Last Updated on November 25, 2025 by Ugurkan Demir
At Liv Hospital, we know many people get confused between atrial fibrillation and atrial flutter. Both are heart rhythm problems but they are different.Understand the difference between atrial fib flutter and atrial fibrillation and learn key treatment facts.
Atrial fibrillation (AFib) has chaotic electrical activity. On the other hand, atrial flutter has a fast but organized circuit. Knowing the difference is key for the right diagnosis and treatment.
We will look at the main differences between AFib and atrial flutter. This includes their unique electrical patterns, symptoms, and how to treat them. We aim to give you a clear picture of these heart conditions.
Key Takeaways
- AFib and atrial flutter are distinct heart rhythm disorders with different electrical patterns.
- Accurate diagnosis is key for effective treatment.
- Treatment approaches vary between AFib and atrial flutter.
- Understanding the differences between these conditions improves patient outcomes.
- Liv Hospital is committed to delivering world-class care for international patients.
Understanding Atrial Arrhythmias

Atrial arrhythmias, like AFib and atrial flutter, affect the heart’s electrical system. They cause irregular heart rhythms in the atria. Knowing about these conditions is key to understanding heart health.
The Normal Electrical System of the Heart
The heart’s electrical system starts with the sinoatrial (SA) node, or the heart’s natural pacemaker. It sends signals that make the atria contract, pushing blood into the ventricles. Then, these signals go to the ventricles through the AV node, making them contract and pump blood.
What Happens During Atrial Arrhythmias
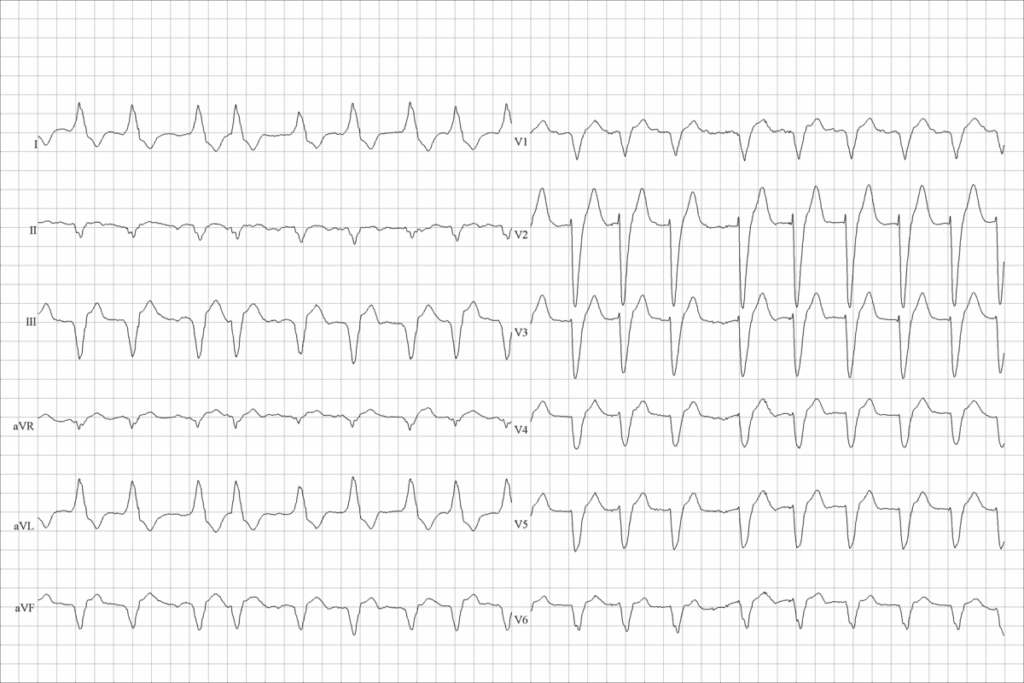
Atrial arrhythmias disrupt the heart’s normal electrical activity. In atrial fibrillation, the atria beat fast and irregularly, causing a quiver. Atrial flutter, on the other hand, has a rapid but regular rhythm, seen as a “sawtooth” pattern on an ECG.
| Characteristics | Atrial Fibrillation (AFib) | Atrial Flutter |
| Atrial Rhythm | Irregular | Regular |
| ECG Pattern | No distinct P waves | “Sawtooth” pattern |
| Heart Rate | Often rapid and irregular | Typically regular and rapid |
It’s important to know the differences between atrial fibrillation and atrial flutter. This helps doctors diagnose and treat these conditions better. By understanding these differences, doctors can manage symptoms and lower the risk of complications.
Atrial Fibrillation: The Chaotic Rhythm
Atrial fibrillation (AFib) is a common heart rhythm disorder. It makes the heart beat irregularly and sometimes too fast. This affects millions globally, causing disorganized electrical activity in the heart’s upper chambers.
Definition and Prevalence
AFib is a heart rhythm disorder that leads to irregular and often fast heartbeats. It’s more common with age, hitting about 9% of those over 65. Men are more likely to get it, often linked to heart disease or other health issues.
| Age Group | Prevalence of AFib |
| Below 49 | Less than 0.1% |
| 50-59 | 0.5% |
| 60-69 | 2% |
| 70-79 | 5% |
| 80 and above | 9% |
Electrical Characteristics of AFib
In AFib, the heart’s electrical activity is chaotic. This leads to irregular heartbeats. The atria beat very fast, often between 300 to 600 times a minute. An electrocardiogram (ECG) shows this by missing a consistent P wave and having an irregular ventricular rate.
Common Triggers and Risk Factors
Many things can trigger AFib or raise your risk. Alcohol, certain meds, and heart conditions like coronary artery disease are common triggers. Other risks include high blood pressure, diabetes, obesity, and sleep apnea. Knowing these can help manage AFib better.
AFib and atrial flutter are related but different. Both are atrial arrhythmias, but they have unique electrical patterns. While they share some risk factors, they are not the same. They can coexist, though.
Atrial Flutter: The Organized Circuit
Atrial flutter shows a unique sawtooth pattern on ECGs. This is because of its organized electrical activity. It’s a condition where the atria’s electrical circuit is fast but regular.
Definition and Prevalence
Atrial flutter is a type of fast heart rhythm that starts in the upper chambers of the heart. It’s less common than atrial fibrillation but is risky. It’s more common with age and often linked to heart disease.
Electrical Characteristics
The electrical activity in atrial flutter creates a consistent pattern on an ECG. This pattern is often called a “sawtooth” or “flutter” wave. It’s most clear in the inferior leads (II, III, and aVF).
Common Triggers and Risk Factors
Atrial flutter has many risk factors similar to atrial fibrillation. These include hypertension, heart failure, and chronic obstructive pulmonary disease (COPD). Other triggers include recent surgery, electrolyte imbalances, and certain medications.
Knowing these risk factors is key to managing atrial flutter. Healthcare providers can create better treatment plans by addressing these factors. This helps lower the risk of complications.
Comparing Atrial Fib Flutter: Key Differences
Atrial Fibrillation (AFib) and Atrial Flutter have different electrical patterns and heart rates. Knowing these differences is key for correct diagnosis and treatment.
Electrical Pattern Distinctions
Atrial Fibrillation (AFib) shows chaotic electrical activity in the atria. This causes the atrial walls to quiver instead of contracting together. Atrial Flutter, on the other hand, has a regular electrical circuit around the tricuspid valve.
The irregularity of AFib comes from many reentrant circuits in the atria. This leads to a variable ventricular response. Atrial Flutter, with a consistent 2:1 or 3:1 AV conduction ratio, has a more predictable ventricular rate.
Heart Rate Variations
The heart rate in AFib can vary a lot, from very fast to normal. This depends on the AV node and any rate-controlling medications. Atrial Flutter, though, usually has a consistent heart rate, influenced by the AV conduction ratio.
For example, a patient with Atrial Flutter might have a heart rate of 150 bpm with a 2:1 AV conduction. In AFib, the ventricular rate is unpredictable and irregular.
ECG Appearance and Sawtooth Patterns
The ECG is a key tool for diagnosing AFib and Atrial Flutter. AFib lacks distinct P waves and has an irregular ventricular rhythm. Atrial Flutter, on the other hand, shows “sawtooth” or “flutter” waves, visible in the inferior leads (II, III, aVF).
The sawtooth pattern in Atrial Flutter comes from continuous electrical activity in the right atrium. This pattern is best seen in lead II and V1.
| Characteristics | Atrial Fibrillation (AFib) | Atrial Flutter |
| Electrical Activity | Irregular, chaotic | Regular, organized circuit |
| Heart Rate | Highly variable | More consistent, based on AV conduction |
| ECG Appearance | No distinct P waves, irregularly irregular | Sawtooth pattern, particular in inferior leads |
Symptoms: How They Feel Different
AFib and atrial flutter can make people feel quite different. Both can cause discomfort, but knowing the specific symptoms helps manage them better.
Common Symptoms in Both Conditions
Both AFib and atrial flutter can cause palpitations, dizziness, and shortness of breath. These happen because of the irregular heartbeats in both conditions.
Unique Symptom Patterns
AFib often leads to an irregular pulse, which can be very noticeable. Atrial flutter, on the other hand, usually has a more regular pulse. This difference can affect how patients feel about their condition.
To show the differences in symptoms between AFib and atrial flutter, here’s a table:
| Symptom | AFib | Atrial Flutter |
| Palpitations | Irregular, often described as “quivering” | Regular or mildly irregular, may feel more “organized” |
| Dizziness | Common due to irregular ventricular response | Can occur, specially if ventricular rate is high |
| Shortness of Breath | Frequent, due to inefficient heart function | Possible, specially with exertion |
When Symptoms Require Emergency Care
It’s important for patients to know when to seek emergency care. Severe chest pain, trouble breathing, or severe dizziness are signs to go to the hospital right away.
We suggest that patients get help immediately if they experience:
- Severe chest pain or pressure
- Severe trouble breathing
- Fainting or near-fainting spells
- Rapid or irregular heartbeat that doesn’t improve with medication
Diagnosis: How Doctors Tell Them Apart
Understanding the differences between AFib and Atrial Flutter starts with accurate diagnosis. Doctors use advanced medical techniques for this. They combine clinical evaluation with specialized tests.
ECG Findings and Interpretation
The electrocardiogram (ECG) is key in diagnosing both Atrial Fibrillation and Atrial Flutter. It shows the heart’s electrical activity.
- AFib ECG Characteristics: The ECG shows an irregular rhythm with no distinct P waves.
- Atrial Flutter ECG Characteristics: It displays a regular or irregular rhythm with “sawtooth” or “flutter” waves. These are seen in leads II, III, and aVF.
Additional Diagnostic Tests
While the ECG is essential, more tests might be needed. They help assess heart disease and guide treatment.
- Echocardiogram to check heart structure and function.
- Stress test to see how the heart works under stress.
- Blood tests to find thyroid disorders or other conditions that might cause AFib or Atrial Flutter.
Challenges in Diagnosis
It can be hard to tell AFib and Atrial Flutter apart. This is because of variations in how they present and other heart conditions.
To overcome these challenges, doctors might use long ECG monitoring. They also use other advanced techniques to study the arrhythmia.
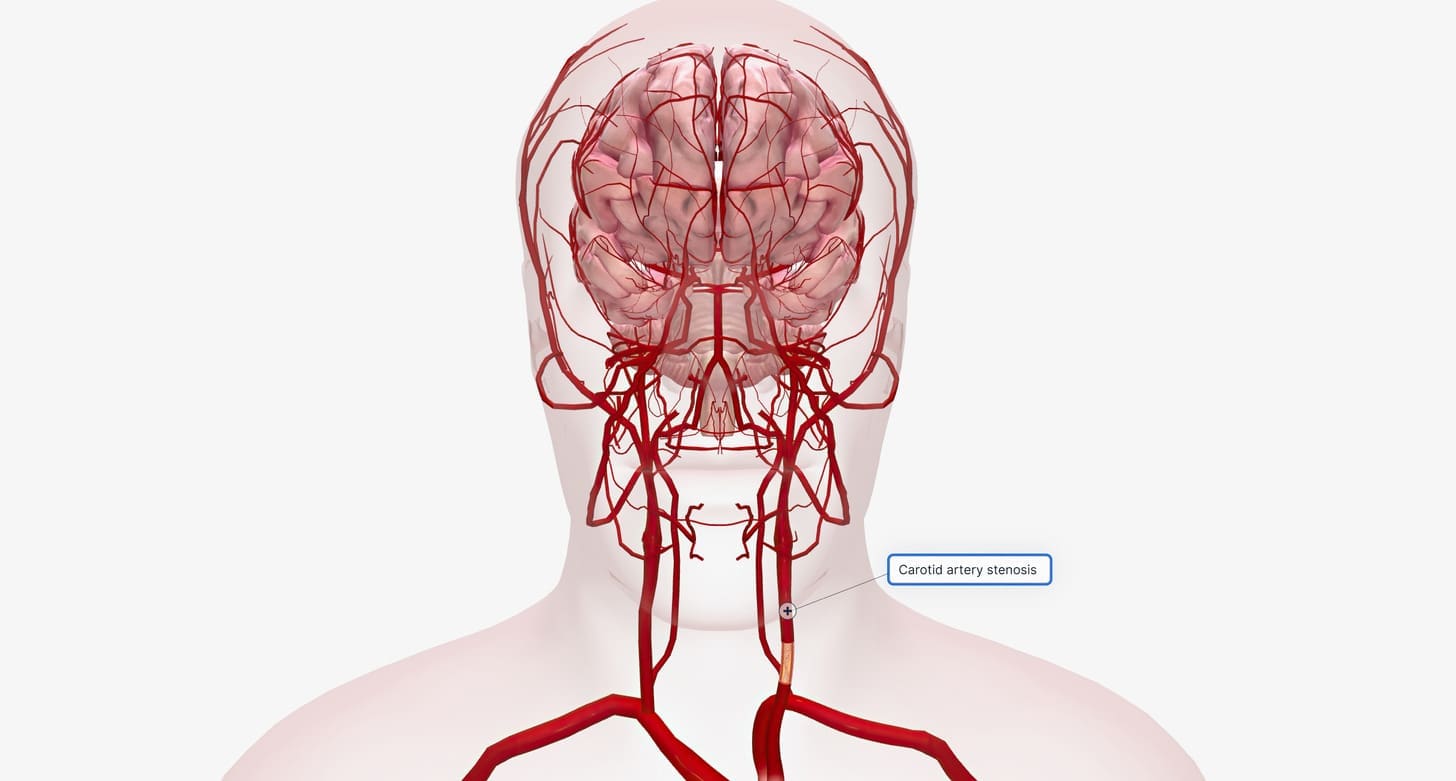
Stroke Risk: Understanding the Dangers
People with AFib or atrial flutter face a big risk of stroke. These heart rhythm problems can cause blood clots in the heart. These clots can then go to the brain, leading to a stroke. It’s important to know this risk to manage and prevent it.
Why Atrial Arrhythmias Increase Stroke Risk
Atrial fibrillation (AFib) and atrial flutter raise stroke risk because of their irregular heartbeats. AFib’s irregular beats cause blood to pool and clot. Atrial flutter, though less risky, can also lead to clot formation.
Key factors that contribute to the increased stroke risk include:
- Irregular heart rhythms leading to blood stasis
- Formation of blood clots in the atria
- Potential for these clots to embolize to the brain
Comparing Risk Levels Between AFib and Flutter
AFib is generally more risky for stroke than atrial flutter. Research shows AFib raises stroke risk by a lot. But, atrial flutter also poses a significant risk and should not be ignored.
“The risk of stroke in patients with atrial fibrillation is approximately 5% per year, which is two to seven times the rate in those without this arrhythmia.”
Current Risk Assessment Tools
Healthcare uses tools to assess stroke risk. The CHA2DS2-VASc score is a key tool. It looks at heart failure, high blood pressure, age, diabetes, stroke history, and more.
Using these tools helps create personalized treatment plans. This can greatly lower stroke risk for those with AFib and atrial flutter.
Treatment Approaches for Atrial Fibrillation
Treating atrial fibrillation (AFib) is complex. It involves several approaches, like rate and rhythm control. We will explore these strategies and the various interventions available to manage AFib effectively.
Rate Control vs. Rhythm Control Strategies
When treating AFib, clinicians often debate between rate control and rhythm control strategies. Rate control focuses on slowing the heart rate to alleviate symptoms. Rhythm control aims to restore a normal sinus rhythm. The choice between these approaches depends on the patient’s symptoms, medical history, and preferences.
“The decision to pursue rate or rhythm control should be individualized, taking into account the patient’s quality of life and risk factors for stroke,” as emphasized in recent clinical guidelines.
Medication Options
Medications play a key role in managing AFib. For rate control, beta-blockers and calcium channel blockers are commonly used. In contrast, rhythm control often involves antiarrhythmic drugs such as amiodarone or sotalol. The choice of medication depends on the patient’s underlying health conditions and the specific characteristics of their AFib.
It’s essential to note that while medications can effectively manage symptoms, they also carry possible side effects. For instance, long-term use of amiodarone can lead to thyroid dysfunction or pulmonary toxicity.
Cardioversion Procedures
Cardioversion is a procedure that involves delivering a controlled electric shock to the heart to restore a normal rhythm. This approach is often used for patients with persistent AFib who have not responded to medication or as an urgent intervention for those with severe symptoms.
Cardioversion can be highly effective, with success rates varying depending on the duration of AFib and the patient’s overall heart health. It may require anticoagulation therapy to prevent stroke.
Catheter Ablation Techniques
Catheter ablation is a minimally invasive procedure that involves destroying the abnormal electrical pathways in the heart that cause AFib. This technique has gained popularity as a potentially curative treatment for AFib, specially for patients who are symptomatic despite medical therapy.
The success of catheter ablation depends on various factors, including the patient’s AFib type, the presence of underlying heart disease, and the operator’s experience. While it offers a promising solution, it’s not without risks, such as tamponade or pulmonary vein stenosis.
In conclusion, treating AFib requires a tailored approach that considers the individual patient’s needs and circumstances. By understanding the available treatment strategies, we can better manage AFib and improve patient outcomes.
Treatment Approaches for Atrial Flutter
Managing atrial flutter well means knowing the treatment options. This condition is similar to atrial fibrillation. It’s important to pick the right treatment plan.
Medication Strategies
Medicines are key in treating atrial flutter. Rate control medications like beta-blockers help control the heart rate. This improves symptoms and life quality.
Rhythm control medications are used to change the heart rhythm. They help keep the rhythm normal after a procedure.
Cardioversion Success Rates
Cardioversion is a top choice for treating atrial flutter. It has a high success rate in restoring normal heart rhythm. The method uses a controlled electric shock.
Research shows cardioversion works in up to 90% of cases. But, the risk of it happening again is high if the cause isn’t fixed.
Catheter Ablation as a Curative Option
Catheter ablation is a cure for atrial flutter. It’s a minimally invasive method. It uses catheters to destroy the bad electrical pathway in the heart.
Studies show catheter ablation works in over 90% of cases. It’s a good choice for many patients.
Long-term Management Considerations
Managing atrial flutter long-term means treating the arrhythmia and fixing underlying issues. It also means preventing strokes.
| Treatment Approach | Success Rate | Long-term Considerations |
| Medication | Variable | Ongoing medication management, possible side effects |
| Cardioversion | Up to 90% | Risk of recurrence, need for blood thinners |
| Catheter Ablation | Above 90% | Possible need for more procedures, watch for recurrence |
It’s vital for both doctors and patients to understand atrial flutter treatments. Choosing the best treatment depends on the patient’s situation and wishes.
Anticoagulation Therapy: Preventing Strokes
Preventing strokes is key for those with AFib and atrial flutter. Anticoagulation therapy is vital. It helps lower the risk of stroke.
Who Needs Blood Thinners
Not every patient with AFib or atrial flutter needs blood thinners. But, those at high stroke risk do. The choice depends on many factors like age and health history.
We use tools like the CHA2DS2-VASc score to decide. A higher score means blood thinners are more likely to help.
Types of Anticoagulants
There are many anticoagulants, including warfarin and DOACs like dabigatran. The right one depends on the patient’s health and preferences.
DOACs are popular for their ease of use. But, always talk to a doctor before choosing.
Monitoring and Safety Considerations
DOACs need less monitoring than warfarin. But, they’re not risk-free. Regular check-ups are important to watch for bleeding or other issues.
It’s also key to adjust doses based on kidney function. Patient education is vital to understand the risks and benefits.
Latest Research on Stroke Prevention
New studies improve our stroke prevention methods for AFib and atrial flutter. DOACs are shown to be effective in lowering stroke risk. They often have a lower bleeding risk than warfarin.
Research is ongoing to find better ways to prevent strokes. This includes new anticoagulants and targeted treatments.
When Patients Experience Both Conditions
It’s important to understand the link between AFib and atrial flutter, as many patients have both. This makes diagnosis and treatment more complex. We’ll look at how these conditions relate, how they switch, and how to manage both together.
The Relationship Between AFib and Flutter
AFib and atrial flutter often happen together in patients. Research shows they share risk factors and triggers. Having one condition can make getting the other more likely.
Studies find that AFib patients are more likely to get atrial flutter, and vice versa. This shows the need for a full management plan for both conditions.
Transition Patterns Between Arrhythmias
It’s common for patients to switch between AFib and atrial flutter. Knowing how these switches happen is key to managing them well.
Changes in heart rate, electrolyte imbalances, and some medicines can cause these switches. Keeping an eye on these factors helps predict and manage arrhythmia episodes.
Management Strategies for Dual Diagnoses
Dealing with both AFib and atrial flutter needs a custom plan. Treatment often includes controlling heart rate, rhythm, and preventing blood clots.
| Management Strategy | AFib | Atrial Flutter |
| Rate Control | Beta blockers, Calcium channel blockers | Beta blockers, Calcium channel blockers |
| Rhythm Control | Antiarrhythmic medications, Cardioversion | Antiarrhythmic medications, Cardioversion, Catheter Ablation |
| Anticoagulation Therapy | Warfarin, NOACs (e.g., Apixaban, Rivaroxaban) | Warfarin, NOACs (e.g., Apixaban, Rivaroxaban) |
Latest Clinical Protocols
New guidelines focus on personalized treatment for AFib and atrial flutter. They stress assessing stroke risk, choosing the right blood thinner, and considering catheter ablation for some patients.
There’s a move towards treating both conditions together. This integrated approach aims to better patient outcomes and lower complication risks.
Conclusion
It’s key to know the differences between atrial fibrillation (AFib) and atrial flutter. This knowledge helps in giving the best care to those with heart rhythm issues. We’ve looked at how these two conditions are different, including their electrical patterns, symptoms, and how to treat them.
Knowing the difference between AFib and atrial flutter is important. It helps doctors make better treatment plans for each patient. This can lead to better health outcomes and lower the chance of serious problems like stroke.
The main differences between AFib and atrial flutter are in how the heart beats and looks on an ECG. Getting the right diagnosis is critical. It helps doctors choose the best treatment, like controlling the heart rate or using medicines to restore a normal rhythm.
Understanding AFib and atrial flutter helps us care for patients better. This improves their lives and reduces the strain on healthcare systems.
FAQ
What is the main difference between atrial fibrillation (AFib) and atrial flutter?
AFib has a chaotic, irregular rhythm. Atrial flutter, on the other hand, has a more organized rhythm.
Is atrial flutter the same as AFib?
No, they are not the same. Atrial flutter has a predictable pattern, unlike AFib’s irregular rhythm.
What’s the difference between AFib and atrial flutter in terms of symptoms?
Both can cause palpitations and shortness of breath. But atrial flutter’s regular rhythm might make symptoms feel more predictable.
How do doctors diagnose AFib versus atrial flutter?
Doctors use electrocardiograms (ECGs) for diagnosis. AFib shows an irregular rhythm. Atrial flutter has a sawtooth pattern on the ECG.
Are the treatment approaches different for AFib and atrial flutter?
Yes, treatments vary. Both can use medications, cardioversion, and catheter ablation. The approach depends on the condition and patient’s health.
Do patients with atrial flutter have the same stroke risk as those with AFib?
Both increase stroke risk, but atrial flutter’s risk is generally lower. Risk assessment tools help manage this risk.
Can a patient have both AFib and atrial flutter?
Yes, it’s possible. Managing both conditions can be complex. Treatment plans are tailored to the individual.
What is the role of anticoagulation therapy in AFib and atrial flutter?
Anticoagulation therapy prevents strokes in both conditions. The decision to use blood thinners depends on stroke risk factors.
How do lifestyle factors influence the risk of developing AFib or atrial flutter?
Lifestyle factors like alcohol, obesity, and lack of activity increase risk. These factors apply to both conditions.
Are there any new developments in the treatment of AFib and atrial flutter?
Yes, research is evolving treatment options. Advances include better catheter ablation and anticoagulation therapies.
Reference:
Kirchhof, P., Benussi, S., Kotecha, D., Ahlsson, A., Atar, D., Casadei, B., … & Vardas, P. (2016). 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. European Heart Journal, 37(38), 2893–2962. https://www.ncbi.nlm.nih.gov/pubmed/27567408