having had endocarditis before, not getting antibiotics for dental work, and using intravenous drugs. Knowing these risks helps prevent PVE.
| Risk Factor | Description |
|---|---|
| Prior History of Endocarditis | Patients with a previous history of endocarditis are at higher risk. |
| Dental Procedures | Dental procedures without proper antibiotic prophylaxis can increase the risk. |
| Intravenous Drug Use | IV drug use is associated with a higher risk of developing PVE. |
Understanding PVE’s incidence, types, causes, and risk factors is vital. This knowledge helps healthcare providers and patients work together. Together, they can reduce the risks of prosthetic valve endocarditis.
Exploring artificial valve endocarditis reveals four key facts. These are essential for healthcare teams and patients to manage and prevent issues with prosthetic heart valves.
Bacterial growth on heart valves is a serious issue. It can lead to embolic events and other severe problems. This growth is made of bacteria, platelets, and fibrin that stick to the valve, possibly causing it to malfunction.
The type of prosthetic valve affects infection risk. Mechanical valves are more likely to get infected early on. On the other hand, bioprosthetic valves might have a lower risk at first but can become more susceptible to infection over time.
Embolic events are a major issue with artificial valve endocarditis. They happen when pieces of bacterial growth break off and travel in the blood. These can cause strokes, organ damage, or other serious problems, making quick diagnosis and treatment critical.
A paravalvular abscess is a serious problem. It’s a collection of pus around the prosthetic valve. Often, it needs surgery along with antibiotics to treat effectively and avoid more issues.
These four facts show how complex artificial valve endocarditis is. They stress the need for detailed care for those with prosthetic heart valves. Understanding these points helps healthcare teams diagnose, treat, and prevent this serious condition.
Prosthetic valve endocarditis (PVE) is a serious issue after heart valve surgery. It’s important to know the last four key facts about PVE. These facts help us understand diagnosis, treatment, and outcomes.
Diagnosing PVE is hard because its symptoms are not clear and prosthetic valves are complex. Clinical diagnosis needs echocardiography, blood cultures, and other imaging. The modified Duke criteria help, but they’re not always clear, mainly in early cases.
“The diagnosis of prosthetic valve endocarditis is often delayed due to its nonspecific presentation, highlighting the need for a high index of suspicion in patients with prosthetic valves,” as noted by experts in the field.
Treatment success for PVE varies based on several factors. Antibiotics are key, and surgery is needed in some cases. Success rates range from 50% to 80%, depending on the patient and treatment.
PVE is linked to high mortality and morbidity. Mortality rates are 20% to 40% in the first year. Many patients face complications like heart failure and need more surgeries.
Long-term outcomes for PVE patients vary. Close follow-up and monitoring are key for better survival and quality of life. With proper care, many patients can live well, but the risk of recurrence is always there.
In conclusion, knowing these final four facts about PVE is vital for healthcare providers. It helps us give the best care to patients with prosthetic heart valves. By understanding these facts, we can manage PVE better and improve patient outcomes.
Prosthetic valve endocarditis shows many signs and symptoms. Knowing these is key to managing the condition well. We will look at the common and unique signs of these infections. This will stress the need for quick action and medical help.
People with prosthetic valve endocarditis often have fever, fatigue, and malaise. These symptoms can be tricky to diagnose. Other signs include heart murmurs, anemia, and embolic events. It’s important to think of prosthetic valve endocarditis when these symptoms appear.
The type of prosthetic valve affects how endocarditis shows up. For example, mechanical valve infections might show valve dysfunction or obstruction. Bioprosthetic valve infections might show leaflet destruction or regurgitation. Knowing these differences helps in diagnosing and treating prosthetic valve endocarditis well.
If you have a prosthetic heart valve and feel severe chest pain, shortness of breath, or fever above 101.5°F (38.6°C), get medical help right away. Quick treatment of prosthetic valve endocarditis can greatly improve your chances of recovery.
Being aware of the signs and symptoms of prosthetic heart valve infections helps both patients and healthcare providers. Together, they can ensure timely and effective management of this serious condition.
We understand that diagnosing and managing endocarditis in mitral and aortic valves is complex. Each valve has its own set of challenges.
Mitral valve endocarditis is tricky because of its location. It can lead to heart failure and embolic events. We must weigh the risks and benefits of different treatments.
Aortic valve endocarditis can cause serious problems like aortic root abscesses and heart block. It’s important to catch it early with advanced imaging.
Imaging is key in diagnosing PVE. We use different methods to check valve function and look for infection signs.
Echocardiography is vital for diagnosing endocarditis. It shows us how the valve looks and works. We look for things like vegetation and abscesses.
Cardiac CT and MRI also help. They give us more info on the infection and any complications.
The modified Duke criteria help us diagnose PVE. They combine clinical, microbiological, and echocardiographic findings. This helps us make accurate diagnoses.
| Diagnostic Criteria | Major Criteria | Minor Criteria |
|---|---|---|
| Modified Duke Criteria | Positive blood cultures, echocardiographic evidence of vegetation or abscess | Fever, vascular phenomena, immunologic phenomena, microbiological evidence |
By using these diagnostic methods and criteria, we can better diagnose and manage endocarditis. This improves outcomes for patients with mitral and aortic valve prosthetics.
Dealing with prosthetic valve endocarditis needs a mix of treatments. This includes using antibiotics and sometimes surgery. We’ll look at the best ways to tackle this serious condition.
Antibiotics are key in treating prosthetic valve endocarditis. The right antibiotics depend on the bacteria causing the infection. Medical studies suggest starting with broad-spectrum antibiotics until the bacteria are known.
Once the bacteria are identified, the antibiotics can be adjusted. Treatment usually lasts 4 to 6 weeks, based on the bacteria and how well the patient responds.
Surgery is often needed for prosthetic valve endocarditis, mainly for complications like heart failure. A team of doctors, including cardiologists and surgeons, will decide if surgery is needed.
Some patients might need another surgery if their valve doesn’t work well or if they keep getting infections. The decision to operate again depends on the patient’s health and the infection’s severity.
Deciding when to have surgery for prosthetic valve endocarditis is tricky. Some patients might need surgery right away, while others can start with antibiotics first. Keeping a close eye on the patient is key.
Handling complications from prosthetic valve endocarditis is vital for better outcomes. This includes treating heart failure and preventing blood clots. A team effort is needed to manage these complex cases.
Recovering from prosthetic valve endocarditis treatment involves many steps. This includes cardiac rehab, watching for long-term issues, and making lifestyle changes. Helping patients understand their condition and supporting them is also important.
By using antibiotics, surgery, and managing complications, we can help patients with prosthetic valve endocarditis get better.
It’s very important to prevent artificial valve endocarditis for those with prosthetic heart valves. We suggest a detailed plan that includes following medical guidelines, making lifestyle changes, and keeping up with regular check-ups.
Antibiotic prophylaxis is advised for those with prosthetic heart valves before dental and medical procedures. This step helps avoid bacterial endocarditis. The American Heart Association has clear guidelines on when to use antibiotics.
Before any medical or dental procedures, tell your healthcare team about your prosthetic heart valve. Some procedures need antibiotics to lower the risk of endocarditis.
Making lifestyle changes can greatly lower the risk of endocarditis. This includes keeping your teeth clean, avoiding intravenous drugs, and managing any ongoing health issues well.
It’s key to keep up with regular visits to your healthcare provider. This helps track your prosthetic valve’s condition and your heart’s health. You’ll need routine check-ups and echocardiograms as advised.
Know the early signs of endocarditis, like fever, tiredness, and trouble breathing. If you notice these symptoms, seek medical help right away.
| Prevention Tip | Description | Benefit |
|---|---|---|
| Antibiotic Prophylaxis | Antibiotics before certain procedures | Reduces risk of endocarditis |
| Good Oral Hygiene | Regular brushing and dental check-ups | Minimizes bacterial entry points |
| Lifestyle Modifications | Avoiding IV drug use, managing chronic conditions | Reduces overall risk factors |
Living with a prosthetic heart valve means you need ongoing medical care. It also means you must take steps to prevent problems like endocarditis. Prosthetic valves can get infected, which is serious and needs quick treatment.
With help from doctors like you can stay healthy. This includes following antibiotic rules, keeping your mouth clean, and seeing a doctor fast if you feel sick.
Knowing the risks and acting early can help you live well. Regular check-ups and care are key to keeping your valve working right.
With the right care, you can lower the risks of a prosthetic valve. This leads to better heart health and a better life overall.
Artificial valve endocarditis, also known as prosthetic valve endocarditis (PVE), is a serious infection. It happens in patients with artificial heart valves. It’s a big worry because it can be very dangerous.
Both mechanical and bioprosthetic heart valves can get infected. The risk and how common it is can differ between the two.
PVE stands for Prosthetic Valve Endocarditis. It’s when the artificial heart valve gets infected.
Common bacteria causing PVE include Staphylococcus aureus, coagulase-negative staphylococci, and streptococci. The type of bacteria can affect treatment and outcome.
Risk factors for PVE include the type of valve, other health conditions, and overall health. Knowing these helps prevent and catch it early.
Diagnosing PVE is hard. It involves clinical checks, imaging like echocardiography, and lab tests. The modified Duke criteria are often used.
Treatment for PVE usually includes antibiotics. Sometimes, surgery is needed. The choice depends on the bacteria, infection severity, and patient’s health.
Preventing PVE includes antibiotics before certain procedures, good oral hygiene, and following up with care. Lifestyle changes and knowing early signs are also key.
Symptoms of PVE include fever, fatigue, and heart failure signs. People with artificial valves should watch for these and seek help if they have them.
PVE’s outcome depends on treatment timing, complications, and patient health. With right care, many recover, but ongoing care is vital.
Patients should follow a detailed management plan. This includes regular checks, preventive steps, and reporting any symptoms to their doctor.
Regular checks are key for catching problems early, like PVE. This leads to better treatment and outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!