Learn asthma physiopathology essentials. Read the essential facts on how triggers lead to irreversible airway remodeling over time. Understanding the pathophysiology of asthma is key to finding good treatments. Asthma is a long-term disease that makes breathing hard. It causes wheezing, coughing, and chest pain, affecting 235 million people globally.
The main issues in asthma are chronic airway inflammation and bronchial hyperreactivity. These problems make breathing even harder. Asthma also causes airway inflammation, makes airways too sensitive, and changes the airway structure.
Key Takeaways
- Asthma is a chronic inflammatory airway disease.
- It affects 235 million people worldwide.
- Chronic airway inflammation and bronchial hyperreactivity are key mechanisms.
- Understanding asthma pathophysiology is key to effective treatment.
- Complex mechanisms include airway inflammation, hyperresponsiveness, mucus hypersecretion, and remodeling.
Understanding Asthma: Definition and Global Impact
Asthma is a chronic condition that affects the airways. It causes wheezing, coughing, and shortness of breath. These symptoms come from inflammation and airway sensitivity.
Clinical Definition of Asthma
Asthma is a chronic inflammatory disease. It leads to recurring symptoms and airflow problems. The pathology of asthma involves inflammation and structural changes in the airways.
“Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation.”
Epidemiology and Global Disease Burden
The epidemiology of asthma shows it’s a big global health problem. About 4% of people worldwide have asthma. It affects their quality of life and healthcare systems.
|
Region |
Asthma Prevalence (%) |
Estimated Population Affected (millions) |
|---|---|---|
|
North America |
8.4 |
29.3 |
|
Europe |
7.1 |
30.4 |
|
Asia-Pacific |
3.5 |
44.8 |
The asthma prevalence highlights the need for more research and awareness. We must find better ways to manage it globally.
Asthma Physiopathology: Core Concepts
Asthma’s pathophysiology is complex, involving chronic inflammation and hyperresponsiveness in the airways. It’s key to understand these concepts to see how asthma impacts patients and evolves over time.
Asthma is more than an allergic reaction. It’s a complex condition with many cellular and molecular processes. At its heart, asthma is marked by chronic inflammation and hyperresponsiveness in the airways.
Chronic Airway Inflammation
Chronic airway inflammation is a key feature of asthma. It results from a long-lasting inflammatory response in the airways. This inflammation causes damage and remodeling, making airways more prone to constriction and obstruction.
Many cell types, like eosinophils and T lymphocytes, play a role in this inflammation. They release inflammatory mediators that keep the inflammation going. Chronic airway inflammation damages the airway epithelium and leads to excess mucus production, further blocking airflow.
Bronchial Hyperresponsiveness
Bronchial hyperresponsiveness is another critical aspect of asthma. It’s when the airways react too strongly to stimuli, causing constriction. This hyperresponsiveness comes from the chronic inflammation, making airways sensitive to many triggers.
The mechanisms behind bronchial hyperresponsiveness involve complex interactions. When an asthma patient meets a trigger, it can cause immediate bronchoconstriction. This leads to symptoms like wheezing, coughing, and shortness of breath.
Understanding the link between chronic inflammation and hyperresponsiveness is vital for managing asthma. By tackling these core mechanisms, we can better control symptoms and improve life quality for those with asthma.
Cellular and Molecular Mechanisms in Asthma
Understanding asthma’s cellular and molecular basis is key to finding better treatments. Asthma is a complex condition with chronic airway inflammation. Many cells and molecules are involved in its development.
Inflammatory Cells in Asthma
Inflammatory cells are at the heart of asthma. Eosinophils are granulocytes that add to airway inflammation. They release proteins that harm airways. Mast cells also play a big role by releasing histamine, causing airways to narrow and produce more mucus.
- T lymphocytes, mainly Th2 cells, are key in asthma’s inflammatory response. They make cytokines like IL-4, IL-5, and IL-13.
- Dendritic cells are antigen-presenting cells that start and keep the Th2 response going.
The interaction between these cells and the airway epithelium is complex. It involves many signaling pathways.
Inflammatory Mediators and Their Effects
Inflammatory mediators are vital in asthma’s development. Histamine from mast cells causes airways to narrow, produce more mucus, and increase blood flow. Leukotrienes, made by mast cells, eosinophils, and basophils, are strong airway constrictors and increase blood vessel permeability.
Cytokines like IL-4, IL-5, and IL-13 are important in inflammation. IL-4 boosts IgE production, IL-5 helps eosinophils survive and work, and IL-13 makes airways more sensitive and produce more mucus.
“The complex interplay between various inflammatory cells and mediators contributes to the heterogeneity of asthma, making it challenging to develop universally effective treatments.”
Expert Opinion
Grasping these mechanisms is vital for creating targeted treatments. These treatments aim to better manage asthma symptoms and improve patient outcomes.
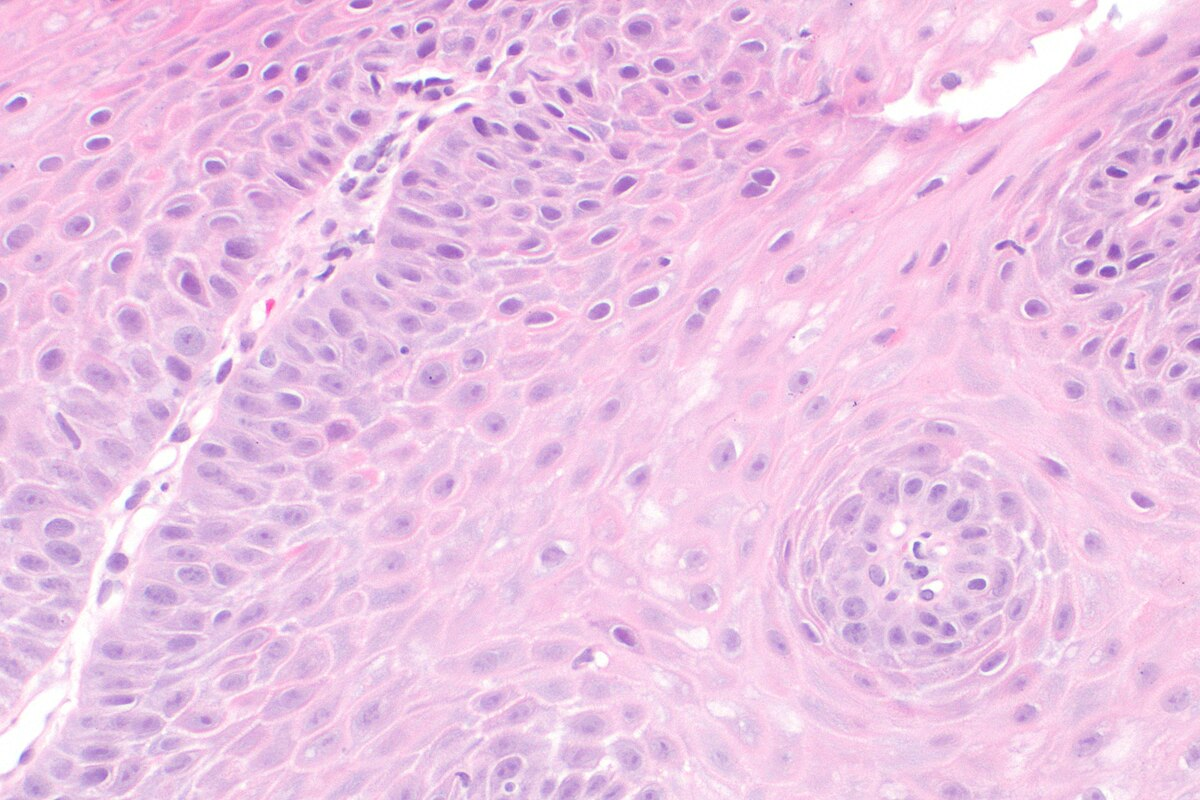
Structural Changes: Airway Remodeling in Asthma
In asthma, the airways change a lot, known as airway remodeling. These changes make it hard to breathe and make the disease worse.
Epithelial Changes
The airway’s first defense is the epithelium. In asthma, this layer gets damaged. There’s more goblet cells and less mucociliary clearance.
This means more mucus and trouble clearing it. It blocks the airways.
Subepithelial Fibrosis
Subepithelial fibrosis is a big part of asthma. It’s when collagen and other proteins build up under the epithelium. This makes the airway wall thicker.
It makes breathing harder and airways more sensitive.
Smooth Muscle Hypertrophy and Hyperplasia
Asthma also makes airway smooth muscle cells bigger and more. This makes it harder to breathe. It’s because of too much muscle.
It’s caused by inflammation and growth factors working together.
Key features of airway remodeling include:
- Epithelial damage and goblet cell hyperplasia
- Subepithelial fibrosis and thickening of the airway wall
- Smooth muscle hypertrophy and hyperplasia
- Increased mucus production and impaired mucociliary clearance
Understanding these changes is key to treating asthma. By focusing on remodeling, we can lessen the disease’s impact. This improves life for asthma patients.
The Acute Asthmatic Response
When someone with asthma breathes in an allergen, their body reacts quickly. This reaction is a key part of how asthma works. It involves many immune cells and substances working together.
Allergen Recognition and IgE Production
The first step is when immune cells recognize the allergen. They then show this allergen to T-helper 2 (Th2) cells. This makes IgE antibodies, which are important in allergies.
These IgE antibodies stick to mast cells. When the same allergen comes back, the IgE antibodies bind to it. This makes mast cells active.
Mast Cell Activation and Mediator Release
When mast cells get activated, they release many substances. These include histamine, leukotrienes, and cytokines. These substances are key in the asthma response. They make airways narrow, increase mucus, and cause inflammation.
Key mediators released during mast cell activation include:
- Histamine: Causes immediate bronchoconstriction and increases vascular permeability.
- Leukotrienes: Contribute to sustained bronchoconstriction and inflammation.
- Cytokines: Promote the recruitment of inflammatory cells to the airways.
Immediate Bronchoconstriction Mechanisms
The release of histamine and other substances causes airways to narrow. This is a key part of the asthma response. The narrowing is due to smooth muscle contraction, making it hard to breathe.
The asthma response is complex, involving many immune cells and substances. Knowing how it works is key to finding good treatments for asthma.
The Late Asthmatic Response
Asthma’s late asthmatic response is a complex mix of cell and molecular actions. It happens hours after exposure to an allergen. Symptoms worsen significantly during this phase.
Cellular Infiltration Patterns
In the late asthmatic response, many inflammatory cells move into the airways. Eosinophils, lymphocytes, and neutrophils are key players in this inflammation and airway damage.
- Eosinophils release granules that harm the airway epithelium.
- Lymphocytes, mainly T-helper 2 cells, lead the inflammatory response.
- Neutrophils add to the inflammation by releasing harmful substances.
Perpetuation of Airway Inflammation
The inflammation in the late asthmatic response is fueled by cytokines and chemokines. These molecules attract and activate inflammatory cells, keeping the airways inflamed.
- Cytokines like IL-4, IL-5, and IL-13 are vital for the inflammatory process.
- Chemokines, such as eotaxin, help bring eosinophils to the airways.
Mucus Hypersecretion and Airway Obstruction
Mucus hypersecretion is a key feature of the late asthmatic response. It greatly contributes to airway blockage. The increase in goblet cells and mucin production drives this excessive mucus.
The mix of airway inflammation, mucus, and smooth muscle contraction causes severe airway blockage. This leads to symptoms like wheezing, coughing, and shortness of breath.
Asthma Endotypes: Beyond Clinical Phenotypes
Asthma is a complex disease with different endotypes, each with its own inflammation. This new understanding changes how we diagnose and treat asthma.
Before, asthma was seen through its symptoms. Now, we look at the deeper pathophysiological processes. This shift helps us better understand and treat asthma.
Type 2-High Asthma
Type 2-high asthma is marked by eosinophilic inflammation. This is caused by type 2 helper T cells and cytokines like IL-4, IL-5, and IL-13. It’s often seen in allergic asthma and responds well to corticosteroids.
The main features of type 2-high asthma are:
- Eosinophilic airway inflammation
- Elevated IgE levels
- Good response to corticosteroids
A leading researcher says, “Recognizing type 2-high asthma has been key in creating targeted treatments. These treatments have greatly improved patient outcomes.”
“Biologics targeting IgE and IL-5 have shown remarkable efficacy in reducing exacerbations and improving quality of life for patients with severe asthma.”
Type 2-Low Asthma
Type 2-low asthma has different inflammation pathways. It often shows neutrophilic or pauci-granulocytic patterns. This type is less responsive to corticosteroids, making treatment harder.
|
Characteristics |
Type 2-High Asthma |
Type 2-Low Asthma |
|---|---|---|
|
Inflammatory Profile |
Eosinophilic |
Neutrophilic or Pauci-granulocytic |
|
Response to Corticosteroids |
Typically responsive |
Less responsive |
|
Common Triggers |
Allergens |
Environmental irritants, infections |
Knowing these endotypes is key for personalized treatment plans. As we learn more about asthma, understanding type 2-high and type 2-low asthma will guide our treatments.
Genetic and Environmental Factors in Asthma Pathophysiology
Asthma’s development and worsening come from a mix of genetic and environmental factors. It’s not caused by one thing alone. Instead, it’s the result of many genetic and environmental elements working together.
Genetic Predisposition
Genetics play a big part in who gets asthma. Scientists have found many genes linked to asthma risk. These genes affect airway inflammation, how airways react, and the immune system’s function.
For example, genes related to IgE production and eosinophil function are connected to asthma. Family history also matters a lot. People with asthma or allergies in their family are more likely to get it. Studies show that genetics are a big part of asthma risk.
Environmental Triggers and Their Mechanisms
Environmental factors are key in starting and making asthma worse. Common culprits include allergens like dust mites, pet dander, and pollen. Air pollutants, such as tobacco smoke and particles, also play a role. Respiratory infections, mainly from viruses, can set off asthma symptoms.
How these triggers affect asthma is complex. Allergens can start an allergic reaction, leading to IgE antibodies and mast cell activation. This causes airway constriction and inflammation. Air pollutants can irritate airways, making inflammation and hyperresponsiveness worse.
It’s important to understand how genetics and environment interact in asthma. By knowing who’s at risk and reducing their exposure to triggers, we can lower asthma’s incidence and severity.
Conclusion
Understanding asthma’s pathophysiology is key to better treatments and outcomes. Asthma is complex, involving inflammation, hyperresponsiveness, and airway changes.
We’ve looked at the main causes of asthma, from inflammation to airway changes. Knowing the different types of asthma helps tailor treatments for each patient.
Asthma’s pathophysiology is a mix of genetics, environment, and immune factors. This summary shows the need for a full approach to managing asthma. It includes medicine and lifestyle changes for better care.
Explaining asthma helps us see its global impact. It also highlights the need for more research. This will improve our care for those with asthma.
FAQ
What is the pathophysiology of asthma?
Asthma’s pathophysiology involves chronic inflammation and airway hyperreactivity. These lead to recurring symptoms and damage to the airways.
What are the main characteristics of asthma?
Asthma is marked by chronic inflammation and airway hyperreactivity. Symptoms include wheezing, coughing, and shortness of breath.
How does chronic airway inflammation contribute to asthma?
Chronic inflammation damages the airways and makes them more sensitive. This sensitivity leads to symptoms and disease progression.
What is airway remodeling in asthma?
Airway remodeling changes the airway structure. It includes fibrosis and muscle growth, leading to persistent airflow issues and disease severity.
What happens during an acute asthmatic response?
An acute asthmatic response starts with allergen recognition and IgE production. Mast cell activation releases histamine, causing immediate bronchoconstriction and symptoms.
What is the late asthmatic response?
The late asthmatic response happens hours after allergen exposure. It involves cellular infiltration, ongoing inflammation, and mucus hypersecretion, causing airway obstruction and symptoms.
What are asthma endotypes?
Asthma endotypes categorize asthma based on inflammation types. They include type 2-high asthma with eosinophilic inflammation and type 2-low asthma with different pathways.
How do genetic and environmental factors contribute to asthma?
Genetics can make someone more susceptible to asthma. Environmental triggers like allergens and pollutants can also trigger or worsen symptoms. Understanding these factors is key for prevention and management.
What is the significance of understanding asthma pathophysiology?
Knowing how asthma works is vital for effective treatments and better patient outcomes. It allows for personalized management strategies based on individual needs.
References
Government Health Resource. Asthma Pathophysiology: Mechanisms and Global Impact. Retrieved from https://ginasthma.org/reports/