Last Updated on November 25, 2025 by Ugurkan Demir
Restoring normal heart rhythm is key for managing atrial fibrillation. This condition affects about 10.55 million adults in the US.
At Liv Hospital, we follow international standards for treating AF. We focus on patient care above all.
We aim to give full care to our patients. Our care is based on the newest cardioversion guidelines for atrial fibrillation. We work to bring back the heart’s natural rhythm and keep our patients safe.
Atrial fibrillation (AFib) is a complex heart rhythm problem. It affects patients a lot, so we need to understand it well. We’ll look into what AFib is, its symptoms, how it affects the heart, and why we try to fix the rhythm.
Atrial fibrillation makes the heart beat fast and irregularly. This happens because of chaotic electrical activity in the atria. This chaos makes the atria not work well, leading to less blood being pumped out.
The reasons behind AFib are complex. They involve changes in how the heart’s electrical system works and its structure. Electrical remodeling makes it harder for the heart to go back to normal. Structural remodeling changes the heart’s shape, making AFib harder to stop.
AFib symptoms vary. Some people don’t feel anything, while others have palpitations, shortness of breath, chest pain, fatigue, and trouble exercising. The heart’s ability to pump blood is also affected.
The symptoms of AFib can really hurt a person’s quality of life. Palpitations and dyspnea are common. They show how the heart’s rhythm is off and how it might not pump well. This can be a big problem, even more so for those with heart disease.
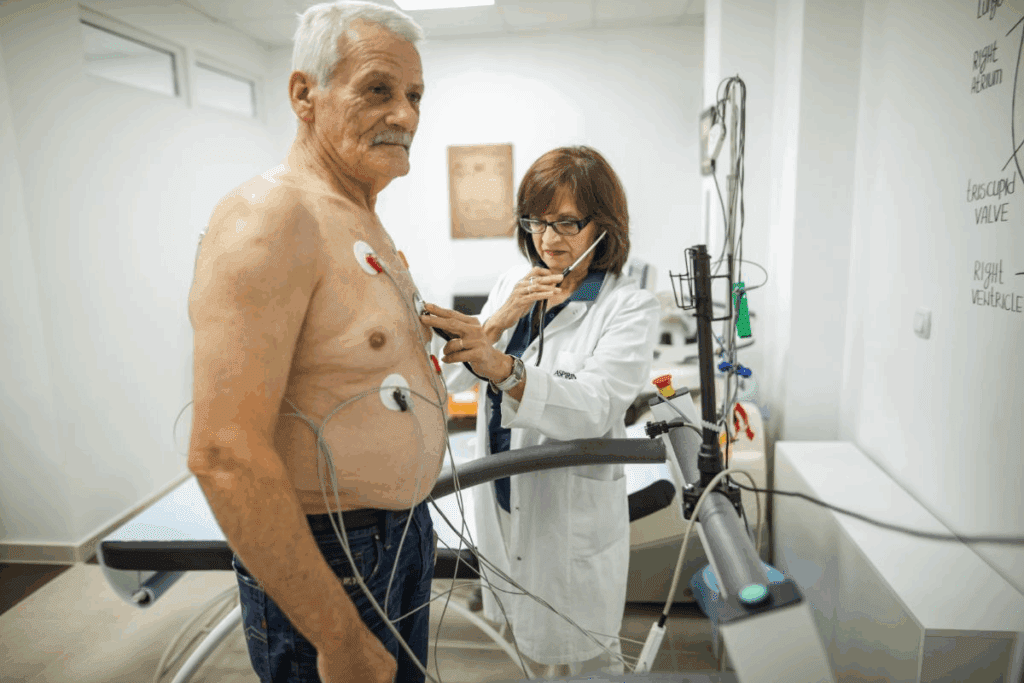
Getting the heart back to a normal rhythm is a main goal for AFib patients. This is very important for those who feel bad or whose heart isn’t working right. Cardioversion is a key treatment to achieve this.
Deciding to do cardioversion depends on several things. These include how long the AFib has lasted, if the patient is feeling symptoms, and their overall health. Cardioversion can be done in two ways: electrically or with medicine. The choice depends on the patient’s situation and what they prefer.
Atrial fibrillation cardioversion is a key treatment for patients with this heart rhythm problem. It aims to bring the heart back to its normal rhythm. This procedure is used to fix an abnormal heart rhythm.
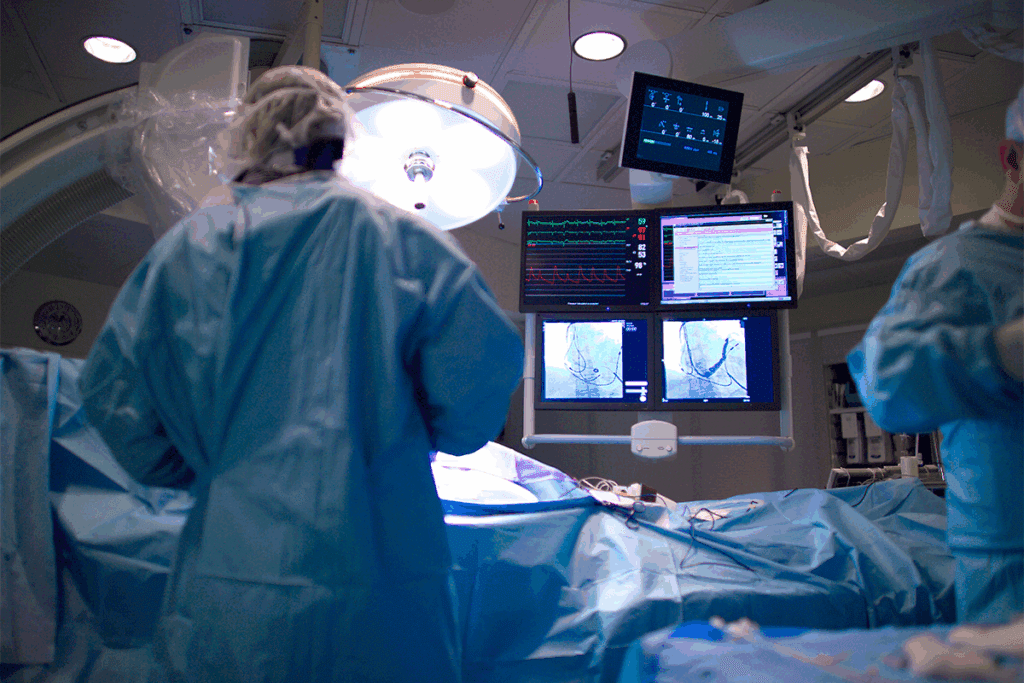
Cardioversion uses electrical or pharmacological methods to fix the heart rhythm. Electrical cardioversion uses a shock to the heart. Pharmacological cardioversion uses medicines to achieve the same goal.
We will look into these methods, their success rates, and what affects them.
Electrical cardioversion, or DCCV, uses a shock to the heart to fix the rhythm. It’s very effective for quick rhythm restoration.
Pharmacological cardioversion uses medicines to fix the rhythm. It’s good for patients not suited for electrical cardioversion or as extra help.
| Method | Efficacy | Advantages | Disadvantages |
| Electrical Cardioversion (DCCV) | High immediate efficacy | Rapid restoration of sinus rhythm, effective for acute management | Requires sedation or anesthesia, risk of complications |
| Pharmacological Cardioversion | Variable efficacy depending on the drug and patient factors | Non-invasive, can be used for long-term management | Potential side effects, may not be as effective for all patients |
The success of cardioversion depends on many things. These include how long the patient has had atrial fibrillation, any heart disease, and other health issues.
Efficacy rates for electrical cardioversion are usually higher, but it’s best to choose based on the patient’s needs and wishes.
Knowing about these factors and cardioversion methods is key for doctors. It helps them make the best choices for their patients.
It’s key to know the latest guidelines for Afib cardioversion to manage patients well. These guidelines help us make sure our cardioversion methods are safe and work.
The American Heart Association (AHA), American College of Cardiology (ACC), and Heart Rhythm Society (HRS) have set out detailed guidelines for managing atrial fibrillation. They stress the need to check stroke risk and ensure proper anticoagulation before cardioversion.
Anticoagulation therapy is vital in managing Afib, more so when thinking about cardioversion. The guidelines suggest patients with AFib should be on anticoagulation for at least three weeks before cardioversion, unless there’s a reason not to.
| Guideline Component | Recommendation |
| Anticoagulation Therapy | At least 3 weeks before cardioversion |
| Stroke Risk Assessment | CHA2DS2-VASc score recommended |
| Cardioversion Approach | Electrical or pharmacological |
The European Society of Cardiology (ESC) also has guidelines for managing atrial fibrillation, including cardioversion. While similar to the AHA/ACC/HRS guidelines, there are some differences in approach and focus.
The ESC guidelines emphasize a patient-centered approach. They suggest considering the patient’s unique characteristics and preferences when deciding on cardioversion.
When thinking about cardioversion for a patient with AFib, a detailed risk-benefit assessment is critical. This involves weighing the benefits, like better symptoms and quality of life, against the risks, like stroke and complications from the procedure.
We use a structured framework to evaluate these factors. We look at the patient’s stroke risk, how long they’ve had AFib, and any heart disease they might have.
Cardioversion is a key treatment for atrial fibrillation (Afib) patients. It’s important for doctors to know when to use it. We’ll cover the 7 main reasons for cardioversion in Afib.
These reasons include when patients are unstable, have persistent symptoms, or don’t respond to other treatments. Cardioversion helps bring back a normal heart rhythm in Afib patients.
Doctors must carefully consider each patient’s situation before choosing cardioversion. Knowing the right time to use it helps ensure the best care for Afib patients. This approach improves their quality of life.
The main aim of cardioversion is to convert Afib to a normal rhythm. Understanding when to use it is key. Doctors follow guidelines and consider each patient’s needs to make the right choice.
Atrial fibrillation cardioversion is a procedure to fix an irregular heartbeat. It uses electrical or medicine methods to get the heart back to normal. This improves heart function and lowers stroke risk.
We do cardioversion for patients with bad symptoms or fast heart rates. It’s also for those at risk of heart failure. The main reasons include severe symptoms, unstable heart, or not responding to medicine.
Electrical cardioversion uses a shock to fix the heartbeat. Pharmacological cardioversion uses medicine. We pick the best method based on the patient’s health and the reason for the irregular heartbeat.
The American Heart Association and others have guidelines for this procedure. These guidelines help us manage atrial fibrillation, including when to use cardioversion.
We look at several factors to decide if cardioversion is right. These include stroke risk, bleeding risk, and heart conditions. This helps us choose the best treatment for each patient.
Anticoagulation therapy is key to prevent stroke and blood clots. We start it before the procedure and keep it going for a few weeks after.
Yes, some patients can have cardioversion as an outpatient. We check each patient’s health and history to decide the best place for the procedure.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!