
It’s important to know the difference between atrial tachycardia and atrial fibrillation for the right treatment. At Liv Hospital, we use the latest methods to treat these fast heart rhythms from the atria.
Compare atrial tachycardia vs atrial fibrillation in ECG and clinical presentation.
Atrial tachycardia shows a fast heart rate. On the other hand, atrial fibrillation has an irregular and fast heart rhythm.
We focus on accurate diagnosis and treatment. Our care is centered on the patient, using top international practices for the best results.
Key Takeaways
- Atrial tachycardia and atrial fibrillation are different arrhythmias with unique ECG signs.
- Getting the right diagnosis is key for effective treatment.
- Liv Hospital uses evidence-based methods for heart rhythm disorders.
- Our main goal is patient-centered care, providing full support.
- It’s essential to understand the clinical effects of these conditions.
Understanding Atrial Arrhythmias: The Basics
It’s important to know the basics of atrial arrhythmias to diagnose and treat heart rhythm disorders. Atrial arrhythmias, like atrial tachycardia and atrial fibrillation, make the heart’s upper chambers beat irregularly. They can beat too quickly or too slowly.
The Normal Cardiac Conduction System
The heart’s electrical system controls the heartbeat. It starts with the sinoatrial (SA) node, the heart’s natural pacemaker. This node sends electrical impulses to the atria, making them contract.
The impulse then goes to the atrioventricular (AV) node. This node delays the signal before it reaches the ventricles. This ensures the heartbeat is coordinated.
The normal heart rate changes with age. Physical activity, stress, and some medications can also affect it. For example, sinus tachycardia is a normal increase in heart rate due to activity or stress.
What Happens When Atrial Rhythm Goes Awry
When the atrial rhythm becomes abnormal, it can cause arrhythmias like atrial tachycardia or atrial fibrillation. Atrial tachycardia is a rapid, regular atrial rate, often caused by an abnormal electrical focus in the atria.
Atrial fibrillation, on the other hand, is a rapid, irregular atrial rate. It’s caused by multiple disorganized electrical impulses.
“Atrial fibrillation is the most common sustained cardiac arrhythmia, affecting millions of people worldwide.”
Epidemiology and Clinical Significance
Atrial arrhythmias are a big public health concern. They’re common and can lead to serious complications. Atrial fibrillation, in particular, raises the risk of stroke, heart failure, and death.
| Arrhythmia Type | Prevalence | Clinical Significance |
| Atrial Tachycardia | Less common than atrial fibrillation | Can cause palpitations, shortness of breath |
| Atrial Fibrillation | Affects millions worldwide | Increases risk of stroke, heart failure |
Understanding atrial arrhythmias is key for healthcare providers. It helps them manage these conditions well and improve patient outcomes.
Atrial Tachycardia: Definition and Mechanisms
To understand atrial tachycardia, we need to know its definition, how it works, and what makes it different. It’s a condition where the heart beats too fast, over 100 times a minute. This is seen on an electrocardiogram (ECG) as a regular pattern with a specific P wave.
Pathophysiology of Atrial Tachycardia
Atrial tachycardia happens when the heart’s electrical system gets out of sync. This can be caused by several things. Enhanced automaticity means the heart cells beat too fast. Triggered activity happens when there are extra electrical signals during or after the heart’s rest period.
When atrial tachycardia occurs, the heart rate might speed up and then slow down. This pattern is a key sign of the condition.
Common Causes and Triggers
Many things can lead to atrial tachycardia. Heart problems, imbalances in electrolytes, and some medicines are common causes. Triggers can include stress, caffeine, or other stimulants.
- Structural heart diseases such as cardiomyopathy or valvular disease
- Electrolyte imbalances, like potassium and magnesium issues
- Medications like beta-agonists or antiarrhythmic drugs
Types of Atrial Tachycardia
Atrial tachycardia can be divided into types based on its cause and how it works. The main types are focal, multifocal, and re-entrant atrial tachycardia. Each type has its own signs and treatment options.
Focal atrial tachycardia starts from one spot in the heart. Multifocal atrial tachycardia has multiple starting points. Re-entrant atrial tachycardia involves a loop of electrical activity in the heart.
Atrial Fibrillation: Definition and Mechanisms
Atrial fibrillation is a heart rhythm disorder that is very common. It makes the heart beat irregularly and chaotically. This condition is a big challenge for doctors and puts a lot of strain on healthcare systems.
Pathophysiology of Atrial Fibrillation
The heart’s upper chambers change a lot in atrial fibrillation. These changes include electrical and structural remodeling, and problems with how the heart contracts. These changes help start and keep atrial fibrillation going.
Key factors contributing to the pathophysiology include:
- Atrial enlargement and fibrosis
- Inflammation and oxidative stress
- Electrical remodeling due to chronic arrhythmia
Common Causes and Risk Factors
Atrial fibrillation is linked to many conditions and risk factors. Knowing these is key to preventing and treating it.
| Cause/Risk Factor | Description | Clinical Significance |
| Hypertension | High blood pressure | Increases atrial pressure and promotes remodeling |
| Heart Failure | Reduced cardiac output | Contributes to atrial enlargement and fibrosis |
| Coronary Artery Disease | Reduced blood flow to the heart | May lead to ischemia and arrhythmia |
Prevalence and Impact in the United States
Atrial fibrillation is a big health problem in the United States. It was estimated to affect 5.2 million people in 2010. By 2030, this number is expected to rise to 12.1 million. This means we need better ways to spot, treat, and manage it.
This condition does more than just affect the heart’s rhythm. It also raises the risk of stroke, heart failure, and other heart problems. If we manage it well, we can lower these risks and help patients live better lives.
Atrial Tachycardia vs Atrial Fibrillation: 7 Key Differences
Understanding the differences between atrial tachycardia and atrial fibrillation is key. These differences are seen in electrocardiographic (ECG) characteristics. Accurate diagnosis and effective management depend on these differences.
Difference #1: ECG P Wave Morphology
Atrial tachycardia shows distinct P waves on ECG. These P waves have a consistent shape, showing the arrhythmia’s focal origin. On the other hand, atrial fibrillation has no clear P waves. Instead, it shows fine or coarse fibrillatory waves.
Difference #2: Rhythm Regularity
The rhythm’s regularity is another key difference. Atrial tachycardia has a regular rhythm. Atrial fibrillation, though, has an irregularly irregular rhythm. This irregularity in atrial fibrillation comes from chaotic atrial activity and variable AV nodal conduction.
Difference #3: Ventricular Response Pattern
The ventricular response pattern also differs. In atrial tachycardia, the ventricular response is regular. It’s tied to the atrial rate through a consistent AV conduction ratio. In atrial fibrillation, the ventricular response is irregularly irregular. This shows the unpredictable AV nodal conduction of the fibrillatory impulses.
Difference #4: Heart Rate Range
Both conditions can have a range of heart rates. But, the rhythm’s characteristics help tell them apart. Atrial tachycardia often has a narrow complex tachycardia. Atrial fibrillation can also have a rapid ventricular response. But, the irregularity and lack of P waves are key differences.
| Characteristic | Atrial Tachycardia | Atrial Fibrillation |
| P Wave Morphology | Distinct P waves with consistent morphology | Absence of discernible P waves; fibrillatory waves |
| Rhythm Regularity | Regular | Irregularly irregular |
| Ventricular Response | Regular; related to atrial rate through consistent AV conduction | Irregularly irregular; unpredictable AV nodal conduction |
| Heart Rate Range | Variable; often narrow complex unless aberrancy or pre-existing bundle branch block | Variable; can be rapid with irregular ventricular response |
Understanding these differences helps healthcare providers make accurate diagnoses. They can then develop the right treatment plans for patients with atrial tachycardia or atrial fibrillation.
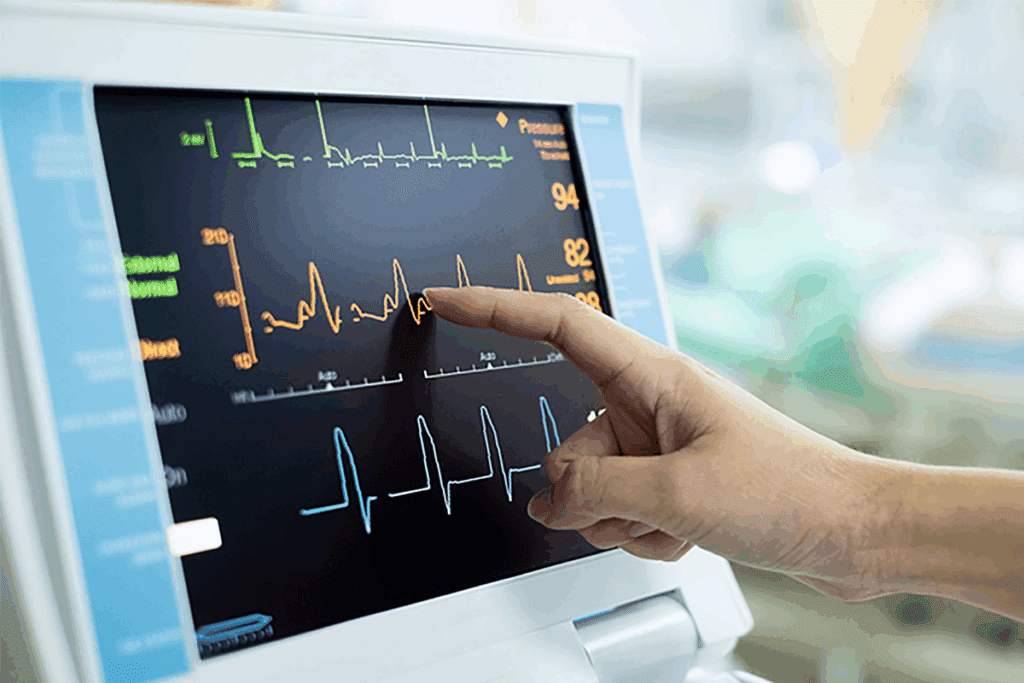
ECG Interpretation: Identifying Atrial Arrhythmias
Reading ECGs correctly is key to spotting atrial arrhythmias. It needs both technical skills and a deep understanding of the heart’s rhythm. ECGs give us vital info to tell different heart conditions apart.
When we look at ECGs for atrial arrhythmias, we focus on certain signs. These signs help us tell one condition from another. We look at the P wave shape, rhythm regularity, and how the ventricles respond.
Characteristic ECG Findings in Atrial Tachycardia
Atrial tachycardia shows a unique P wave shape and a heart rate of 100 to 250 beats per minute. The P wave’s direction and shape can hint at where the tachycardia starts. For example, a negative P wave in the inferior leads might suggest a low atrial origin.
Key ECG features of atrial tachycardia include:
- A consistent P wave morphology
- A regular atrial rhythm
- A ventricular response that may be regular or irregular, depending on the presence of AV block
Characteristic ECG Findings in Atrial Fibrillation
Atrial fibrillation, on the other hand, lacks clear P waves and has an irregular heart rhythm. The atrial fibrillatory waves look chaotic and vary in size and speed on the ECG.
The hallmark ECG features of atrial fibrillation include:
- Absence of P waves
- Irregularly irregular ventricular rhythm
- Fibrillatory waves that vary in amplitude and frequency
Common ECG Misinterpretations
ECGs are very useful, but mistakes can happen. We might confuse artifacts with atrial fibrillation or mix up atrial flutter with atrial tachycardia. Paying close attention to the ECG and matching it with the patient’s symptoms can help avoid these mistakes.
To avoid mistakes, we must think about the patient’s overall situation and match ECG findings with other tests. This way, we can make more accurate diagnoses and choose the right treatment.
Sinus Tachycardia vs Atrial Tachycardia: Critical Distinctions
It’s important to tell the difference between sinus tachycardia and atrial tachycardia. Both have a fast heart rate, but they have different causes and effects on the body.
Physiologic vs Pathologic Tachycardia
Sinus tachycardia is a normal response to stress, fever, or hard work. It has a regular rhythm and looks normal on an ECG. Atrial tachycardia, though, is caused by problems in the heart’s upper chambers.
Key characteristics of sinus tachycardia include:
- Normal P wave axis
- Gradual onset and offset
- Response to autonomic maneuvers
Atrial tachycardia has different P wave shapes and doesn’t always respond to stress or relaxation.
ECG Differences Between Sinus and Atrial Tachycardia
The ECG is key in telling these two apart. Key ECG differences are shown in the table below:
| ECG Feature | Sinus Tachycardia | Atrial Tachycardia |
| P Wave Morphology | Normal, upright in lead II | Abnormal, may be inverted or biphasic |
| P Wave Axis | Normal (0° to +90°) | Abnormal, variable |
| Onset/Offset | Gradual | Sudden |
As shown, sinus tachycardia has normal P waves, while atrial tachycardia has abnormal ones.
Clinical Context in Differentiation
When figuring out if it’s sinus or atrial tachycardia, the patient’s story matters a lot. Symptoms, past health, and how they react to treatment are clues.
“The clinical presentation of atrial tachycardia can vary widely, from asymptomatic to severe hemodynamic compromise, necessitating a nuanced approach to diagnosis and management.” –
Cardiology Expert
By looking at ECGs and the patient’s story, doctors can make better diagnoses and treatment plans for tachycardia.
Clinical Implications and Management Strategies
Atrial tachycardia and atrial fibrillation are different challenges that need specific care plans. It’s key to understand these conditions to help patients well.
Acute Management of Atrial Tachycardia
For atrial tachycardia, the goal is to control the heart rate and get it back to normal rhythm. Vagal maneuvers and adenosine are first steps. If these don’t work, electrical cardioversion might be needed.
Here’s what we suggest for quick treatment:
- First, check if the patient is stable
- Try vagal maneuvers or adenosine
- If those don’t work, think about electrical cardioversion
Acute Management of Atrial Fibrillation
Managing atrial fibrillation means stopping strokes and trying to get the heart back to normal. Doctors often use anticoagulants to prevent strokes. The right choice depends on the patient.
| Management Strategy | Description |
| Rate Control | Use beta-blockers or calcium channel blockers to control heart rate |
| Rhythm Control | Try to get the heart back to normal with drugs or cardioversion |
| Anticoagulation | Use anticoagulants to prevent strokes |
Long-term Treatment Considerations
For both conditions, long-term care includes lifestyle changes, medicines, and sometimes procedures. Catheter ablation is an option for those with ongoing issues.
When planning long-term care, we look at:
- Patient health and what they want
- The type and how often the arrhythmia happens
- How well they’ve done with past treatments
Diagnostic Challenges and Modern Approaches
Diagnosing atrial arrhythmias is tough because they are complex and show up in many ways. Getting it right is key for the best care. It helps decide how to treat and manage the condition.
New tech has made diagnosing and managing atrial arrhythmias better. We now use advanced ECGs, ambulatory monitoring, and electrophysiology studies.
Advanced ECG Technologies
New ECG tech gives us more detailed info on heart rhythms. High-resolution ECG and ECG signal averaging help spot small patterns missed by regular ECGs.
These tools help doctors better detect atrial arrhythmias. This leads to better care for patients.
Ambulatory Monitoring Options
Ambulatory monitoring is key for diagnosing atrial arrhythmias. It lets us watch heart rhythms over time. Holter monitors and event recorders give us data on heart rhythm during daily life.
This data helps catch arrhythmias that a regular ECG might miss.
Electrophysiology Studies
Electrophysiology studies (EPS) are detailed tests that map the heart’s electrical activity. They’re great for finding out what causes atrial tachycardia and fibrillation. This info helps doctors plan the best treatment.
Understanding the heart’s electrical activity helps doctors tailor treatments to each patient.
Impact of Correct Diagnosis on Patient Outcomes
Getting the diagnosis right is critical for patient outcomes. It helps choose the best treatment. Accurate diagnosis means patients get the care they need, whether it’s medicine, catheter ablation, or other treatments.
Correct diagnosis not only improves health but also quality of life for those with atrial arrhythmias.
Conclusion
Getting the right diagnosis and treatment for atrial arrhythmias is key to better patient care. We’ve looked at the main differences between atrial tachycardia and atrial fibrillation. This includes their unique ECG signs and what they mean for patients.
It’s important to know how these conditions work and their causes. This knowledge helps doctors create the best treatment plans for each patient. By understanding these differences, doctors can give more focused care.
Managing atrial tachycardia and atrial fibrillation well means using a mix of treatments. This includes medicines and other methods. With a deep understanding of these conditions, we can make patient care even better.
FAQ
What is the main difference between atrial tachycardia and atrial fibrillation?
Atrial tachycardia has a fast, regular heart rhythm. Atrial fibrillation, on the other hand, has an irregular and chaotic rhythm.
How do I differentiate between atrial tachycardia and sinus tachycardia on an ECG?
Atrial tachycardia shows abnormal P waves and starts suddenly. Sinus tachycardia has normal P waves and starts slowly.
What are the common causes of atrial tachycardia?
Atrial tachycardia can be caused by heart problems, imbalances in electrolytes, and some medications.
How is atrial fibrillation diagnosed on an ECG?
Atrial fibrillation is diagnosed by an ECG showing an irregular heart rhythm. It also shows no clear P waves and chaotic activity in the atria.
What is the difference between atrial tachycardia and supraventricular tachycardia?
Atrial tachycardia is a type of supraventricular tachycardia that starts in the atria. Supraventricular tachycardia is a broader term for tachycardias starting above the ventricles.
How do I manage atrial tachycardia and atrial fibrillation in the acute setting?
In the acute setting, managing these conditions involves controlling the heart rate. It also means converting the arrhythmia to a normal rhythm and treating the underlying causes.
What are the long-term treatment considerations for atrial tachycardia and atrial fibrillation?
Long-term treatment includes using medications to prevent blood clots and maintain a normal heart rhythm. It may also involve procedures like catheter ablation.
How do advanced ECG technologies aid in the diagnosis of atrial arrhythmias?
Advanced ECG technologies like ambulatory monitoring and electrophysiology studies help diagnose atrial arrhythmias. They provide detailed information and prolonged monitoring.
What is the impact of correct diagnosis on patient outcomes in atrial arrhythmias?
Correctly diagnosing atrial arrhythmias is key to guiding the right treatment. It improves patient outcomes, reducing the risk of stroke and other complications.
References:
- Johnson, L. S. B. (2015). A prospective study of supraventricular activity and atrial fibrillation incidence. Heart Rhythm O2. https://www.sciencedirect.com/science/article/abs/pii/S1547527115005524
- L Patti. (2023). Supraventricular tachycardia. In StatPearls . https://www.ncbi.nlm.nih.gov/books/NBK441972/





