Last Updated on November 27, 2025 by Bilal Hasdemir
As we get older, our arteries change a lot. This can lead to atherosclerosis, where plaque builds up in the arteries. This can start as early as the teenage years and gets worse over time. Studies now show that atherosclerotic plaques can grow fast in midlife, unlike what was thought before.
At Liv Hospital, we know how important it is to understand age-related arterial disease and its risks. Our team is here to give top-notch healthcare and support to patients from around the world. We want to help people know about the seven main stages of atherosclerosis and what makes it worse. This way, we can help them take steps to prevent and care for it.
Atherosclerosis is when plaque builds up in artery walls. It can start early in life. This buildup includes fatty deposits, cholesterol, and other substances, causing arteries to harden and narrow.
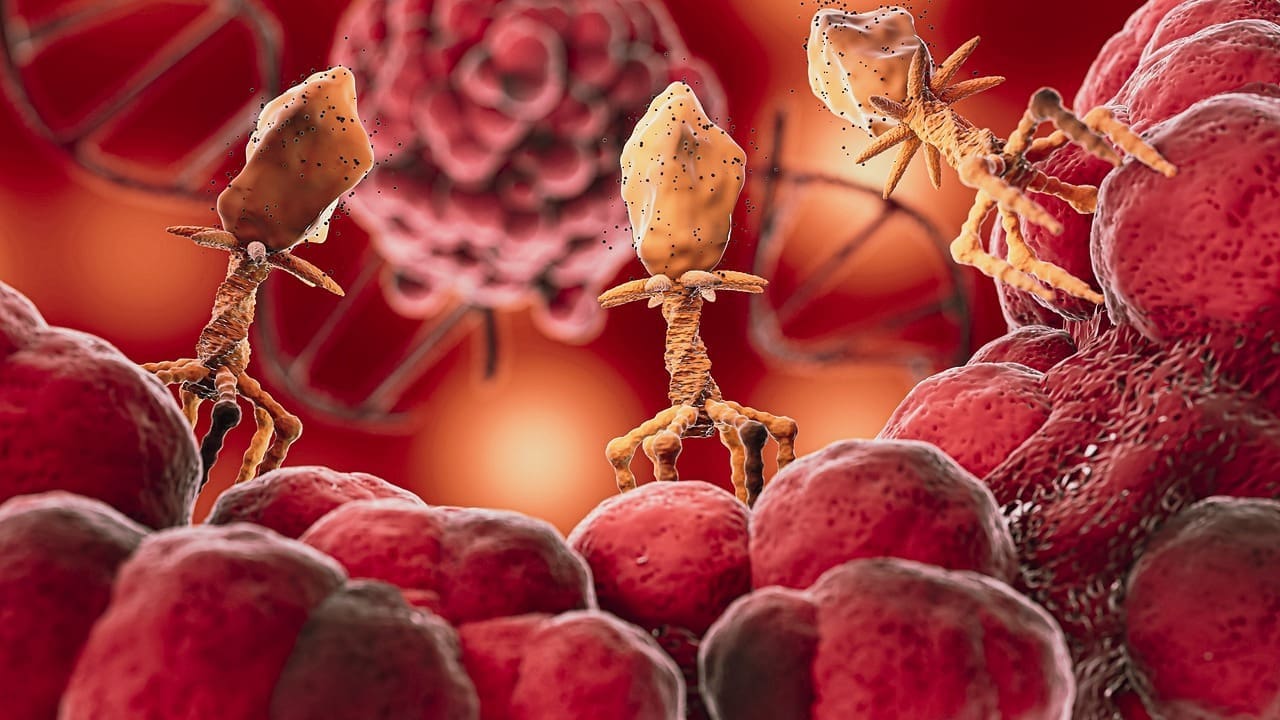
Atherosclerosis involves inflammation, endothelial dysfunction, and lipid metabolism. It starts with monocytes sticking to the endothelial surface. These monocytes then move into the intima, becoming macrophages that take in lipids and turn into foam cells.
This leads to inflammation and the growth of atherosclerotic plaques.
Key components of atherosclerotic plaques include:
As plaques grow, they can narrow the artery, reducing blood flow. This can cause heart disease, peripheral artery disease, and carotid artery disease.
Atherosclerosis is called a “disease of age evolution” because it’s linked to aging. As we age, our arteries change, making atherosclerosis more likely. These changes include stiffer arteries, reduced endothelial function, and altered lipid profiles.
| Age-Related Change | Impact on Atherosclerosis Risk |
|---|---|
| Increased arterial stiffness | Higher risk of plaque rupture |
| Reduced endothelial function | Increased adhesion of inflammatory cells |
| Altered lipid profiles | Increased accumulation of lipids in arterial walls |
Understanding these age-related changes is key to preventing and managing atherosclerosis. By knowing what contributes to its progression, we can develop effective strategies to reduce its impact.
Atherosclerosis doesn’t get worse at the same rate all the time. It speeds up a lot in midlife. Studies show it can grow fast during this time, not as slow as we thought. Knowing how arteries change with age is key to catching the disease early.
The idea that atherosclerosis moves slowly is wrong. Research shows it can speed up a lot during certain life stages, like when we move from young adulthood to middle age. Changes in lifestyle, hormones, and risk factors play a big role in this quickening. For example, a study in Nature points out midlife as a key time for atherosclerosis to worsen.
Arterial changes start early, with fatty streaks forming in teens. These changes grow into more serious plaque in the 20s and 30s. By the 40s, plaque builds up faster, raising the risk of heart problems. Knowing this timeline helps find the best times to act.
Early detection and action are the keys to fighting atherosclerosis. By understanding when and why arteries change, doctors can create better plans to lower risk. This is very important for people with heart disease in their families or those with risk factors like high blood pressure, diabetes, and smoking.
Atherosclerosis starts early, with small changes happening in the teenage years. Understanding these early changes is key to stopping atherosclerosis from getting worse.
Fatty streaks, the first signs of atherosclerosis, can show up in teens. These streaks are made of lipids in the artery walls. Even though they don’t cause symptoms, they mark the start of atherosclerosis.
In young adulthood, changes start to show up that aren’t obvious. The artery walls get thicker, and lipids build up. These changes can lead to serious atherosclerosis later.
It’s important to understand these early signs to prevent atherosclerosis from getting worse. By making healthy choices early, young adults can lower their risk of serious atherosclerosis later.
| Age Group | Common Atherosclerotic Changes | Preventive Measures |
|---|---|---|
| Teenage Years | Formation of fatty streaks | Healthy diet, regular exercise |
| Young Adults | Subclinical changes, intimal thickening | Lifestyle modifications, risk factor management |
By focusing on prevention and early action, we can stop or slow atherosclerosis. This can help lower the risk of heart problems later in life.
In our 20s and 30s, atherosclerosis can quietly start, setting the stage for heart problems later. It often doesn’t show symptoms, making it hard to see the danger. Early prevention and awareness are key to fight atherosclerosis’s silent growth.
In our 20s and 30s, tiny changes start in the arteries. These include fat buildup, inflammation, and smooth muscle cell movement. The changes are slow and often don’t show symptoms until much later.
These changes can cause early atherosclerotic lesions. If not stopped, they can grow over time. Knowing about these changes helps us find ways to prevent them.
Preventing atherosclerosis early is vital. By living a healthy lifestyle in our 20s and 30s, we can lower the risk of serious atherosclerosis later.
“Prevention is better than cure.” This saying is very true for atherosclerosis, where starting early can change the disease’s path.
Some good ways to prevent atherosclerosis early include:
By doing these things, we can greatly lower our risk of heart disease and live better lives.
Entering the 40s often means a big jump in plaque buildup. This is a key time in the growth of atherosclerosis. Many factors come together to speed up artery disease in this decade.
Several things make plaque buildup faster in the 40s. Metabolic changes slow down, and body fat, mainly around the belly, increases. This can cause insulin resistance and higher blood pressure, both risk factors for atherosclerosis.
Lifestyle factors also play a big part. Unhealthy habits like a bad diet, not exercising, and smoking can speed up plaque buildup.
Hormonal changes also affect plaque buildup. For example, menopause in women lowers estrogen levels, increasing the risk of heart disease.
“The fourth decade of life is a critical juncture for cardiovascular health. It’s a period where the cumulative effects of lifestyle choices and age-related changes can significantly impact the progression of atherosclerosis.”
The 40s are a critical intervention window for stopping or slowing atherosclerosis. It’s a time when changing your lifestyle and getting medical help can greatly improve heart health.
It’s important to catch and manage risk factors like high blood pressure, high cholesterol, and diabetes early. Lifestyle changes like eating well, exercising, quitting smoking, and managing stress can help a lot.
By knowing why plaque buildup speeds up in the 40s and acting early, you can lower your risk of serious atherosclerosis and its problems.
The 50s are a key time when atherosclerosis can start showing symptoms. As we get older, plaque in our arteries can cause noticeable changes. These changes often signal a big shift in our heart health.
For years, atherosclerosis might not show any symptoms. But in the 50s, symptoms start to appear more often. This is because arteries get narrower and less flexible, making blood flow harder.
“Atherosclerosis is a ticking time bomb,” a cardiologist said. “And the 50s are when the clock starts to tick louder.”
This decade is key for spotting warning signs and taking action to manage the disease.
In the 50s, atherosclerosis symptoms can differ from person to person. Some common signs include:
Spotting these symptoms early is vital. Early detection and intervention can significantly improve outcomes for those with atherosclerosis. We urge you to watch for any health changes and see a doctor if you notice these signs.
In our 50s, it’s important to be aware of our body’s changes. Working closely with healthcare providers can help manage symptoms. This way, we can control our heart health and lower the risk of atherosclerosis complications.
Entering the 60s brings a higher risk of atherosclerosis. This decade sees more complications from advanced atherosclerotic disease.
Atherosclerosis gets worse, leading to plaque vulnerability and a higher risk of rupture. A ruptured plaque can cause a blood clot, blocking the artery. This can lead to severe heart problems.
Plaque vulnerability is key in predicting heart risks. Vulnerable plaques have a thin cap, a big lipid core, and more inflammation. These traits make them more likely to rupture.
Several things can make plaques more vulnerable, including:
A ruptured plaque can cause heart attacks and strokes. These are often the first signs of advanced atherosclerosis.
It’s important to manage atherosclerosis complications in the 60s. This means making lifestyle changes, taking medication, and sometimes needing procedures. These steps help lower the risk of heart problems.
Healthcare providers can prevent or delay these complications by focusing on plaque vulnerability and rupture risk. This improves outcomes for those in their 60s.
In the 70s, atherosclerosis often gets worse, affecting many blood vessels. This makes managing the disease very hard for both patients and doctors.
By this age, atherosclerosis is not just in one place. It’s in many, making treatment harder.
Multi-territorial atherosclerosis means many blood vessels are affected. This includes the heart, brain, legs, and kidneys. It makes managing the disease more complex and raises the risk of heart problems.
The table below shows which blood vessels can be affected:
| Vascular Territory | Common Manifestations | Potential Complications |
|---|---|---|
| Coronary Arteries | Angina, Myocardial Infarction | Heart Failure, Arrhythmias |
| Carotid Arteries | Transient Ischemic Attack (TIA), Stroke | Cognitive Decline, Disability |
| Peripheral Arteries | Intermittent Claudication, Limb Ischemia | Gangrene, Amputation |
| Renal Arteries | Renovascular Hypertension, Kidney Disease | Chronic Kidney Disease, End-Stage Renal Disease |
Dealing with atherosclerosis in older adults is tough. It’s because of other health issues, many medicines, and finding the right treatment for each person.
Doctors have to think about the patient’s health, how well they can function, and what they want. This might mean changing their diet, taking medicine, or even surgery.
In conclusion, managing atherosclerosis in the 70s needs a careful and detailed plan. Understanding the disease helps doctors tailor treatments for older patients. This can lead to better health outcomes.
End-stage atherosclerosis is a critical point in heart health. At this stage, the disease is at its worst. The arteries are badly damaged, leading to serious health problems and death.
The effects of atherosclerosis on arteries are complex. Years of plaque buildup and inflammation cause severe damage.
End-stage atherosclerosis causes widespread damage to arteries. This damage makes it hard for arteries to control blood flow and pressure.
Key features of severe arterial damage include:
A leading cardiologist notes, “Atherosclerosis’s end stage is a complex process.”
“Atherosclerosis is a diffuse process, affecting multiple vascular beds, and its end-stage represents a failure of both the vascular and the cardiovascular system as a whole.”
End-stage atherosclerosis greatly affects a patient’s quality of life. Symptoms like angina, shortness of breath, and intermittent claudication worsen. These symptoms limit physical activity and lower overall well-being.
| Symptom | Impact on Quality of Life | Mortality Risk Association |
|---|---|---|
| Angina | Reduces physical capacity, increases anxiety | High risk of myocardial infarction |
| Shortness of Breath | Limitations in daily activities, possible heart failure | Increased risk of cardiovascular events |
| Intermittent Claudication | Restricts mobility, affects independence | Associated with higher risk of cardiovascular mortality |
The risk of death from end-stage atherosclerosis is high. Patients face a high risk of heart attacks and strokes. These are major causes of death worldwide.
In conclusion, end-stage atherosclerosis has severe effects on quality of life and survival. Understanding these risks is key for healthcare providers to manage the disease and improve patient outcomes.
We know some risk factors are key in atherosclerosis development. It’s vital to manage these to prevent or slow the disease.
Some risk factors can’t be changed. These include:
Knowing these non-modifiable risk factors helps us spot those at higher risk. This allows for early action and monitoring.
Many risk factors can be changed through lifestyle and medical help. Key modifiable risk factors are:
By managing these modifiable risk factors, we can lower the risk of atherosclerosis getting worse. This is done through lifestyle changes and, if needed, medical treatment.
By focusing on modifiable risk factors, we can create tailored prevention and treatment plans. These plans meet an individual’s specific needs and risk level.
Managing atherosclerosis starts with early detection and timely action. Modern technology and risk stratification help a lot. We can now spot and treat atherosclerosis early, thanks to these advancements.
Modern imaging has changed how we find atherosclerosis. Tests like coronary artery calcium scoring (CACS) and carotid intima-media thickness (CIMT) help spot early changes. These tests are non-invasive and give doctors valuable info to plan treatment.
A study in the Journal of the American College of Cardiology shows CACS’s power. It found people with high CACS scores face a higher risk of heart events than those with low scores.
“The use of coronary artery calcium scoring has emerged as a powerful tool in the assessment of cardiovascular risk, allowing for the identification of individuals who would benefit from more aggressive preventive measures.”
Journal of the American College of Cardiology
Risk stratification is key in managing atherosclerosis. It helps doctors focus on high-risk patients. Methods include the Framingham Risk Score and biomarkers like hs-CRP.
| Risk Stratification Method | Description | Clinical Utility |
|---|---|---|
| Framingham Risk Score | Estimates 10-year cardiovascular risk based on age, sex, blood pressure, cholesterol levels, and smoking status. | Guides preventive therapy and lifestyle counseling. |
| hs-CRP | Measures inflammation, a key component of atherosclerosis. | Identifies individuals at increased risk of cardiovascular events. |
| CACS | Quantifies coronary artery calcium, a marker of atherosclerosis. | Refines risk assessment and guides statin therapy. |
Healthy habits before 40 can prevent atherosclerosis. Eating well, exercising, quitting smoking, and keeping a healthy weight are important. These habits can lower your risk of atherosclerosis later.
Medical treatments are vital for atherosclerosis management. The right time for these treatments depends on your risk and disease level. Statins, antiplatelet drugs, and blood pressure meds are often used.
Choosing and timing treatments should be based on a full risk assessment and disease status.
Managing atherosclerosis early is key to avoiding heart problems and improving life quality. We’ve talked about the seven stages of atherosclerosis, from when it starts in teens to when it’s severe in the elderly.
Preventing atherosclerosis means finding it early, making lifestyle changes, and getting medical help on time. Knowing the risks and taking action can greatly lessen the disease’s impact.
There are ways to treat atherosclerosis, like eating right and exercising, and also using medicines like statins. Taking a proactive stance can slow the disease and lead to better results.
We stress the need for a full plan to handle atherosclerosis, combining prevention and treatment. Together, we can greatly reduce heart disease worldwide.
Atherosclerosis is when plaque builds up in arteries, making them hard and narrow. It grows quietly, often without symptoms until later. It’s called a “disease of age evolution” because it gets worse with age.
Atherosclerosis can start in the teens, with fatty streaks in arteries. Young adults may also see early changes. This shows why starting prevention early is key.
Risk factors include age, genetics, and family history. Lifestyle and certain health conditions also play a part. Changing these can help prevent or slow the disease.
Healthy diet, regular exercise, and not smoking are important. They help prevent or slow atherosclerosis, best when started before 40.
In the 50s, atherosclerosis may start showing symptoms. Look out for chest pain, shortness of breath, and leg pain when exercising. Catching these signs early is vital.
Ultrasound, CT scans, and MRI are used to diagnose atherosclerosis. They help find problems early and guide treatment.
In older age, atherosclerosis can cause serious problems. This includes increased risk of heart attacks and strokes. It also makes managing the disease harder in the elderly.
Yes, lifestyle changes can prevent or slow atherosclerosis. Eating well, exercising, and not smoking are effective. Starting early is best.
Treatment includes lifestyle changes, medicine, and surgery. The right choice depends on the person’s risk, disease severity, and health.
Age-related arterial disease can greatly affect quality of life and increase death risk. It can lead to mobility issues, cognitive decline, and heart problems.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!